A 🧵on humidity and airborne viruses. Several articles have said that at higher relative humidity (RH), droplets/aerosols retain more water, are larger, and then fall out of the air faster. True, but the effect of RH on biological decay is probably more important. /1
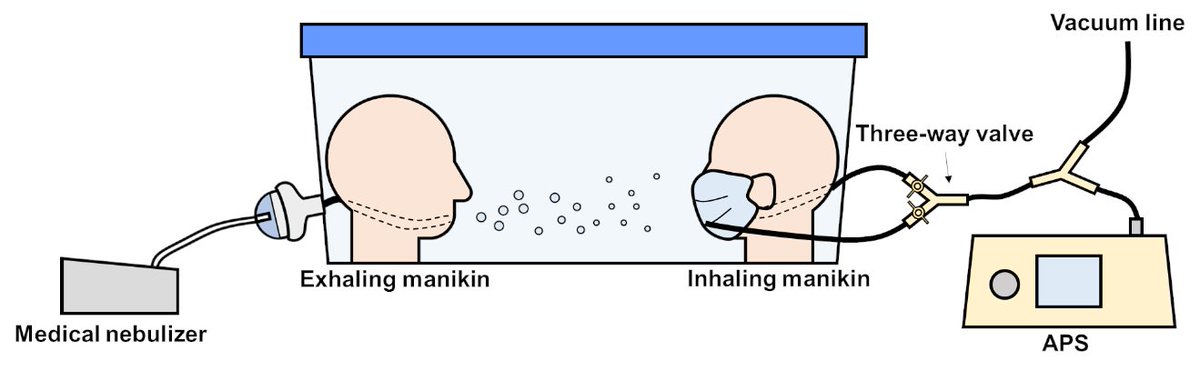
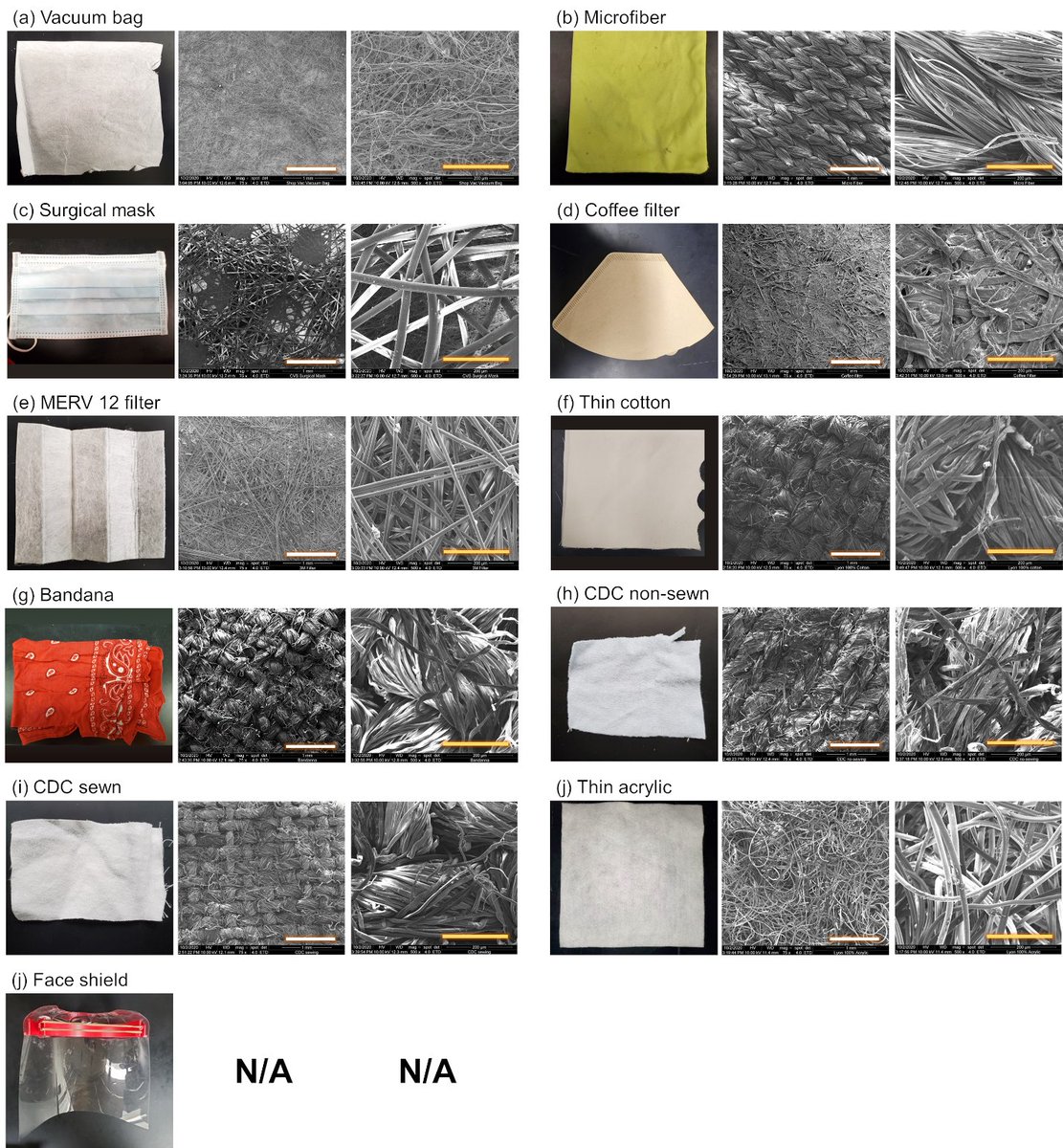
.@DrWanYang and I studied this question in 2011, exploring different removal mechanisms from air as a function of RH. I thought we’d find that at high RH, droplets/aerosols would be a lot larger and settle out quickly. journals.plos.org/plosone/articl… /2
But the biological inactivation rate is more sensitive to humidity. See bigger steps in RH for inactivation than for settling in Fig. 5. We used decay rates for influenza from Harper 1961. Also note the difference ventilation makes at 1 vs. 10 ACH. /3 
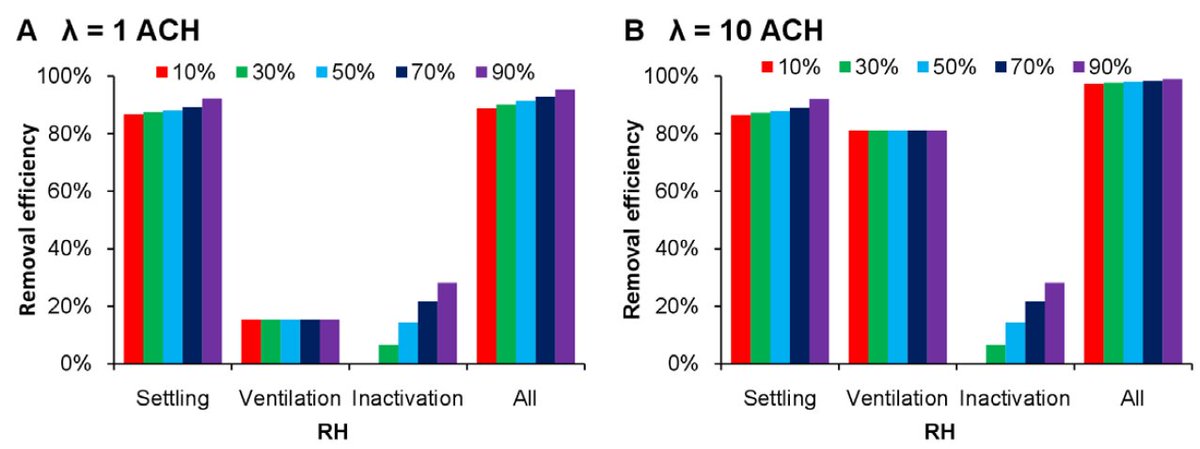
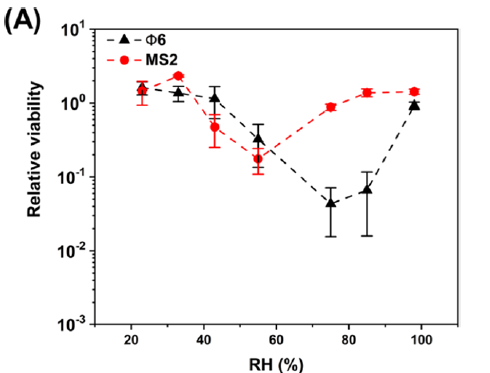
