@CDCgov needs to harmonize/update all websites on spread of COVID-19
1 updated page has clear &(nearly) accurate information:
cdc.gov/coronavirus/20…
(here's detailed thread on update:
Many other CDC pages still focus on wrong mechanisms of spread
Thread
1 updated page has clear &(nearly) accurate information:
cdc.gov/coronavirus/20…
(here's detailed thread on update:
https://twitter.com/DiseaseEcology/status/1313193505276133376)
Many other CDC pages still focus on wrong mechanisms of spread
Thread
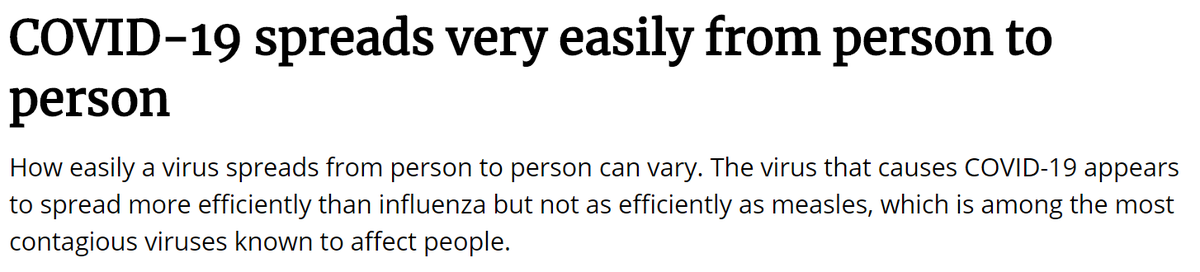
Updated page is clear about #1 mechanism of spread:
close (<6') contact
It also makes it clear that further >6' spread is possible
("airborne transmission") & when this occurs (indoors, poor ventilation)
Perhaps most importantly it accurately tells people how to be safe.
close (<6') contact
It also makes it clear that further >6' spread is possible
("airborne transmission") & when this occurs (indoors, poor ventilation)
Perhaps most importantly it accurately tells people how to be safe.

Relative ranking isn't completely right, but pretty good (still too much focus on surfaces, hand washing). For far more details on update see:
https://twitter.com/DiseaseEcology/status/1313193505276133376
Unfortunately if you google "cdc how is corona spread" you get these pages:
cdc.gov/coronavirus/20…
cdc.gov/coronavirus/20…
Neither of these link to the updated webpage (cdc.gov/coronavirus/20…). The 1st of these pages (Spread faq) is ok... (cont)
cdc.gov/coronavirus/20…
cdc.gov/coronavirus/20…
Neither of these link to the updated webpage (cdc.gov/coronavirus/20…). The 1st of these pages (Spread faq) is ok... (cont)
It gets the #1 mechanism right, but overemphasizes surface transmission that is still very rare (including NZ trash lid). It mentions aerosols & >6' which is great but it'd be better to just link to updated page w/ fuller explanation. 

Unfortunately on this same faq page the link for "How can I protect myself" goes to this page:
cdc.gov/coronavirus/20…
This page is very old & lists #1 thing to do is Wash hands. Ugh. Definitely not top priority. Bad guidance.
cdc.gov/coronavirus/20…
This page is very old & lists #1 thing to do is Wash hands. Ugh. Definitely not top priority. Bad guidance.

Why does this matter? Because many people are still confused about what is most important to keep people safe. So much early focus was on hand washing & surface transmission that public still thinks that is biggest risk, leading to excessive focusing on surface cleaning.
Instead people should be focusing on masks, distance & ventilation (best version is outdoors). Surfaces & hand washing are very distant 4th priority (but still good general practice, of course).
@MackayIM has nice visual of how layers of protection help:
Outside=good. Outside+6'=great. Outside+6'+mask=even better.
1 shortcoming of cheese slices is that they all look equally important. They aren't.
@MackayIM can you revise to clarify this?
https://twitter.com/MackayIM/status/1316716840232448000
Outside=good. Outside+6'=great. Outside+6'+mask=even better.
1 shortcoming of cheese slices is that they all look equally important. They aren't.
@MackayIM can you revise to clarify this?
Main point: CDC should have all websites on how SARS-COV-2 is spread point to their updated page which gives proper focus to each mode of spread & how to be safe. This would help people focus on key issues which is extremely important since it's hard to do everything.
Some restaurants have people standing in lines waiting to be seated for >15 minutes while removing the shared salt and pepper shakers from tables or pulling the dispensable ketchup packets. Same for some stores. This improper focus will lead to infections. Please fix @CDCgov
• • •
Missing some Tweet in this thread? You can try to
force a refresh