To date, anecdotal reports from dual entry inhibition in mild acute COVID-19 remain excellent.
Recovery within 48 hours appears typical, absent significant complications (e.g. secondary infection).
Dual entry inhibition means blocking both:
- TMPRSS2/13/11
- endosomal entry
Recovery within 48 hours appears typical, absent significant complications (e.g. secondary infection).
Dual entry inhibition means blocking both:
- TMPRSS2/13/11
- endosomal entry
https://twitter.com/Statins_Kill/status/1343885264800927744
Dual entry inhibition was tested in the Ansarin et al. RCT, adding bromhexine 8mg t.i.d. to a baseline of HCQ 200mg q.d.
Mortality in hospitalized moderate COVID-19 patients fell to zero.
This remains one of the best results of any COVID-19 RCT to date.
Mortality in hospitalized moderate COVID-19 patients fell to zero.
This remains one of the best results of any COVID-19 RCT to date.
https://twitter.com/__ice9/status/1285711393992445952?s=19
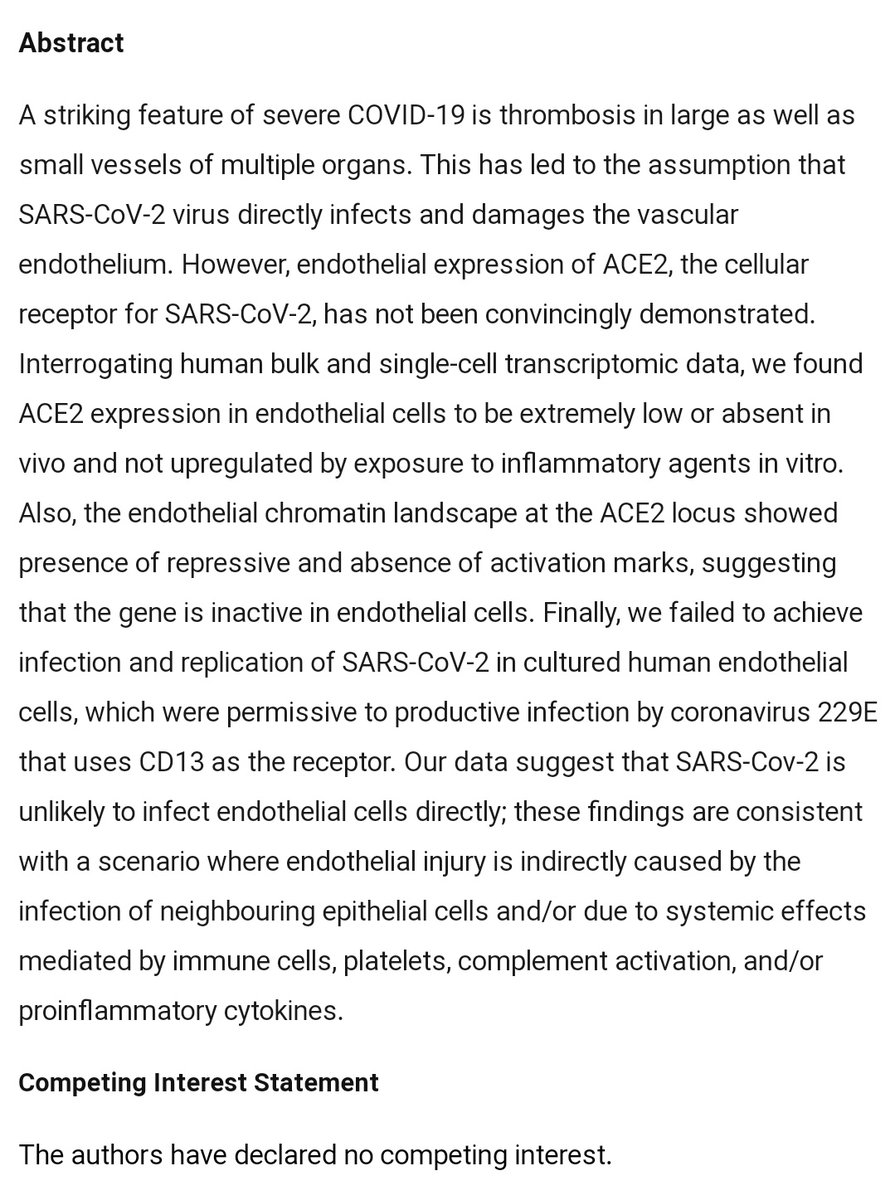
Theoretical justification arises from the fact that endosomal entry is of only secondary importance for SARS-CoV-2 replication in the respiratory tract.
Both TMPRSS (proteases at the cell membrane) and cathepsins (proteases in endosomes) must be blocked.
Both TMPRSS (proteases at the cell membrane) and cathepsins (proteases in endosomes) must be blocked.
https://twitter.com/__ice9/status/1327201071631114240?s=19
This is because most epithelial cells in the lungs, and many in the nasal passages, express TMPRSS2/13/11.
Cells expressing one or more of these TMPRSS isoforms, plus ACE2, are vulnerable to SARS-CoV-2 even in the presence of endosomal entry inhibitors.
