
Next up for some tweet-ucation is “Antibiotics and Fluids: Controversies in Sepsis Care”! #CHEST2020
The first session is "Early Broad-Spectrum Antibiotics Save Lives" with Dr. Angel Coz! #CHEST2020 

The 2016 guidelines recommend broad-spectrum antibiotics to cover all likely pathogens, but those won't be the same for every patient! #CHEST2020 

We know that the duration of hypotension before initiation of effective antimicrobial therapy....
#CHEST2020

#CHEST2020


There is a decline in mortality when sepsis bundles were mandated. #CHEST2020 

Progression to septic shock is more likely with delays in antibiotics. #CHEST2020 

Supply chain delays also affect mortality, so remember that placing the order for antibiotics is not enough! #CHEST2020 

Inappropriate antibiotic therapy resulted in a 5-fold reduction of survival in shock. #CHEST2020 

These studies show that a lot of patients with sepsis have negative cultures. #CHEST2020 



Culture-negative sepsis still has a high mortality. #CHEST2020 

So what is the downside of broad spectrum antibiotics? #CHEST2020
At least 30% of human antibiotic prescriptions are considered unnecessary. If we want to decrease antibiotic use we should target outpatient use rather than among the most critically ill who are higher risk. #CHEST2020 



If we do not use broad spectrum antibiotics in our sickest patients, who are we saving them for? #CHEST2020 

Summary #CHEST2020 

The next session is "Empiric Broad-Spectrum Antibiotics Should NOT be Routinely Administered to All Septic Patients" with Dr. Jayshil Patel! #CHEST2020 

Time sensitive aspects of sepsis control #CHEST2020 

The range of possibilities - The ideal is the appropriate antibiotics without delay. #CHEST2020 

Guidelines #CHEST2020 

Survival is decreased per hour delay in antibiotics. #CHEST2020 

Surviving Sepsis Guideline #CHEST2020 

What does empiric therapy mean? Broad spectrum therapy? #CHEST2020 

Implications of recommendations #CHEST2020 

Before widespread policy is implemented we should determine the value. To increase value you either need to increase the quality or outcomes or decrease the cost/harm. #CHEST2020 

This is what an observational study looks like. #CHEST2020 

The studies included in this meta-analysis were observational. #CHEST2020 

This is an updated systematic review that favors appropriate antimicrobial therapy. #CHEST2020 

What can we conclude so far? #CHEST2020 

What do these observational studies have in common? #CHEST2020 

What are the implications of studies that compare appropriate to inappropriate antibiotics? #CHEST2020 

Good question! #CHEST2020 

There is potential for harm with broad spectrum antibiotics, including adverse drug effects, C diff, and altering the microbiome. #CHEST2020 

So does appropriate therapy equal broad spectrum? #CHEST2020
So what should we do? #CHEST2020 

Different patients need different antibiotics to be "appropriate". #CHEST2020 

Summary #CHEST2020 

The next session is "30 mL/kg: An Appropriate Initial Fluid Bolus for the Treatment of Severe Sepsis and Septic Shock" with Dr. Chhaya Patel! #CHEST2020 

The question #CHEST2020 

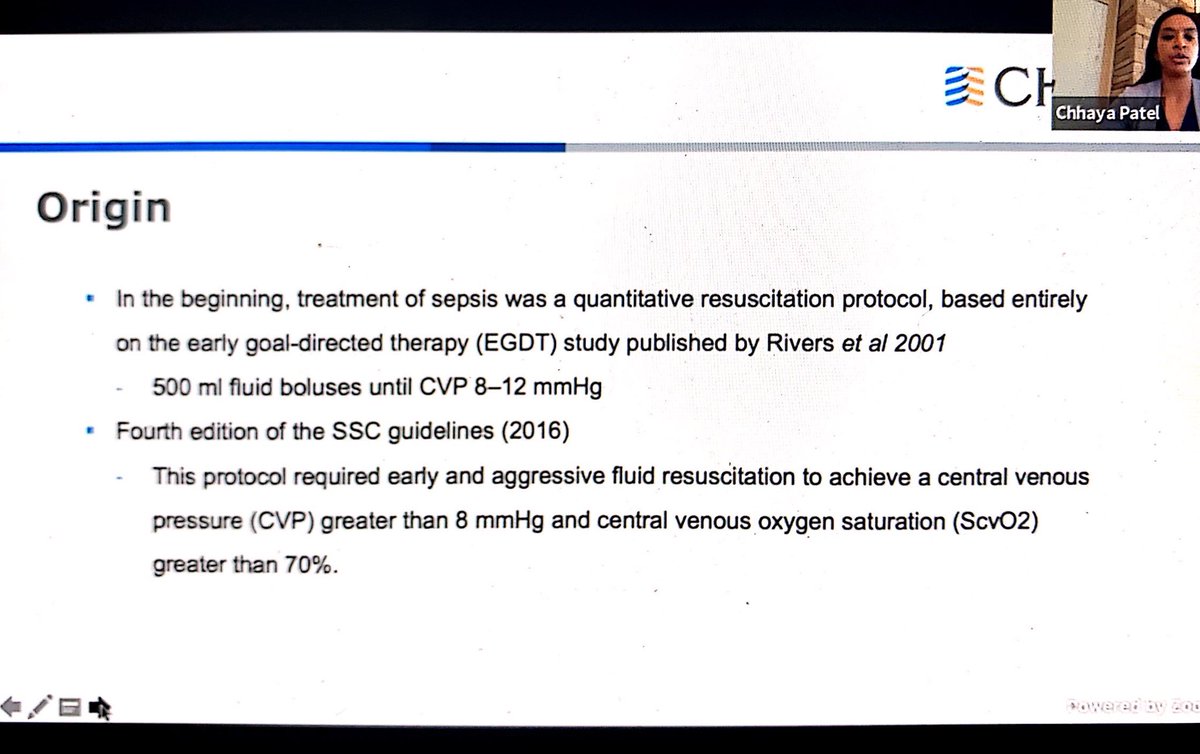
The origins of fluid resuscitation #CHEST2020 
The primary physiologic problem with septic shock is vasodilation with maldistribution of blood to organs. #CHEST2020 

