
The #RELAx trial has been published today in @JAMA. It was coordinated by Anna Algera. This thread is to explain the rationale, what we did, the findings and the meaning.
The rationale of #RELAx is based on the following premises.
jamanetwork.com/journals/jama/…
The rationale of #RELAx is based on the following premises.
jamanetwork.com/journals/jama/…
First, there is NO adequate evidence on the level of PEEP in non-ARDS patients. Most of the studies are old, conducted in post-surgical patients (short-term ventilation), and were not powered to detect differences in patient-centered outcomes.
annalsofintensivecare.springeropen.com/articles/10.11…
annalsofintensivecare.springeropen.com/articles/10.11…
Second, despite the absence of evidence, the levels of PEEP used in non-ARDS patients increased over years, from 5 to 7/8 cmH2O, probably as a reflection of studies and practice in ARDS patients.
link.springer.com/article/10.100…
link.springer.com/article/10.100…
Third, one IPDM showed that higher levels of PEEP could benefit more severe ARDS patients. However, opposite trends (higher mortality and longer ventilation) were found in mild ARDS with higher PEEP (despite not powered to be statistically significant).
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…
Fourth, most of the weaning protocols include PEEP ≤ 5 cmH2O as a criterion for readiness to wean. Theoretically, a standardized liberal strategy of higher PEEP could delay weaning in some settings.
bmj.com/content/342/bm…
bmj.com/content/342/bm…
Five, most of the textbooks do not mention the ‘best’ level of PEEP in non-ARDS patients or do it without reference. For example, Kacmarek’s chapter for Egan’s Fundamentals of Respiratory Care suggests a PEEP of 5-8 cmH2O without offering a reference.
derangedphysiology.com/main/cicm-prim…
derangedphysiology.com/main/cicm-prim…
Sixth, the best evidence till the date is from 2008 from a single-center study enrolling 131 patients and comparing 5-8 cmH2O of PEEP against no PEEP. The study was neutral for the primary outcome but suggested a lower incidence of VAP with ‘higher’ PEEP.
journals.lww.com/ccmjournal/Abs…
journals.lww.com/ccmjournal/Abs…
Finally, the balance between benefit and harm of any level of PEEP, could very well depend on the presence and severity of lung injury. Also, non-pulmonary effects like hemodynamic effects should be considered in the selection of the best PEEP in any clinical scenario.
In #RELAx we enrolled 980 mechanically ventilated adults expected not to be extubated within 24 hours. The patients were assigned to a lower PEEP strategy (lowest level below 5 cmH2O to keep SpO2 > 92%) or to a higher PEEP strategy (8 cmH2O) within 1 hour of intubation.
A noninferiority design was chosen because higher levels of PEEP are being increasingly used and are considered standard of care in many settings, despite lack of evidence. It may not be better to use a lower PEEP strategy, but it could be as good as higher PEEP.
The primary outcome was ventilator-free days at day 28, with a noninferiority margin of -10%. Practically, this meant that a difference of less than 12 hours in duration of ventilation or 1.6 ventilator-free days with lower PEEP was considered noninferior.
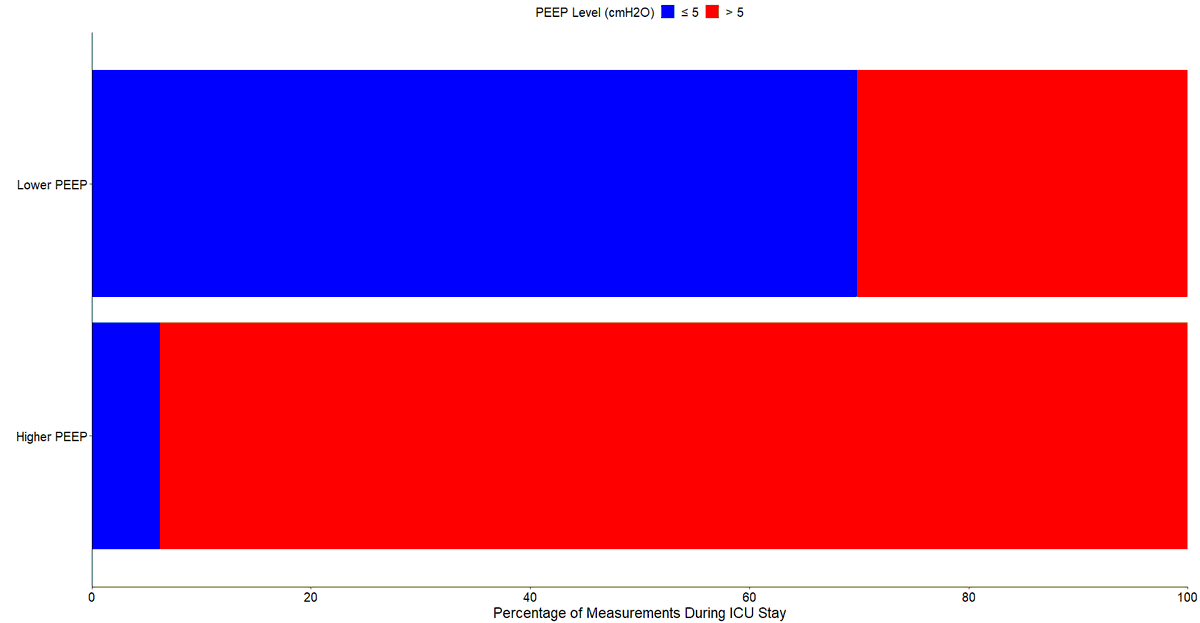
Patients allocated to lower PEEP spent a lot more time in ICU receiving ventilation with PEEP ≤ 5 cmH2O, following the proposed protocol. 
