The @gmcuk annual training survey is out, looking in particular at the impact of COVID19 on medical trainers and trainees
gmc-uk.org/-/media/docume…
gmc-uk.org/-/media/docume…

As always there is lots of granular data in the report but at the high level:
~25% of trainees & ~20% of trainers score “high” or “very high” on Copenhagen Burnout Inventory questions in the survey
40% of both trainees and trainees describe work as emotionally exhausting
~25% of trainees & ~20% of trainers score “high” or “very high” on Copenhagen Burnout Inventory questions in the survey
40% of both trainees and trainees describe work as emotionally exhausting

And almost half report feeling tired/fatigued at the end of the day
(though, as always, I think the phrasing of the question “are you exhausted in the morning at the thought of work” is quite an existential way of asking it!)

(though, as always, I think the phrasing of the question “are you exhausted in the morning at the thought of work” is quite an existential way of asking it!)


It’s been clear for a long time now that our NHS is functioning on fumes - the good will and personal reserves of NHS staff - and that that has an inevitable cost, both for patient safety but also for the health, wellbeing and safety of our staff
“We can’t go on the way we are”
“We can’t go on the way we are”

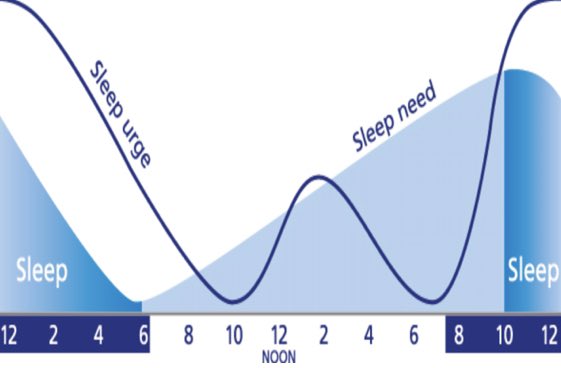
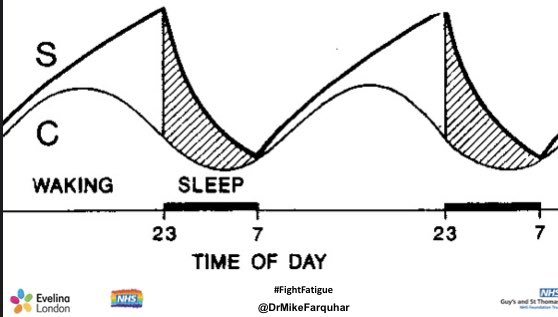
It’s why campaigns like HALT @GSTTnhs are so important: we have to get the absolute foundational basics, like regular rest and breaks, right 

In the wider NHS, @Assoc_Anaes @RCoANews @FICMNews, with their #FightFatigue campaign, have been clear leaders in offering practical strategies to help departments - in all specialties - change their culture around rest, breaks and staff wellbeing
anaesthetists.org/Fatigue
anaesthetists.org/Fatigue

We still have a huge problem with “superhero culture” in NHS - the idea many NHS staff have that, when resources we need aren’t there, that somehow we are able to continue pulling it all out of our own personal reserves, and if we don’t that WE -not those in charge- have failed 

There’s only so much we can do to make this better with resources we have
If we don’t improve this, staff and patients will continue to suffer consequences, and things will only get worse
We need a comprehensive approach to #SafeStaffing if we are genuine in delivering the best
If we don’t improve this, staff and patients will continue to suffer consequences, and things will only get worse
We need a comprehensive approach to #SafeStaffing if we are genuine in delivering the best

• • •
Missing some Tweet in this thread? You can try to
force a refresh