
And we're back with guidelines part 2! Updates on paediatrics, neonates, first aid and education! #RESUS20 @ERC_ALS_SEC @ERC_resus with @perkins_gd and @HSvavarsd 

Paediatric update with Patrick Van de Voorde. If they look like an adult, use adult guidelines. BVM is first line. Oxygen is a drug and should titrate to 94-98%. Reassess frequently with fluid boluses #RESUS20 







ALS updates for pediatrics @ERC_resus @ERC_ALS_SEC draft coming soon for comments! Watch this space #RESUS20 





AEDs in paediatrics is difficult due to aetiology but may still make a difference. If you are a two rescuer team please do locate and apply AED in paediatric arrests. Follow your BLS or PLS training for ratios of 15/2 and 30/2. If untrained, call EMS for assistance #RESUS20
Newborn updates with Charles Roehr #RESUS20 very active research area. Keep 2015 guidelines until 2020 officially released! Ideal O2 conc is controversial. Majority <32/40 will require O2 aim between air-30%. Term babies aim room air
Breathing support at birth is not "one size fits all". Subgroup of babies develop dive reflex and stop breathing with PEEP #RESUS20 sustained inflations are not recommended - the smaller the baby the worse they fare
Continue with 5 inflation breaths of 2-3 seconds as per 2015. Tracheal suctioning is now discouraged in routine amniotic stained fluid births! Ventilate first results in fewer babies to NICU with meconium aspiration #RESUS20 #neonatal
Neonatal Resuscitation is changing. Leave your comments and thoughts on the ERC.edu public space 

First aid updates with David Zideman #RESUS20 @ERC_ALS_SEC @ERC_resus recovery position only for those with abnormal breathing. Cooling for heat stroke life saving peri arrest. Tourniquets should only be removed by a HCP once put on! 







First aid: Thermal burns need cooling for 20minutes minimum. Compression wrap alone doesn't have an indication but may be helpful when used as part of RICE strategy #RESUS20 #firstaid 



A problem is the belief that anyone who is unresponsive should be put in recovery position. May not be the case! Can be useful in certain circumstances when breathing normally to stop airway obstructing. But should only be done when having to leave the person alone #firstaid
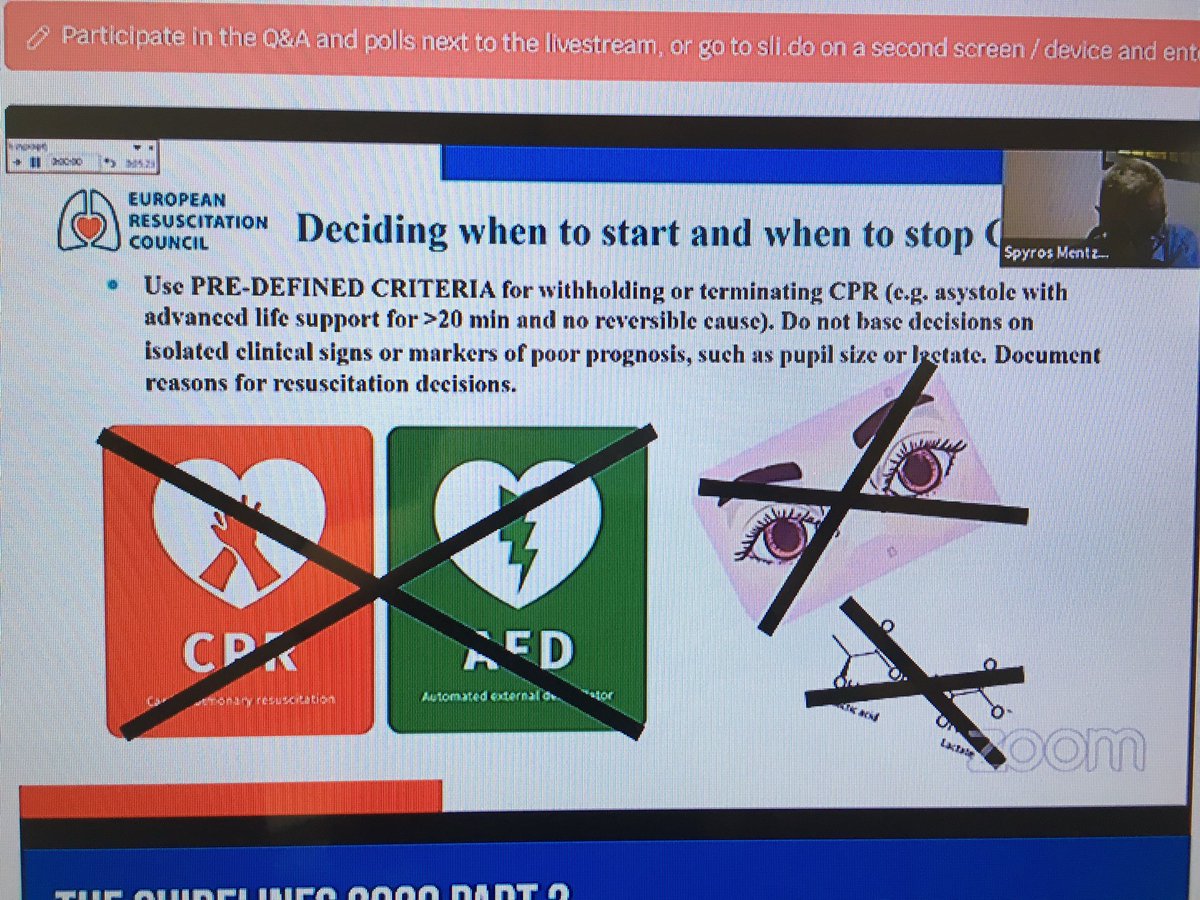
Ethics update with Spiros Mentzelopoulos #RESUS20 advanced care planning is fundamental for shared decision making and safeguarding. Need pre determined criteria for withholding/terminating CPR @ERC_resus 




Education update with Tino Grief #RESUS20 new chapter coming with guidelines 2020! Resuscitation is a blend of learning in your own bespoke way and practical assessment from the experts to stay competent @ERC_resus 



• • •
Missing some Tweet in this thread? You can try to
force a refresh