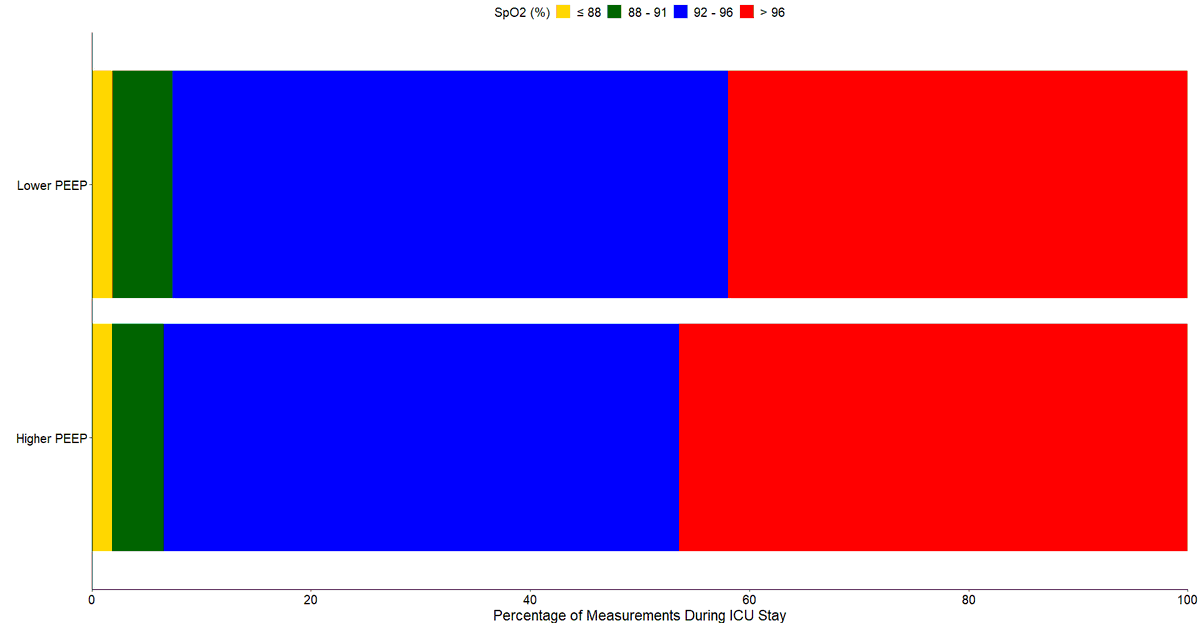
Patients allocated to lower PEEP also spent a little more time with an SpO2 ≤ 96% where they would not be expected to be exposed to hyperoxemia. The time under hypoxemia was similar in both groups. 
An important finding (not included in the paper) is that none baseline characteristic was associated with a higher risk of protocol violation in any of the groups. This means that none of the characteristics assessed can be used as a reason to not consider one of the strategies.
Lower PEEP was noninferior in relation to ventilator-free days at day 28 compared to higher PEEP (mean ratio, 1.04 [95% CI, 0.95 to ∞]; p = 0.007 for non-inferiority). The absolute difference was 0.41 days (95% CI, -1.16 to 1.98).
