
The COVID-19 pandemic has shown power of open data and analytics in research, but these activities often aren't recognised in traditional academic metrics. New perspective piece with @rozeggo & @sbfnk: journals.plos.org/plosbiology/ar…. I'd also like to highlight some examples... 1/
- Curation of open data sources, such as line list data by @MOUGK @davidmpigott et al (github.com/beoutbreakprep…), case tracking by @TexasDownUnder et al (coronavirus.jhu.edu/map.html), testing from @OurWorldInData (ourworldindata.org/coronavirus-te…)... 2/ 



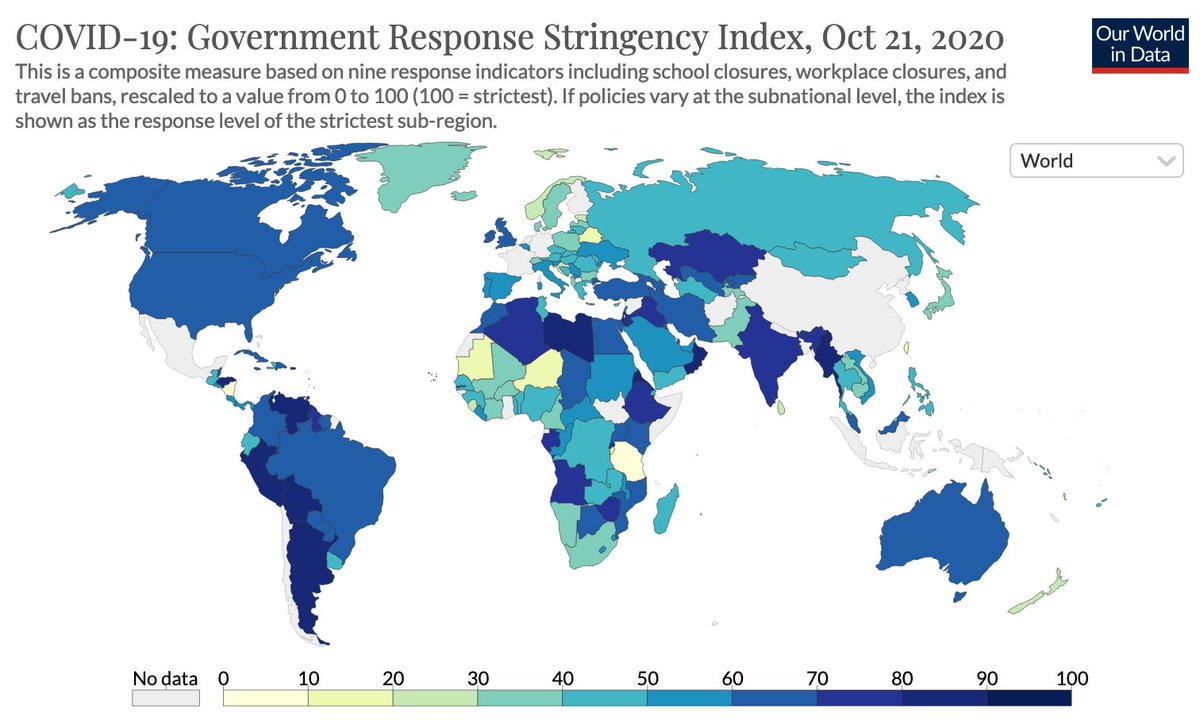
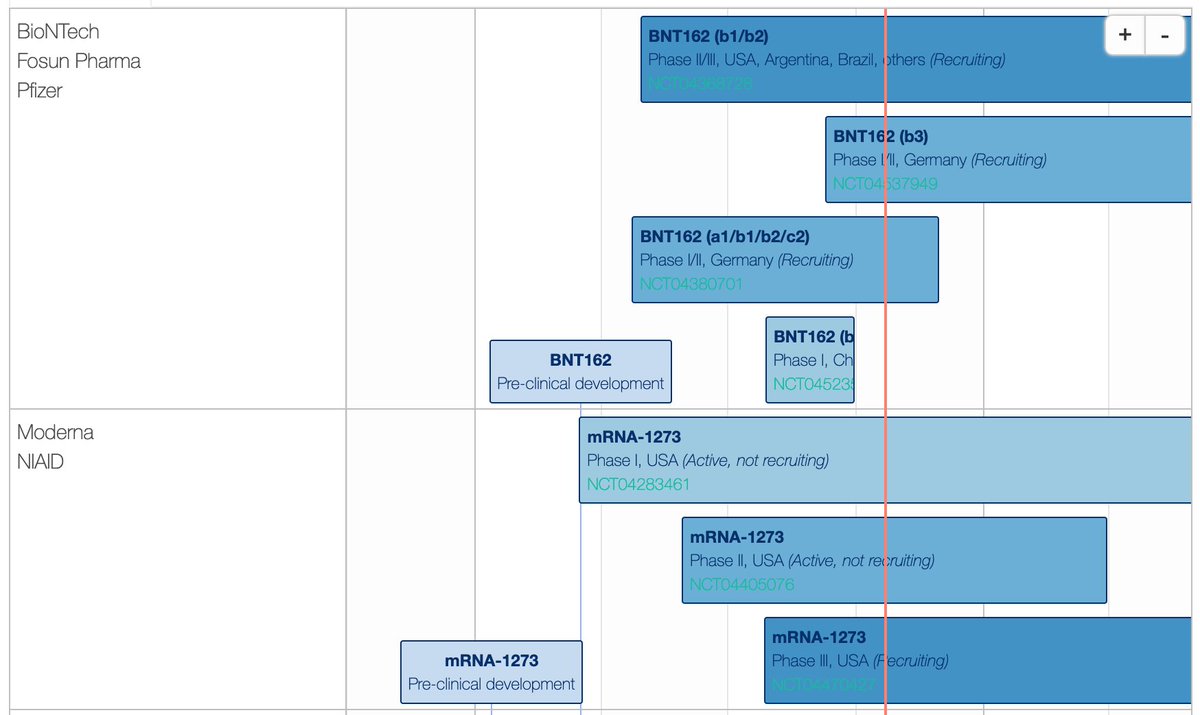
...government responses by @thomasnhale et al (bsg.ox.ac.uk/research/resea…), vaccines by @LSHTM_Vaccines (vac-lshtm.shinyapps.io/ncov_vaccine_l…), behaviour by @Imperial_IGHI (github.com/YouGov-Data/co…) 3/ 

