
Folks concerned about my advocacy for structural, neurological diagnoses, for #MCAS and connective tissue disorders, or for "#MEspine"––I really do want to understand what is at the heart of this. Frankly, it has been hard.
There is a lot of misinformation floating around (or simply lack of education/awareness––again, it's a lot of different conditions, and I know next to nothing about most of them, other than the ones I happen to have). 
I see a really big gap between how American patients are responding to this information v. patients in the UK & Europe, and I don't fully understand all of the reasons for that. I think that's worth discussing amicably, if we can.
It may be that we may be one, (mostly anglophone) corner internet but that we face very different opportunities, challenges, and risks depending on where we live, both as individuals and communities (we should talk about that).
I've tried to talk about the benefits (and risks/costs) of diagnosis but to emphasize that diagnosis does not inevitably imply surgery. I am hearing that some people agree with this but say, "but I am really concerned about surgery."
While others have said, "I don't even think diagnosis is a good idea. How do we know that people are being accurately diagnosed? I have a hard time believing all these people in our community have these undiagnosed conditions no one figured out."
Regarding being concerned about surgery––I am really concerned, too. I have general concerns about surgery for anyone with undiagnosed EDS, MCAS, or a c-spine problem. After all, it was having thyroid surgery w/ undiagnosed CCI/AAI + TC that got me into this mess.
I am less concerned about ACDFs, SFTs, or styloidectomies. There are a whole lot of surgeries that I don’t know anything about that have their own risks, indications, and evidence bases. Here are my specific concerns about craniocervical fusions:
https://twitter.com/jenbrea/status/1332808036616867840?s=20
I think it is absolutely right to urge caution, identify risks, and tell people to SLOW DOWN when it comes to deciding to have major surgery, but...that is what we see the majority of people doing.
This is a process that can organically take a year or often much more, if you seek multiple opinions, learn about your diagnoses and all their treatment options, and talk to other patients.
The idea that there needs to be an ME-specific clinical trial does not make sense to me. To all of these surgeons, from their perspective, they probably think “What is ME? I’ve never even heard of that before?” or that it was a misdiagnosis...
I think what’s going on is more nuanced than that––the circumstantial evidence that a subset of patients in our community have a connective tissue disorder (genetic, acquired, or both) is HIGH. I think this soup of “new” diagnoses is just an echo of that.
These neurosurgeons are just recognizing what they observe as being present, using the same diagnostic methods as they were using two years ago, as many were using ten years ago.
Yes, some of these DM’s do have unresolved questions/evolving understandings re: diagnostic methods, surgical thresholds, and techniques. Others are perfectly ho-hum. Still others are so rare, there can’t be a universal standard of care: not enough people are affected by them.
But we aren’t going to tackle all that to start (these diagnoses existed long before most of us got sick, and have their own research communities, advocacy organizations, etc.).
Rather, what I think we need is BETTER observational data: epidemiology to understand the actual rate of missed diagnoses in our patient community, and if they follow a pattern that can help point to something more broadly true about the disease process(es) that can lead to ME.
To definitively answer questions like: are there really higher rates of hEDS, HSD, intracranial hypertension, “craniocervical obstructions,” Tarlov cysts, and the myriad other connective tissue disorder-associated neurological diagnoses in our community.
And if so, do we only find them in EDS patients? Or do we also find them in patients who don’t meet any common understanding of EDS as well? If so, why do we find these diagnoses in these patients?
Can these issues arise from complications of acquired connective tissue disorders or damage? Of MCAS? Or do we need to redefine how we categorize EDS?
So those are the concerns that keep me up at night and the questions I think we need to be asking. And if we establish that a lot of ME patients have these diagnoses, then yes, we can start to study how they relate to symptoms and pathophysiology...
...and even move to trials so we can better optimize treatment (and hopefully develop more/better nonsurgical options).
But we cannot make any blanket statements regarding treatment access. To do would be absurd. When left untreated, most of these conditions are chronic but can be debilitating. However, tethered cord can be progressive. In some cases, Chiari can be life-threatening.
There can be costs to deterring people from diagnosis, especially if they have neurological symptoms. The “right” decision is diagnosis and case-dependent, always.
As for this skepticism...let me see, so many possible answers.
https://twitter.com/jenbrea/status/1335761646640222208?s=20
First, #EDS patients often have to walk through a very similar hell to #MECFS patients to get diagnosed. They are similarly disbelieved and psychologized. Life-altering diagnoses are routinely missed.
In Europe, they can also face sectioning for severe eating disorder (MALS?) or removal of their kids due to unexplained bruises (vEDS?) or dislocations (cEDS? hEDS? Pick your EDS). Well, some ME patients are EDS patients, too.
To ask this is to fail to understand the experiences of the EDS community.