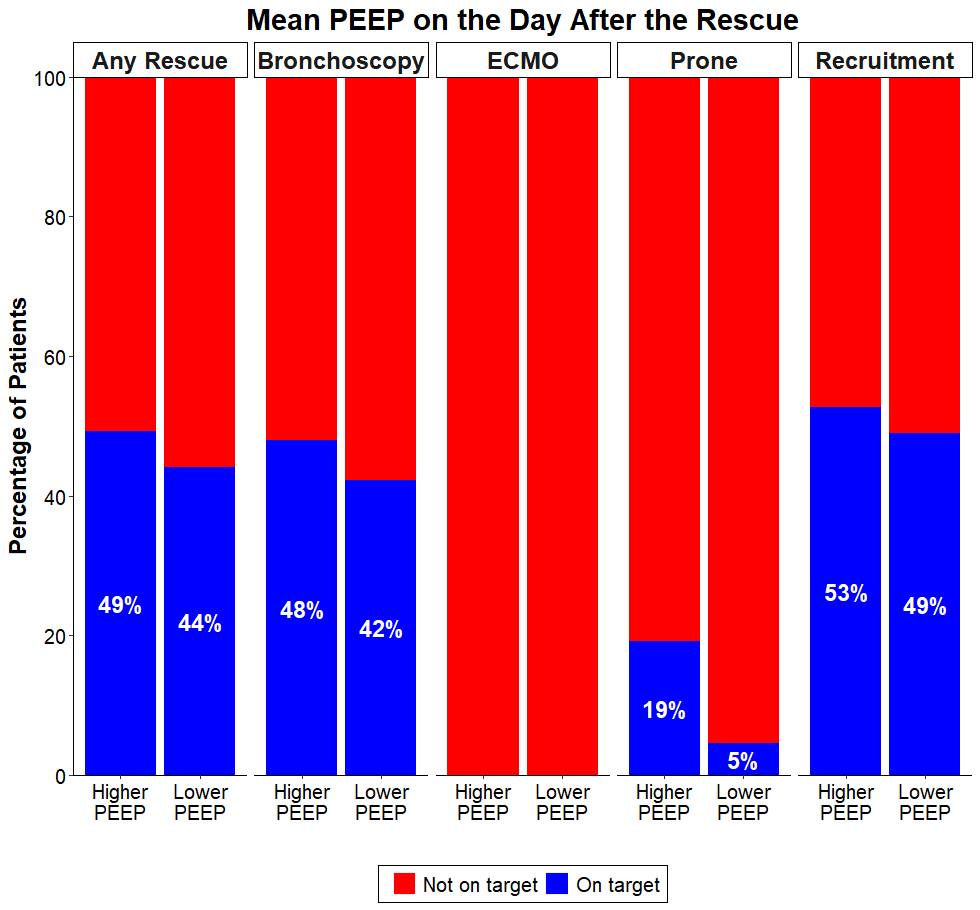
Occurrence of severe hypoxemia was 20.6% vs 17.6% (risk ratio, 1.17 [95% CI, 0.90 to 1.51]; p = 0.99), and need for rescue strategy was 19.7% vs 14.6% (risk ratio, 1.35 [95% CI, 1.02 to 1.79]; p = 0.54) in patients in the lower and higher PEEP group, respectively.
On the day after the need of rescue, it was possible to return the PEEP to the target in 44% and in 49% of the patients in the lower and higher PEEP group, respectively. This was highly dependent on the level of rescue needed. 
At day 28 and day 90, the mortality rate was lower (but not statistically) in lower PEEP group than in higher PEEP group (38.4% vs. 42.0%, and 41.6% vs. 44.3%), for a hazard ratio of 0.89 (95% CI, 0.73 to 1.09), and 0.92 (95% CI, 0.76 to 1.11), respectively.
There was no heterogeneity of treatment effect of lower PEEP on ventilator-free days at day 28 in any of the subgroups assessed.
Some can say that the control (higher PEEP) arm in #RELAx is not the actual practice around the world. Indeed, we do not claim that ventilation using 8 cmH2O of PEEP is standard care. However, this level of PEEP is increasingly used in ICU patients without ARDS.
An important finding of #RELAx is the difference in mortality rate found at day 28 and day 90 (despite not statistically significant). Based on the data distribution, there is a 70% chance that lower PEEP decreases 90-day mortality by more than 1.5% compared with higher PEEP.
As a comparison, the #ICU-ROX, conducted in a similar population and performed by the excellent @DogICUma, found a 46% and a 19.3% chance that conservative oxygen increases or decreases absolute mortality by more than 1.5% compared with usual O2, respectively.
It is important to emphasize that the point estimate for the percentage requiring rescue strategies was greater in the lower PEEP group, and the study may have been underpowered to detect a significant difference favoring higher PEEP group.
However, weighing a probable reduction in the need of rescue against a potential increase in the risk of death with higher PEEP is needed. The NNT to prevent a rescue is 20. Thus, although the uncertainty whether higher PEEP increases mortality, the risks should be considered.
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh


