
NEW! research shows rapid antigen tests can work in a real world setting - with asymptomatic and symptomatic people. The rapid "paper-strip" antigen test called the BinaxNOW detected >90% of people with high viral loads who are likely to be infectious
nytimes.com/2020/10/15/hea…
1/
nytimes.com/2020/10/15/hea…
1/
I've written about the BinaxNOW from @abbottnews before and why these types of tests can be 'game changers' for our ability to combat this virus
2/
https://twitter.com/michaelmina_lab/status/1298775922510790658?s=20
2/
As expected... the BinaxNOW did NOT detect all PCR positive people... only ~60%
BUT DID detect >90% of those with high/contagious virus load. THESE ARE THE PPL THAT MATTER most when trying to cut off transmission chains.
3/
BUT DID detect >90% of those with high/contagious virus load. THESE ARE THE PPL THAT MATTER most when trying to cut off transmission chains.
3/
If goal is to detect ppl who are likely contagious, PCR can be too sensitive. Many - or MOST PCR positve ppl who are detected through infrequent surveillance testing are no longer infectious by the time they are detected
4/
https://twitter.com/michaelmina_lab/status/1296690611685404672?s=20
4/
This issue that PCR positivity does not equal infectious positivity was also well reported in a recent @nytimes article also by @apoorva_nyc that has really raised awareness of why we MUST consider PCR Ct values.
nytimes.com/2020/08/29/hea…
5/
nytimes.com/2020/08/29/hea…
5/
Back to the new research.. the BinaxNOW rapid test was able to detect most (93%) ppl with high viral loads - consistent with cultural positive/potentially transmissible virus. The BinaxNOW did not capture PCR positive people with low RNA copy numbers unlikely to be contagious
6/
6/
If the goal is to find infectious people, this is OK... or perhaps even better so that we are not isolating people who are no longer infectious. Again, covered in this article. (which admittedly caused some confusion)
nytimes.com/2020/08/29/hea…
7/
nytimes.com/2020/08/29/hea…
7/
Some say "we don't know enough" yet about Ct values & transmission-but we do.
Even forgetting how much we knew PRE-COVID on this issue, numerous #COVID19 studies show strong correlation where high PCR Ct values are culture neg:
ncbi.nlm.nih.gov/pmc/articles/P…
8/
Even forgetting how much we knew PRE-COVID on this issue, numerous #COVID19 studies show strong correlation where high PCR Ct values are culture neg:
ncbi.nlm.nih.gov/pmc/articles/P…
8/
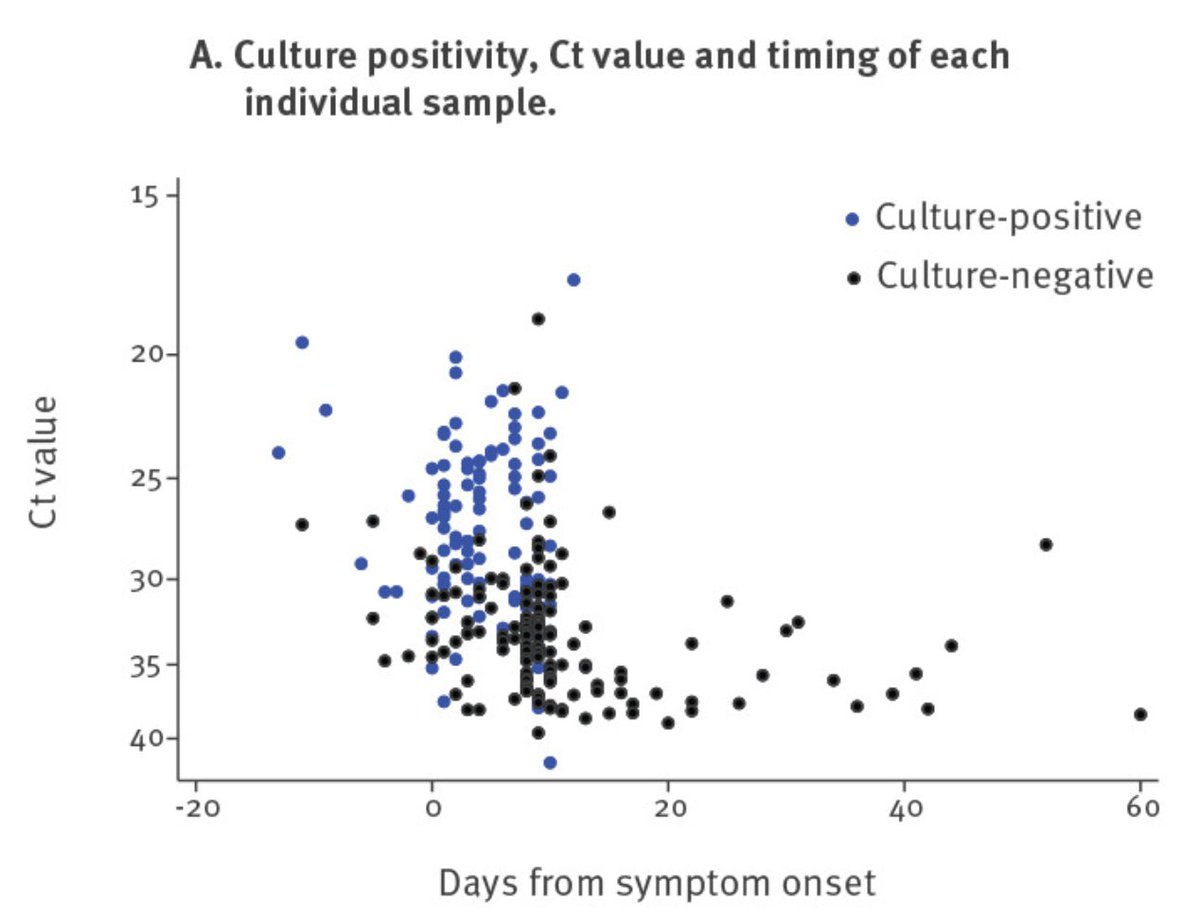
Importantly, the above study also found essentially no culture positive samples >10 days past symptom onset - regardless of Ct value. Rapid antigen tests would mostly be neg at >10 days and thus can be MORE accurate for detecting contagious people than PCR...
9/
9/
This new BinaxNOW data from SF shows that rapid paper strip tests can work very well to detect potentially infectious people, with >90% sensitivity....
Importantly, even when the overall sensitivity against PCR is only 50%!
10/
Importantly, even when the overall sensitivity against PCR is only 50%!