Summary of methods predicting preload responsiveness #CHEST2020 

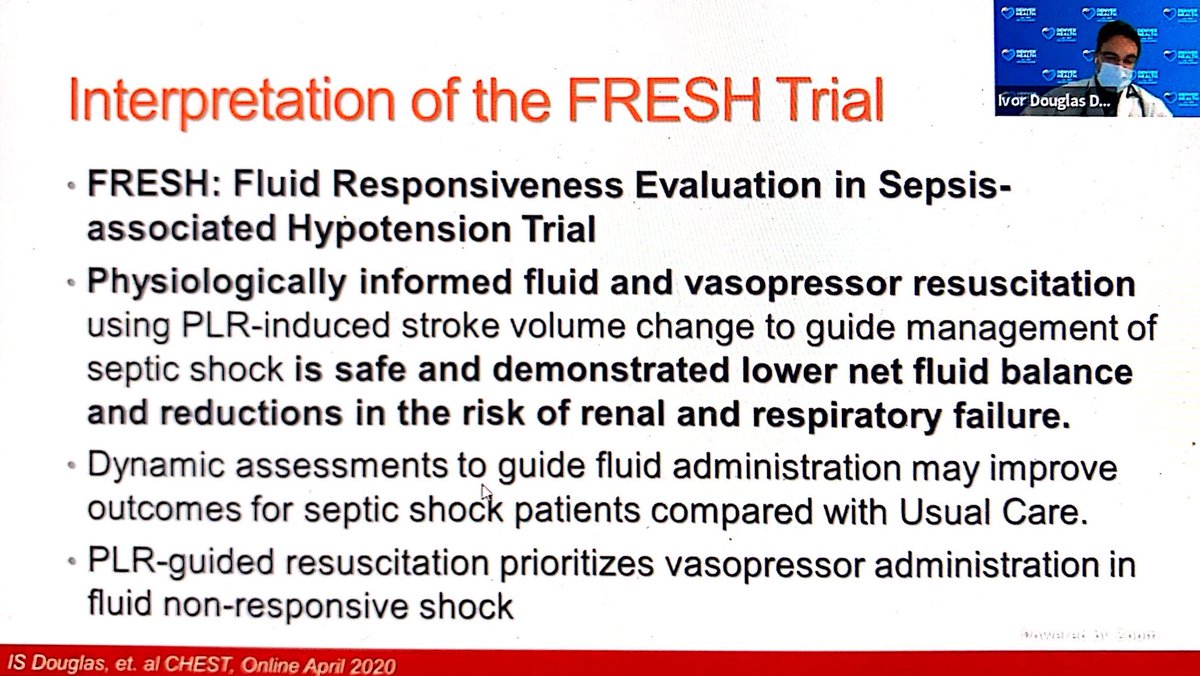
This study showed that the use of passive leg raise SV change to guide management is safe.
#CHEST2020
#CHEST2020

The surviving sepsis guidelines recommend at least 30 ml/kg IVF to be given within the first 3 hours.
#CHEST2020
#CHEST2020

This is the idea behind the recommendation to give the initial fluid bolus. #CHEST2020 

These papers support the use of the initial fluid bolus. #CHEST2020 

In the ARISE trial the EGDT group got a little more fluid at the beginning, but that difference evened out later on. #CHEST2020 



Promise trial also evened out between 6 and 72 hours. #CHEST2020 

So does fluid cause harm? In this study they found lower mortality in the group receiving higher IV fluid volume with persistent shock. #CHEST2020 

