I believe that if we had spent 1% of the money we are burning on testing to supply everyone over 60 with enough N95s, and let the life to go on as normal, we would have max. 10% of the current mortality.
But we keep insisting on the wrong mode of transmission. (1/x)
But we keep insisting on the wrong mode of transmission. (1/x)
https://twitter.com/covidtweets/status/1333161918085951488
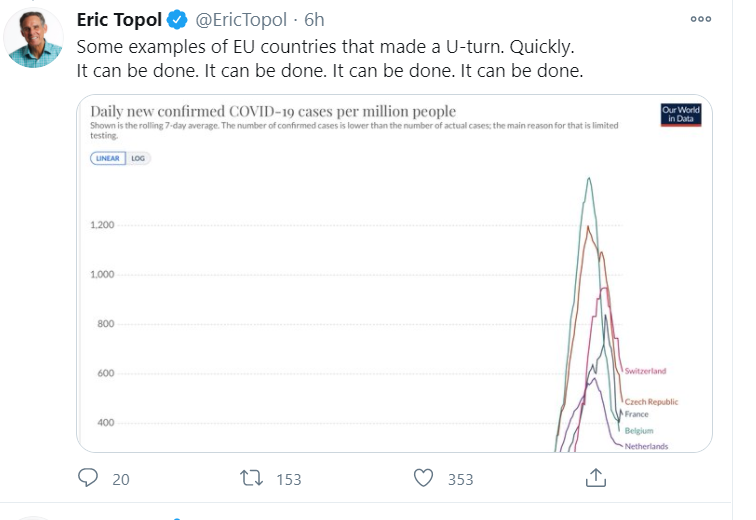
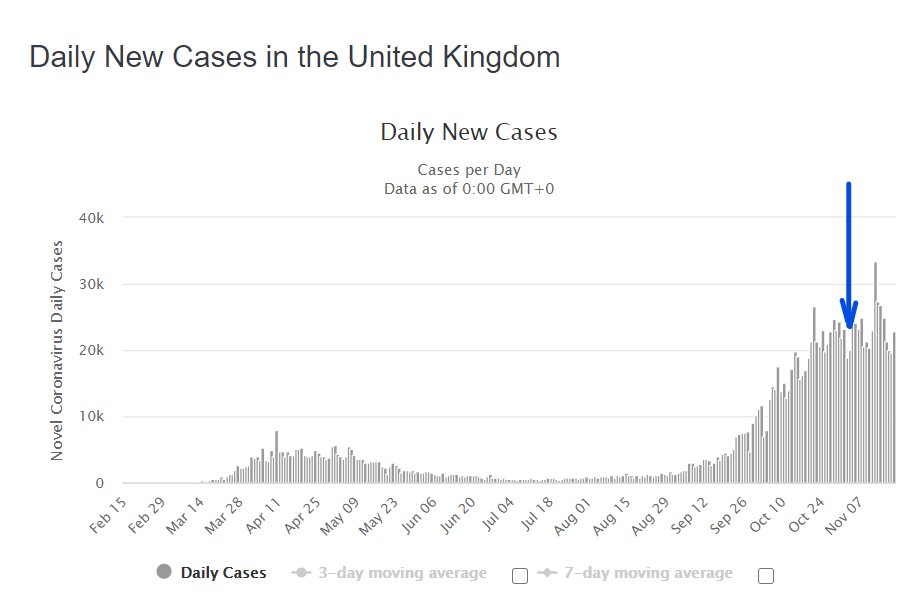
We operate under a droplet model and do the things that should work, like masks, distance, contact tracing. None of those things work - as seen repeatedly since October.
Without any apparent change in human behavior, cases are skyrocketing. (2/x)
Without any apparent change in human behavior, cases are skyrocketing. (2/x)
https://twitter.com/covidtweets/status/1339397851261100033?s=20
I wouldn't be surprised if we one day discover that this virus, like pollens, don't need droplets of any size (not even aerosols) to float in the air, at right temperatures/humidity. Like mold, it stays in the air, and infects when they find the right host environment. (3/x)
Actually, maybe every virus does this, but because our bodies know them, one or two counts are not enough to infect us, and that's why we need larger doses (droplet) to get sick with them.
But when a new pathogen arrives, it is a different ballgame. (4/x)
But when a new pathogen arrives, it is a different ballgame. (4/x)
https://twitter.com/covidtweets/status/1333161937958531080?s=20
Using a way analogy, our defenses are highly effective at killing say 50 invaders if their weapons are well-known.
But one invader with a different weapon can knock our defenses down and get into the body. (5/x)
But one invader with a different weapon can knock our defenses down and get into the body. (5/x)
Since I am not a virologist, I am just speculating here. But nothing other than this virus getting airborne under certain conditions explains these spikes we see in places like LA. When the weather is right, like pollens, it fills the air, infects thousands at once. (6/x)
Obviously, such a discovery would be a public health messaging nightmare, but also would allow us to focus on the right dangers and do the right things instead of wasting our energy.
We would focus on N95s, ventilation, even forecasting... (7/x)
We would focus on N95s, ventilation, even forecasting... (7/x)
For example, imagine we know exactly when the virus is airborne, and like pollen warnings with weather forecasts, we see virus warnings, so at-risk people either stay home or use N95 on those days.
But this would require accepting seasonality and properly researching it. (8/x)
But this would require accepting seasonality and properly researching it. (8/x)
Instead, our messaging denies seasonality and emphasizes close contact settings and droplets.
If the goal is giving people something to do so they don't go insane, it is working. If the goal is reducing spread, its effect is likely negligible. (9/x)
If the goal is giving people something to do so they don't go insane, it is working. If the goal is reducing spread, its effect is likely negligible. (9/x)
I hope this is not too into the "crazy" or "sci-fi" territory.
Again, I am not an expert on these things. But I do have a Ph.D., which means I am probably decent at making observations and digesting data.
Something does not fit... (10/10)
Again, I am not an expert on these things. But I do have a Ph.D., which means I am probably decent at making observations and digesting data.
Something does not fit... (10/10)
• • •
Missing some Tweet in this thread? You can try to
force a refresh