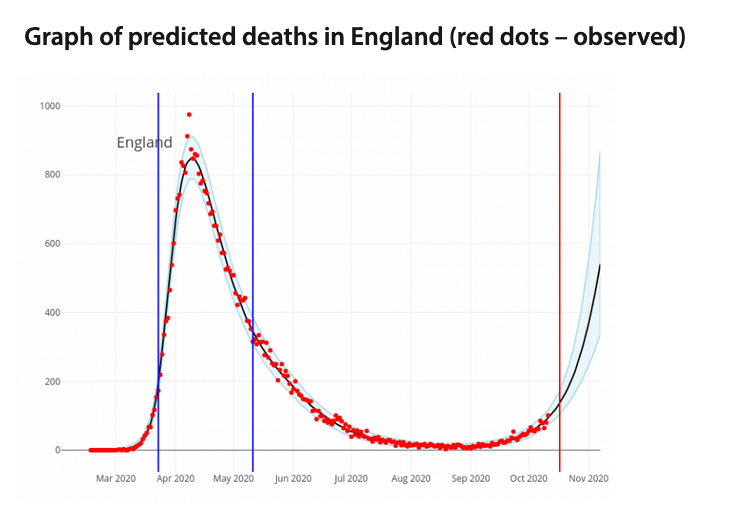
- Reproduction number estimation & forecasting, including dashboards by @bencowling88 et al (covid19.sph.hku.hk), @cmmid_lshtm (epiforecasts.io), @MRC_BSU (mrc-bsu.cam.ac.uk/tackling-covid…), @reichlab et al (viz.covid19forecasthub.org) 4/ 


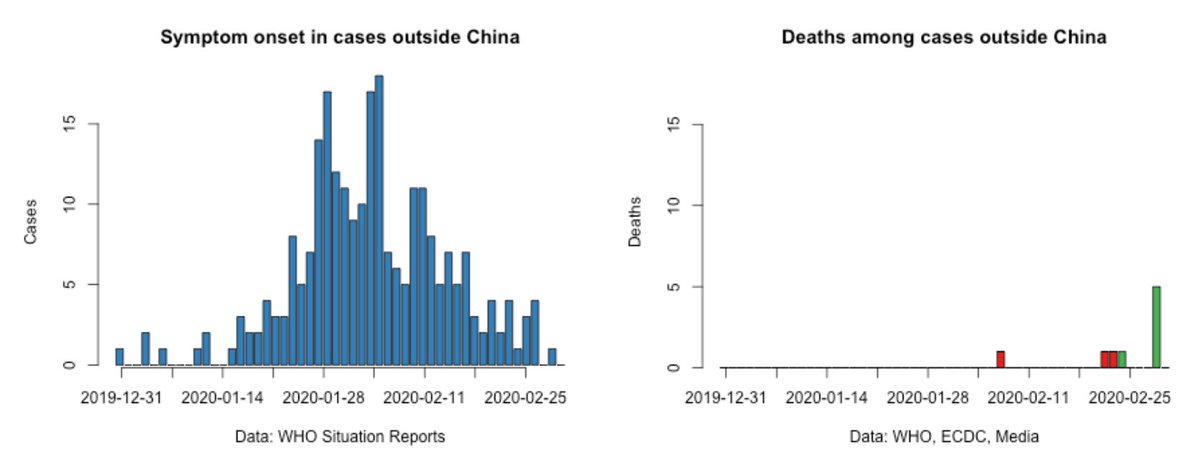
- Key epidemiological parameters, including analysis of fatality risk by @C_Althaus (github.com/calthaus/ncov-…), overdispersion by @khgrantz et al (hopkinsidd.github.io/nCoV-Sandbox/D…), asymptomatic transmission by @dianacarbg et al (medrxiv.org/content/10.110…) 5/ 


