I agree with this. Part of the problem, though, is many of us have symptoms that our primary care doctor isn’t comfortable with. I’ve gone to urgent care before only to be sent to the ER. Eventually you learn that you are supposed to go home and “live with it” until you die.
https://twitter.com/Doug_Lind_Say/status/1345795761859137538
There is no place in the medical system for people living with dangerous (but not immediately life-threatening) symptoms. Many of us need hospital admission, testing, and observation, but that essentially never happens.
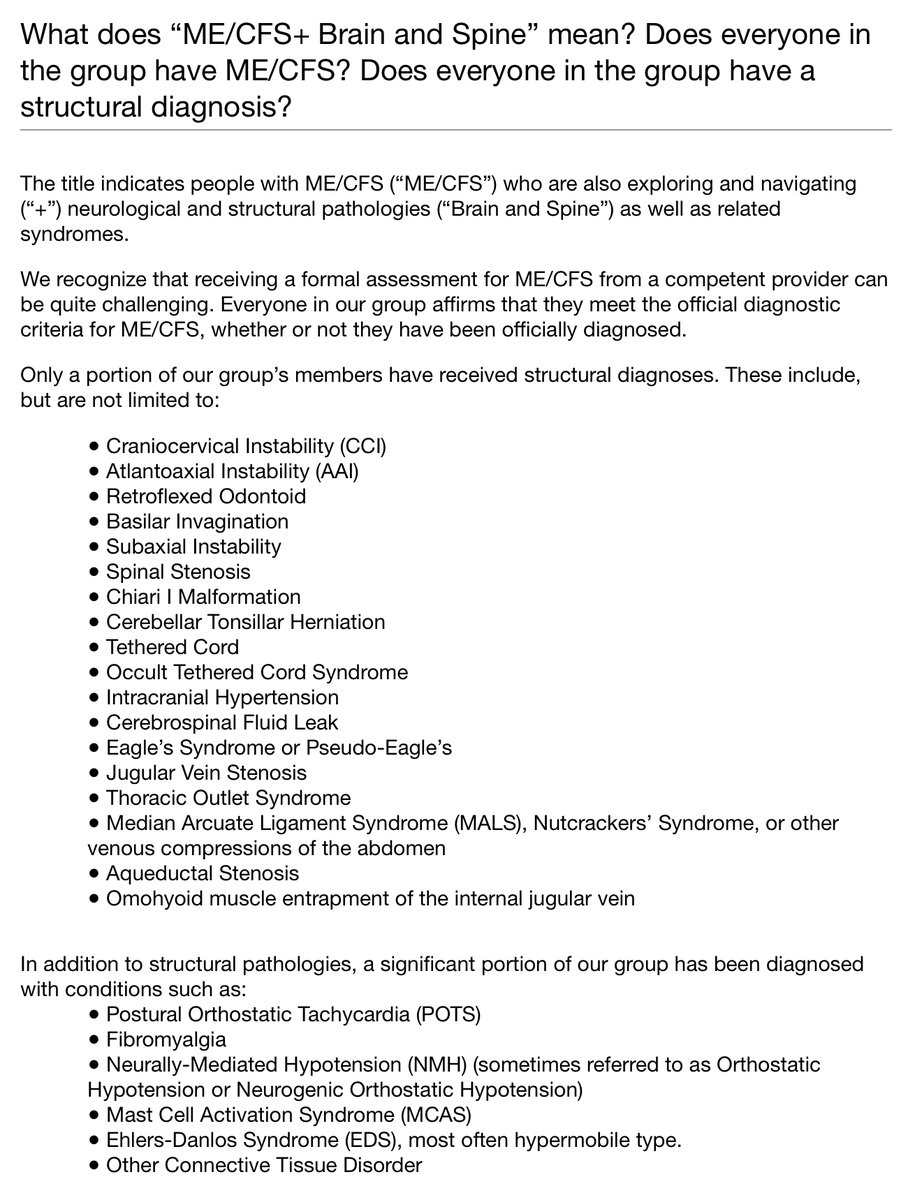
I am sure there are other examples, but if you have Chiari, CCI/AAI, and/or occult tethered cord causing intermittent paralysis, severe central apnea/Ondine’s curse, dysphagia, blackouts, the ER will not take you. Neurology will not treat you. You can die, but you probably won’t.
I have a friend with a severe, genetic metabolic disorder. It took years upon years to diagnose and she had to get lucky—her labs appear abnormal only within a small window of time around her life-threatening episodes.
She’d been to the ER many times but was only diagnosed on the Nth trip. She still has to go to the ER for emergency intervention from time to time, and carries a letter explaining her diagnosis, but has to fight disbelief ALL THE TIME.
“Trust me,” if you don’t give me this intervention I could die. See this note written by my doctor who is a professor at a top 5 academic hospital.
We as patients must become better advocates for ourselves and must learn how to better use/access the system—we have no choice. But we/our behavior are not the problem.
• • •
Missing some Tweet in this thread? You can try to
force a refresh