This 2014 study looked at fluid administration in the first 3 hours and showed those who got more fluids in the first 3 hours had lower hospital mortality. #CHEST2020 
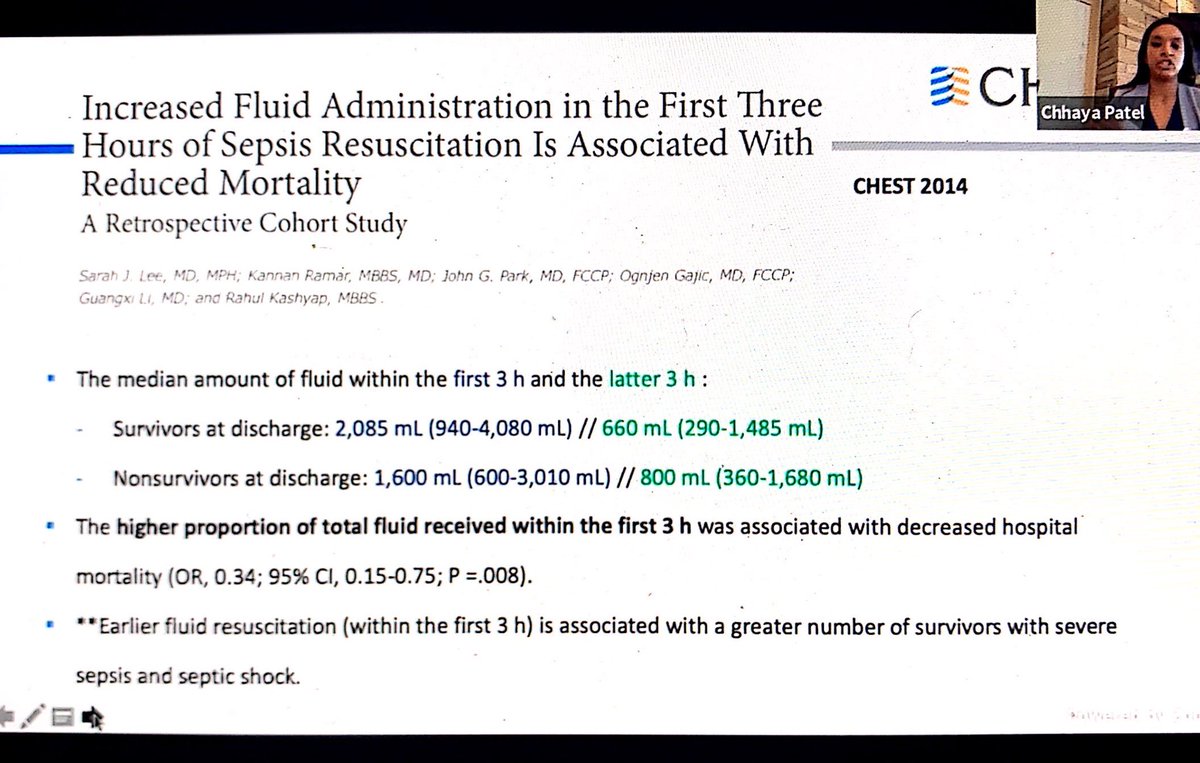
This study from 2019 noted that higher fluid volumes administered by 3 hours correlated with decreased mortality. #CHEST2020 

Conclusions #CHEST2020 

There is a wealth of data that fluids can be harmful. #CHEST2020 

Mechanism of septic shock in CHF #CHEST2020 

This study concluded that CHF patients with septic shock should receive the recommended fluid administration if they present with hypotension. #CHEST2020 

This retrospective study showed improved mortality with adherence to initial fluid resuscitation guidelines. #CHEST2020 

This study showed that initial IV fluid was associated with lower mortality IF negative fluid balance was obtained on two consecutive days within the first 7 days of shock. So it's important to DE-RESUSCITATE, as well. #CHEST2020 

This study found that a de-resuscitative fluid strategy resulted in an increased number of vent-free days and decreased ICU LOS. #CHEST2020 

This study found no difference in the incidence of intubation in patients with cirrhosis, ESRD, aor CHF who received fluid resuscitation. #CHEST2020 

Conclusions #CHEST2020 

The final session is "Fluid Bluses Should be Individually Tailored" with Dr. Ivor Douglas! #CHEST2020 

SEP-1 measures #CHEST2020 

Why fluid resuscitation matters! #CHEST2020 

This isn't just a macro-circulatory problem, but has to do with alterations in endothelial function and microcirculatory blood flow. #CHEST2020 

In EGDT trials there was no difference in fluid volume administered between protocolized resuscitation and usual care. #CHEST2020 

Studies have shown increased mortality with delayed antibiotics, not fluid bolus. #CHEST2020 

Pathophysiological effects of volume overload #CHEST2020 

Delays in vasopressor administration is associated with worse outcomes. #CHEST2020 

The case for individualized boluses #CHEST2020 

Not all patients will respond to fluid! #CHEST2020 



FRESH Resuscitation Protocol #CHEST2020 

There was a significantly reduced fluid balance. #CHEST2020 

Interpretation of the FRESH trial. #CHEST2020 
Thanks to all of our wonderful speakers! #CHEST2020
• • •
Missing some Tweet in this thread? You can try to
force a refresh