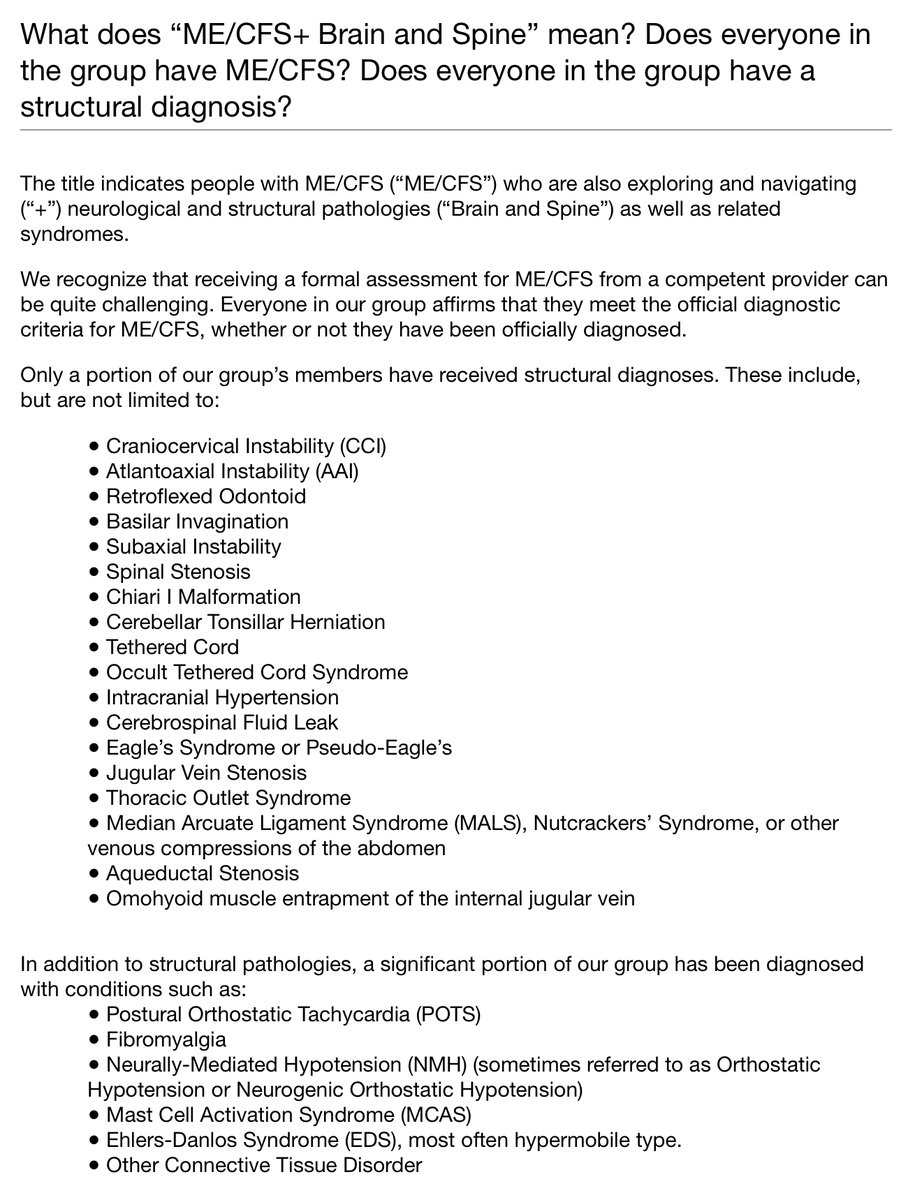
In addition to how hard it is to get a genetic CTD disorder, when you take the pathologies themselves––many #MECFS patients have never even had a brain MRI! Let alone the imaging required to diagnose these conditions:
https://twitter.com/jenbrea/status/974657621268471808?s=20
What has been your general experience with neurologists? Mine is that they give up pretty quickly if they can’t figure out what is wrong on a cursory first pass, if you even get to imaging (always a brain MRI, no one ever thought to look at my spine).
They can jump to a psychiatric or functional diagnosis with astonishing speed. And that it is possible that we are missing a whole host of diagnoses in a whole lot of people (not just ME patients) because of FUNDAMENTAL WEAKNESSES in our medical system.
These are universal problems, present in every country, that affect us deeply but no only #pwME. The idea that something weird happened to us but everywhere else, teh weather is fine is *not true.* I learned this in profound ways during the release of @unrestfilm...
...which brought me into direct contact not only with thousands upon thousands of ME patients, but patients with other diagnoses as well.
– there are not enough resources
– we cope with this by denying people investigation, treatment and care
– this coping strategy is actually *extremely costly* and maladaptive, but no one notices or raises a fuss because we externalize those costs to the most vulnerable
– we cope with this by denying people investigation, treatment and care
– this coping strategy is actually *extremely costly* and maladaptive, but no one notices or raises a fuss because we externalize those costs to the most vulnerable
– we invest less in researching and treating diseases that disproportionately affect women (every diagnosis I can think of is female preponderant, including all those neurosurgical ones!)
– there are major class and race issues at play. if I hear one more doctor wonder why his [insert diagnoses] patients are all “type A, middle/upper class white women” I am going to scream.
- sometimes fifteen minutes is all a patient has of a doctor’s time. It took me putting my story in a nationally televised film to put me on a path to diagnosis of my neurosurgical condition *after six years of severe illness.*
Given how most of us have personally been treated, given the experiences we see so many patients have, should this really surprise us? These factors are a recipe for disaster and that is what we (#NEISvoid) have.
• • •
Missing some Tweet in this thread? You can try to
force a refresh