This led us on a 10-year quest to understand virus inactivation in droplets/aerosols, still ongoing. Survival can vary by 2-100x between <20% RH vs. 40-80% RH, usually U-shaped relationship between viability and RH for many viruses. pubs.acs.org/doi/abs/10.102… with @kaisen_lin /4 
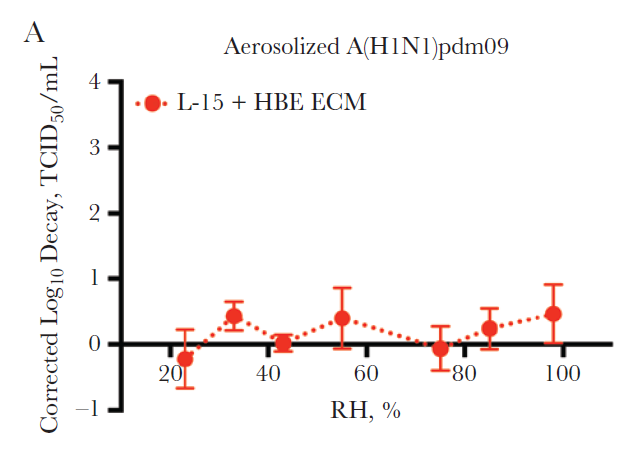
But influenza A (H1N1) 2009 virus in more realistic liquid medium survives well at all RH. academic.oup.com/jid/article/21… with @kaisenlin @LakdawalaLab. Different for other flu strains. msphere.asm.org/content/4/4/e0… /5 
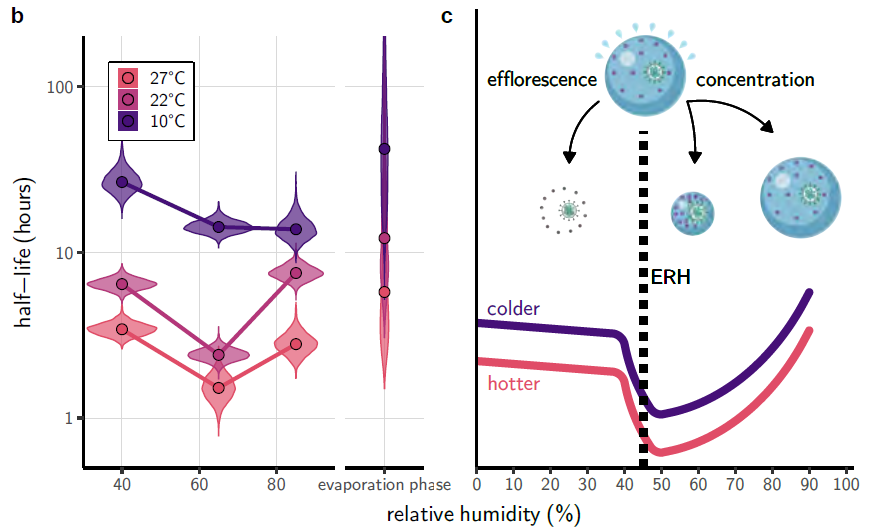
SARS-CoV-2 shows the classic U-shaped relationship between viability and RH that we see with most enveloped viruses in culture media. biorxiv.org/content/10.110… with @dylanhmorris @amandinegamble @qishenhuang @petervikesland Munster Lloyd-Smith others /6 
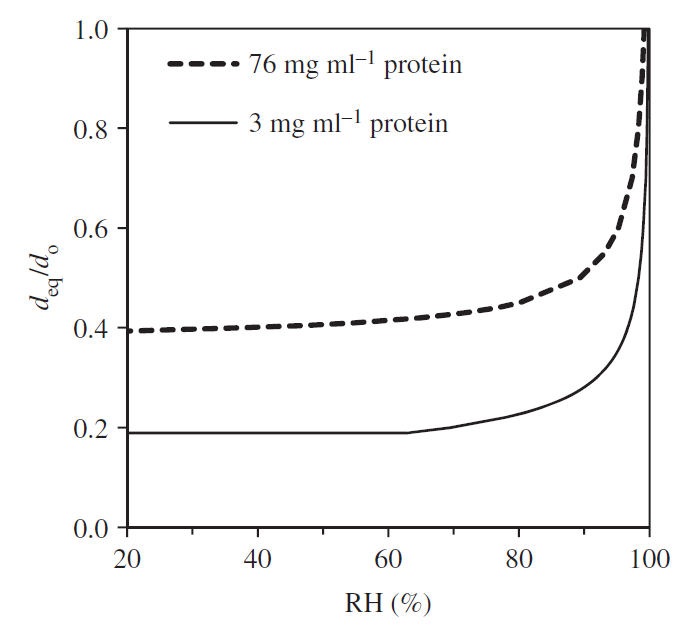
Over the typical range of indoor RH in temperate regions (<80% RH), the evaporated size of aerosols/droplets doesn’t vary much: ratio of equilibrium/initial diameter is mostly flat in Fig. 3. ncbi.nlm.nih.gov/pmc/articles/P… with Tang @LakdawalaLab /7 
At low RH, better virus survival and weakened immune defenses may both contribute to increased transmission, as discussed in a great review by @VirusesImmunity annualreviews.org/doi/10.1146/an… /8
If you decide to humidify, it’s important to stay below 60% so that you don’t promote mold growth and related health problems. /9
Caveats: evaporation rate at different RHs may matter, droplets/aerosols may not reach theoretical equilibrium due to chemical and morphological heterogeneity, we still haven’t identified mechanism of biological decay, more. /10
Oops, meant @Lakdawala_Lab
Wrong paper. I meant to cite this one: journals.plos.org/plosone/articl…
CORRECTION: In tweet #2 of this thread, I meant to cite this paper: journals.plos.org/plosone/articl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh