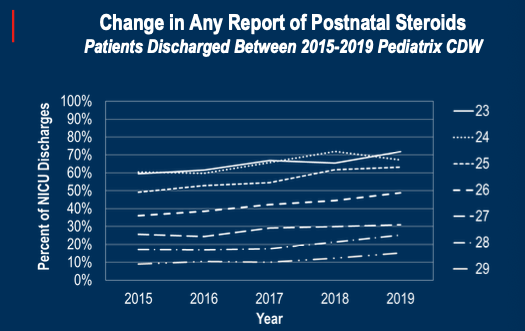
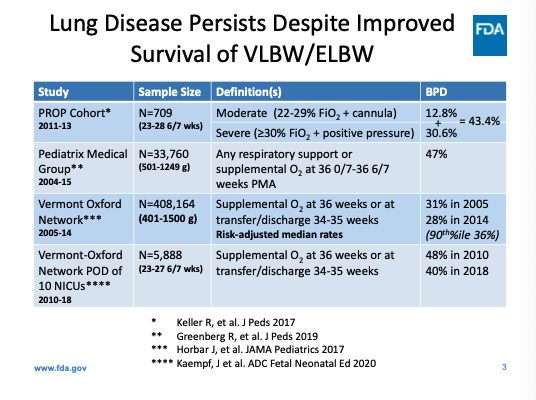
Next up in #HotTopicsNeo2020: Erik Jensen of @ChildrensPhila discussing how the baseline risk of BPD impacts the number needed to treat when considering effective therapies.
chop.edu/doctors/jensen…
@HotTopicsNeo
chop.edu/doctors/jensen…
@HotTopicsNeo

Presentation builds on recently published report in @JPediatr: drugs to Prevent Bronchopulmonary Dysplasia: Effect of Baseline Risk on the Number Needed to Treat
jpeds.com/article/S0022-…
#HotTopicsNeo2020
jpeds.com/article/S0022-…
#HotTopicsNeo2020
Jensen: evaluating the effect of nCPAP for preventing BPD provides an example of how baseline risk impact the NNT. The NNT increases sharply as the baseline risk decreases.
#HotTopicsNeo2020 @HotTopicsNeo #neoEBM
#HotTopicsNeo2020 @HotTopicsNeo #neoEBM

Jensen: Doyle meta-regression in @JPediatr highlighted that risk of CP with steroid use varies by baseline BPD risk:
jpeds.com/article/S0022-…
#HotTopicsNeo2020 @HotTopicsNeo
jpeds.com/article/S0022-…
#HotTopicsNeo2020 @HotTopicsNeo

Jensen: current effort to rigorously look at how baseline risk of BPD modifies the effect of postnatal systemic corticosteroids using NICHD NRN data; objective and study design.
#HotTopicsNeo2020 @HotTopicsNeo

#HotTopicsNeo2020 @HotTopicsNeo


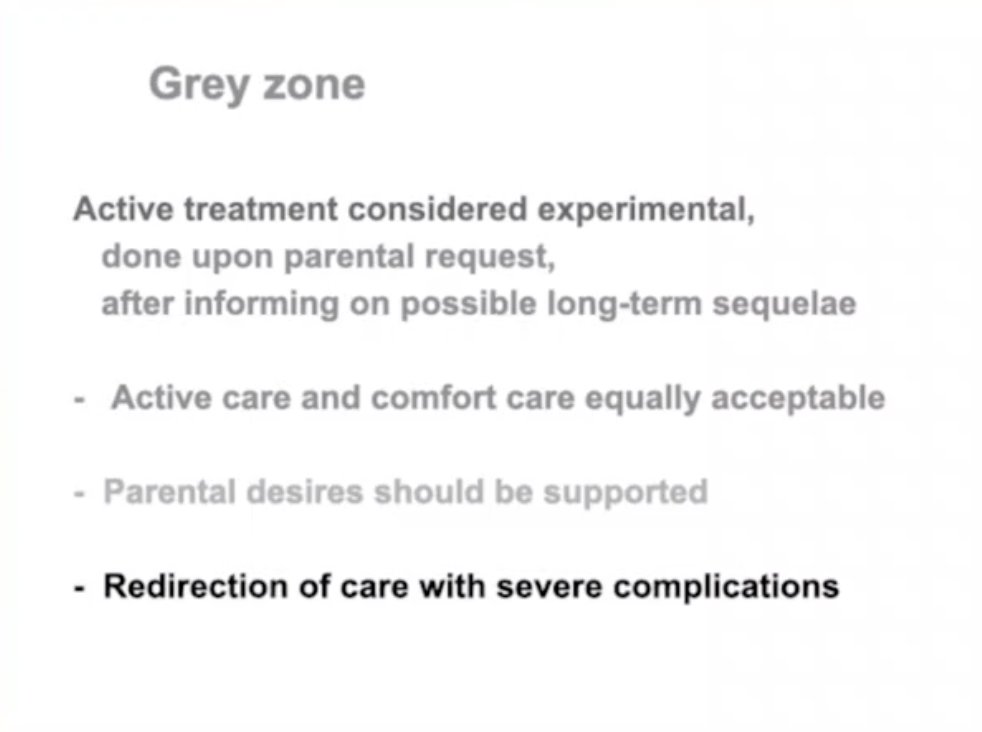
Jensen: summary of unpublished findings, outcome of death or neurologic impairment. Trendline suggests more relative benefit/harm as baseline risk increase, but analyses stratified by risk group without significant benefit in any subgroup. #HotTopicsNeo2020 @HotTopicsNeo 



Jensen: now outcome of death or CP. Similar trendline, suggests more relative benefit/harm as baseline risk increase, analyses stratified by risk group suggest likely benefit in highest risk subgroup. #HotTopicsNeo2020 @HotTopicsNeo 



• • •
Missing some Tweet in this thread? You can try to
force a refresh