10/
This point cannot be overstated... PCR positivity is not the right benchmark if the goal is detection of infectious people!
Please let us stop using simply PCR "positive/negative" as the benchmark - we CAN be more nuanced.
11/
Please let us stop using simply PCR "positive/negative" as the benchmark - we CAN be more nuanced.
11/
Two additional papers have come out recently that further enforce rapid tests...
One looking at BD rapid test which, like BinaxNOW showed that a rapid test is potentially MORE accurate than PCR if the goal is detection of contagious virus.
12/
One looking at BD rapid test which, like BinaxNOW showed that a rapid test is potentially MORE accurate than PCR if the goal is detection of contagious virus.
12/
https://twitter.com/michaelmina_lab/status/1313523532207448070?s=20
An additional important study just came out as well from @MarionKoopmans lab that not only showed that rapid antigen tests can be very accurate to detect culturable virus - but importantly shows that not all rapid tests are equal
13/
https://twitter.com/MarionKoopmans/status/1316376835530403841
13/
In that study, they found that some rapid tests: another rapid test from Abbott 'PanBio' and the SD Biosensor rapid test performed exceptionally well against high virus. While other tests performed quite poorly.
15/
15/
Still though, even the poorest tests in that study, one by Rapigen, performed with >70% sensitivity and thus could still have a role in identifying many contagious people.
16/
16/
To conclude, the evidence is mounting for the role of rapid antigen tests.
These tests work to identify infectious people quickly, without delay. They are best used to identify infectious people when they are used frequently:
nejm.org/doi/full/10.10…
These tests work to identify infectious people quickly, without delay. They are best used to identify infectious people when they are used frequently:
nejm.org/doi/full/10.10…
We layed out the science behind their use to control outbreaks here, with @DanLarremore , @jameshay218 @brwilder @MilindTambe_AI, Roy Parker and others
medrxiv.org/content/10.110…
18/
medrxiv.org/content/10.110…
18/
And for any policy makers out there @alexismadrigal covered the "big idea" of how rapid tests can be used to control outbreaks here:
theatlantic.com/health/archive…
19/
theatlantic.com/health/archive…
19/
We don't need to test every person every day, just a fraction, every few days, in places where outbreaks are the worst to get them under control quickly and make everyone more safe
We don't have a vaccine yet. We might not for a while. Frequent rapid testing can work
20/20
We don't have a vaccine yet. We might not for a while. Frequent rapid testing can work
20/20
FYI Some of the confusion is that these aren’t actually false positives. also I do not call for any universal cutoff from pcr values to say someone is not infectious. But I would say that below certain Cts people are very like to be infectious. Above, we should be more nuanced.
• • •
Missing some Tweet in this thread? You can try to
force a refresh



