Some optimistic commentary here from @FICMNews
Dean @AlisonPittard, suggesting we are getting better at treating COVID-19 leading to fewer deaths than the first wave. Is this over-optimistic, or are patient outcomes really getting better? 1/18
bbc.co.uk/news/health-54…
Dean @AlisonPittard, suggesting we are getting better at treating COVID-19 leading to fewer deaths than the first wave. Is this over-optimistic, or are patient outcomes really getting better? 1/18
bbc.co.uk/news/health-54…
Importantly, @AlisonPittard is not just giving her opinion. Her comments are based on published data. For many years UK intensive care units have reported activity data to @ICNARC. During the pandemic, some of the most robust and objective data reports have come from them. 2/18
The latest @ICNARC report published yesterday describes outcomes for COVID-19 patients admitted to intensive care before and after 1st September. The report is available here: icnarc.org/Our-Audit/Audi… But remember this ONLY tells us about patients admitted to ICU (see later). 3/18
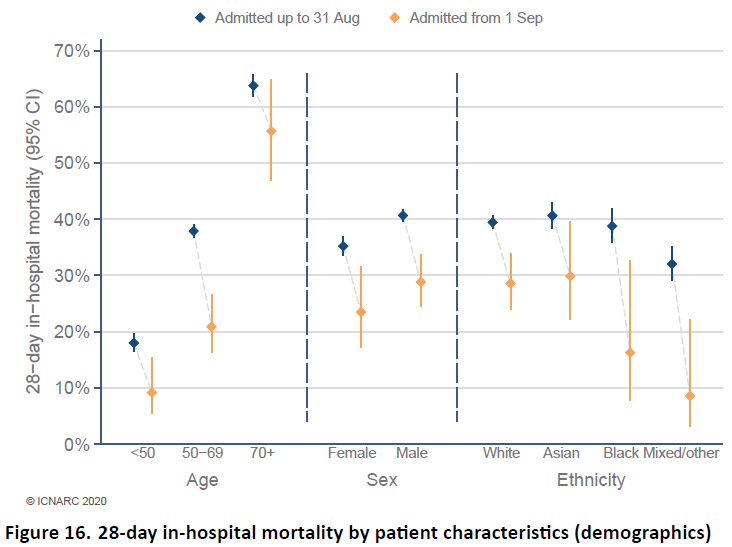
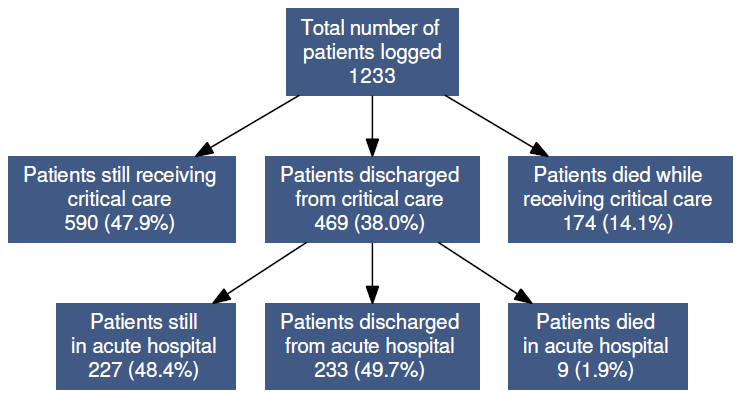
On the face of it, survival does seem to be better: ~15% of COVID patients admitted to ICU since 01/09/20 have died compared ~40% before then. But ICU docs will tell you that difference is huge. Can this be true? Well, yes and no.... 4/18 
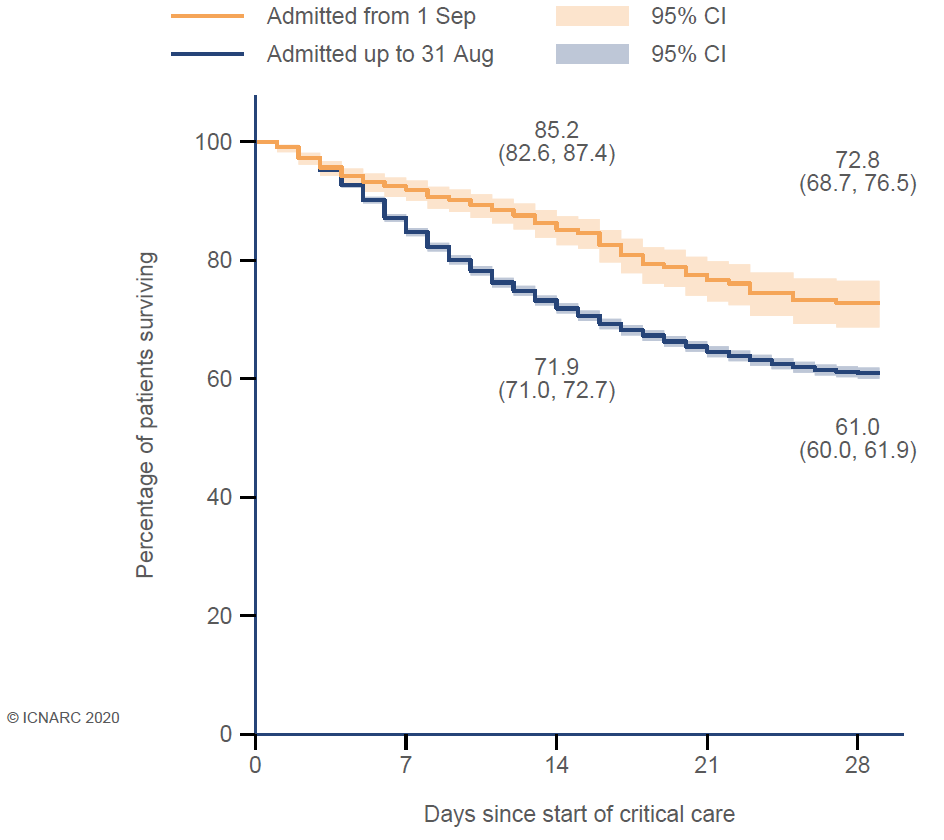
First thing to note is sample size. We're comparing only 1233 patients from 01/09/20 onwards with 10,900 patients from before. 1233 sounds like a lot but when we break this down into different patient groups (age, ethnicity, etc) the numbers get quite small. Caution needed. 5/18
Then we look at casemix: the types of patients. How old were they? How many had other diseases? How sick were they? Well age, sex, ethnicity, obesity are similar to 1st wave. Only social deprivation seems worse. So demographics pretty similar but better outcomes since 01/09. 6/18 
The number of patients with pre-existing severe medical problems also looks similar, as does functional independence (fit enough to do daily activities). Possibly more pregnant patients since 01/09 but these numbers are STILL SMALL so do not over-interpret them. 7/18
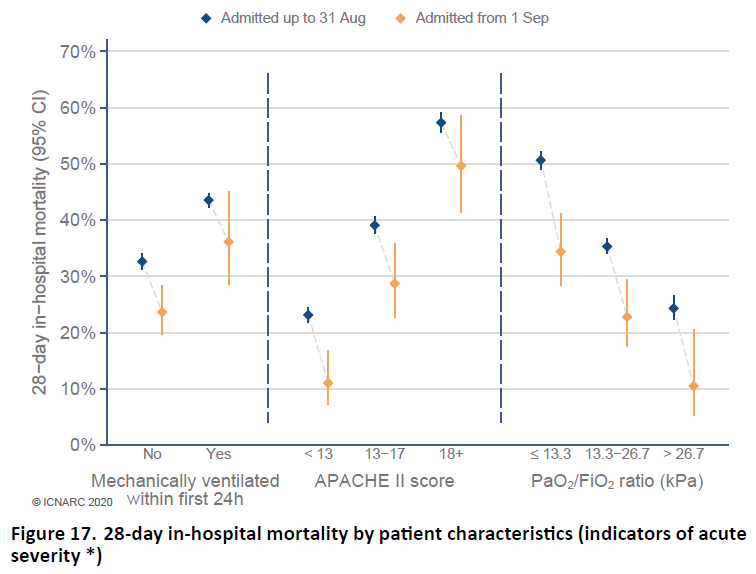
But when we look at how ill these patients are, it gets interesting. Various statistical measures suggest that since since 01/09, on average, patients are less seriously ill at the point of admission to ICU. Could this explain why fewer patients have died? 8/18
In particular, fewer patients were admitted to ICU with very low blood oxygen levels and, most importantly, far fewer patients needed to be placed on a ventilator within the first 24 hours on ICU - 58% patients ventilated in first wave compared to 26% since 01/09/20. 9/18 
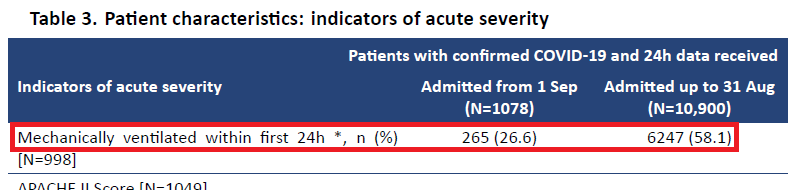
This seems strange until we remember that most of the time since 01/09 ICUs have been working within their normal maximum capacity. Almost every critically ill patient can be admitted to ICU. In the first wave we had to treat many less critically ill patients outside ICU. 10/18
Remember ICNARC data only tell us what happens in ICU, not the whole hospital. If we have more space in ICU, we admit more patients and that means the average level of illness is less severe (when ICU beds are in short supply we admit the sickest patients first). 11/18
Normally (pre-pandemic) we ventilate around 40% of ICU patients. In the first wave we ventilated >60% while colleagues in respiratory medicine looked after many patients with low blood oxygen levels on standard hospital wards. Right now that isn't happening as often. 12/18
So are we doing better or not?! Well this graph seems to be the key one. Here we see that outcomes in all the different risk categories (from low to high) do appear to be better for COVID-19 patients admitted to ICU since 1st September. 13/18 
Big note of caution: Almost half the ICU patients admitted since 01/09 are still there (left hand box in image below). These patients have not survived ICU yet. Many will sadly die despite our best efforts. The data are still live and the survival figures will change. 14/18 
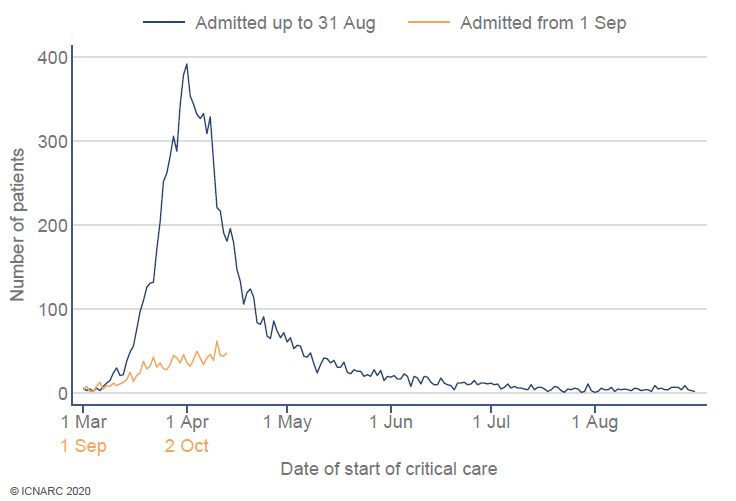
A crucial detail from the @ICNARC report is the graph below. The increase in COVID ICU admissions is much slower since 01/09. The wave of cases is more spread out and our capacity less likely to be overwhelmed at any one time. This is because of #HandsFaceSpace. It works! 15/18 
So I agree with @AlisonPittard. We have reason to be optimistic. We're getting better at treating this disease. Every day we learn more about what works and what doesn't. But we can't relax yet. It will be a tough winter and things will get worse before they get better. 16/18
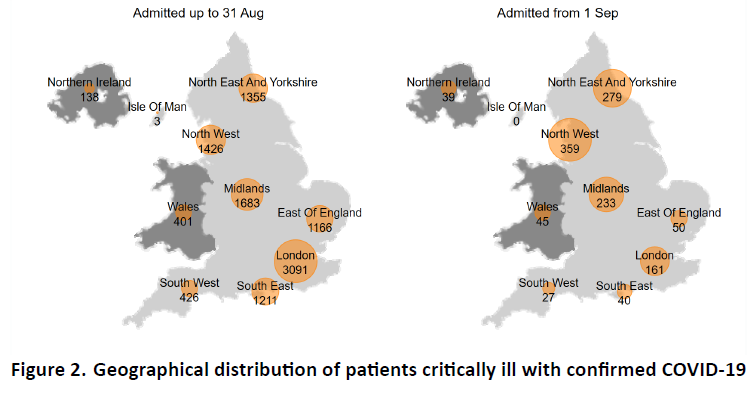
Geographical patterns have reversed and the surge in cases is currently hitting hospitals in the north of England much harder. Some ICUs have already re-opened temporary ICU beds. We must be sensitive to this. We cannot allow these regional differences to divide us. 17/18 
Thanks again for your incredible support for key-workers this year. Your kind words mean more than you can know. The NHS is still here for you and we'll keep going until the job is done. Thanks to @ICNARC for the data. Another lovely photo of @teamaccu from @jometsonscott. 18/18 

• • •
Missing some Tweet in this thread? You can try to
force a refresh