Cells expressing one or more of these TMPRSS isoforms, plus ACE2, are vulnerable to SARS-CoV-2 even in the presence of endosomal entry inhibitors.
https://twitter.com/__ice9/status/1298577668506628096?s=19
This is why e.g. HCQ monotherapy failed.
This is why adding HCQ to post-entry antivirals had little further benefit.
Using an endosomal entry inhibitor like HCQ without blocking TMPRSS is like blocking a side door while leaving the main entrance open.
This is why adding HCQ to post-entry antivirals had little further benefit.
Using an endosomal entry inhibitor like HCQ without blocking TMPRSS is like blocking a side door while leaving the main entrance open.
https://twitter.com/__ice9/status/1286650496946708481?s=19
TMPRSS entry is faster than endosomal, so it dominates viral spread across epithelial surfaces.
The chance to enter via TMPRSS is also chronologically prior to endocytosis and cathepsin encounter.
The endosomal route only matters if TMPRSS is blocked.
The chance to enter via TMPRSS is also chronologically prior to endocytosis and cathepsin encounter.
The endosomal route only matters if TMPRSS is blocked.
https://twitter.com/__ice9/status/1320761499112165377?s=19
Other trials for bromhexine alone, or bromhexine paired with additional TMPRSS inhibitors, also had very good results-- but none quite so impressive as bromhexine+HCQ:
https://twitter.com/__ice9/status/1344005030433722368?s=19
Likewise, nitazoxanide monotherapy actually succeeded in RCT, likely because it has post-entry antiviral effects in addition to its ability to block endosomal entry, but the results were not overwhelming.
Both routes should be blocked.
Both routes should be blocked.
https://twitter.com/__ice9/status/1319708065839652865?s=19
Drugs to inhibit TMPRSS:
1) bromhexine or ambroxol - indirect inhibition via pulmonary surfactant factors
2) camostat or nafamostat - small molecule direct protease inhibitors
3) aprotinin or α1 antitrypsin - protein direct protease inhibitors
See:
1) bromhexine or ambroxol - indirect inhibition via pulmonary surfactant factors
2) camostat or nafamostat - small molecule direct protease inhibitors
3) aprotinin or α1 antitrypsin - protein direct protease inhibitors
See:
https://twitter.com/__ice9/status/1289164553603788805?s=19
Anti-androgenic drugs also induce downregulation of TMPRSS2, albeit seemingly not TMPRSS13 or 11 (or at least, there is no indication of any effect on the latter in available literature).
This thread contains many examples:
This thread contains many examples:
https://twitter.com/__ice9/status/1328923130409127941?s=19
Endosomal entry inhibitors:
Buffers: [hydroxy]chloroquine, pyronaridine*, amodiaquine, mefloquine (avoid)
H+ ionophores: nitazoxanide*, niclosamide*, some vet drugs (ignore)
PIKfyve: apilimod
TPC2: tetrandrine
Cathepsin: teicoplanin, quercetin*
PPIs: weak
* also post-entry
Buffers: [hydroxy]chloroquine, pyronaridine*, amodiaquine, mefloquine (avoid)
H+ ionophores: nitazoxanide*, niclosamide*, some vet drugs (ignore)
PIKfyve: apilimod
TPC2: tetrandrine
Cathepsin: teicoplanin, quercetin*
PPIs: weak
* also post-entry
Essentially any safe combination of at least one TMPRSS inhibitor and at least one endosomal entry inhibitor, at a sufficient dose, will confer dual entry inhibition.
Examples:
TMPRSS:
- bromhexine 8-32mg t.i.d.
- ambroxol 15-50+mg t.i.d.
- camostat 200mg t.i.d. (not ideal but cannot go higher)
Endosomal:
- HCQ 200-400mg b.i.d.
- nitazoxanide 600-1200mg t.i.d.
- niclosamide 1000mg b.i.d. (preferably crushed)
- pyronaridine 720mg q.d.
TMPRSS:
- bromhexine 8-32mg t.i.d.
- ambroxol 15-50+mg t.i.d.
- camostat 200mg t.i.d. (not ideal but cannot go higher)
Endosomal:
- HCQ 200-400mg b.i.d.
- nitazoxanide 600-1200mg t.i.d.
- niclosamide 1000mg b.i.d. (preferably crushed)
- pyronaridine 720mg q.d.
When I was ill earlier, I also included dual entry inhibition in the set of medications used.
I began at below-optimal doses and added sequentially at first, both for conservation and to gauge side effects.
Symptoms abruptly disappeared 36 hours later.
https://twitter.com/__ice9/status/1316112583754158088?s=19
I began at below-optimal doses and added sequentially at first, both for conservation and to gauge side effects.
Symptoms abruptly disappeared 36 hours later.
One important point:
Bromhexine and ambroxol based medications are not available in the United States.
They are commonly present in OTC cough syrups and cold medications in most other countries.
I strongly recommend buying some in advance. Now.
eBay and Etsy e.g. sell them.
Bromhexine and ambroxol based medications are not available in the United States.
They are commonly present in OTC cough syrups and cold medications in most other countries.
I strongly recommend buying some in advance. Now.
eBay and Etsy e.g. sell them.
• • •
Missing some Tweet in this thread? You can try to
force a refresh