- Mobility patterns and predicting risk of international spread by @alexvespi et al (datastudio.google.com/reporting/3ffd…) and @WorldPopProject (worldpop.org/events/china) 6/ 



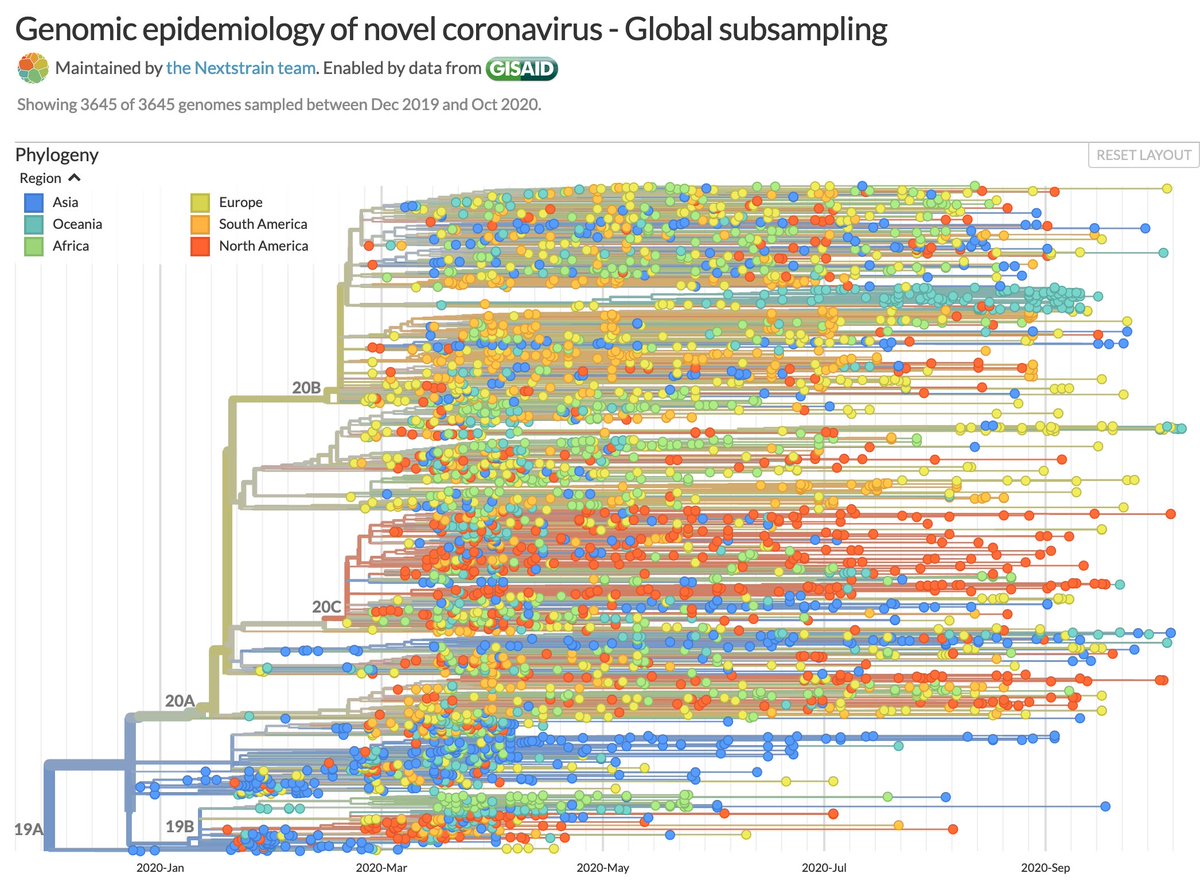
- Genomic analysis of global spread, in Brazil by @nmrfaria et al (virological.org/t/first-cases-…), China by @arambaut et al (virological.org/t/phylogenetic…), and globally by @nextstrain (nextstrain.org/ncov/global?c=…) 7/ 


-Open models and scenario tools, such as EpiNow2 by @seabbs et al (github.com/epiforecasts/E…), OpenABM by @ChristoPhraser et al (github.com/BDI-pathogens/…), & tools to explore scenarios by @n_b_noll et al (medrxiv.org/content/10.110…) and @_nickdavies et al (cmmid.github.io/visualisations…) 8/ 



There are many, many other examples out there. COVID-19 has shown academics are highly motivated to produce work with immediate impact, even if it's beyond scope of traditional metrics. Now is the time to change the incentive structure to recognise these efforts. 9/9
• • •
Missing some Tweet in this thread? You can try to
force a refresh


