If you want to come up with a prior* for the possible long-term dynamics of SARS-CoV-2, there are two recent papers that I think are useful...
(*Prior: en.wikipedia.org/wiki/Prior_pro…) 1/
(*Prior: en.wikipedia.org/wiki/Prior_pro…) 1/
First, this pre-print by @eguia_rachel & @jbloom_lab showing that the seasonal coronavirus 229E can undergo 'antigenic drift' to partially escape immunity over time. biorxiv.org/content/10.110… 2/
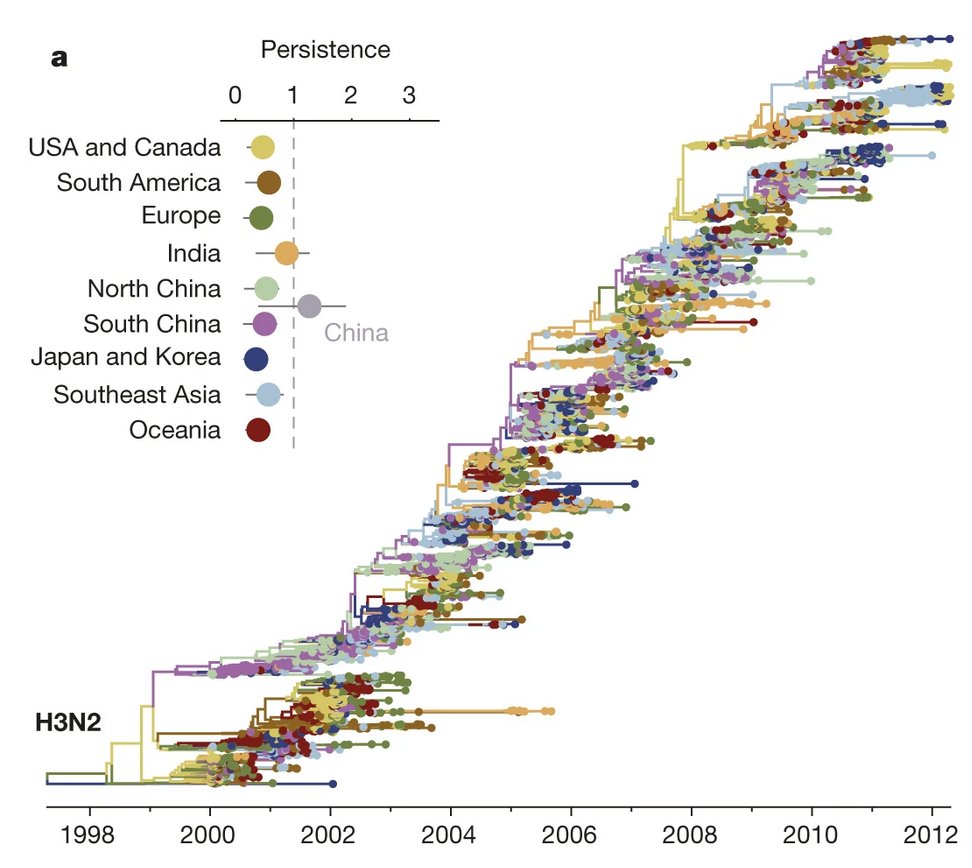
As with influenza, they find a 'ladder-like' phylogenetic tree, suggesting that new variants emerge, become dominant, then are gradually replaced by subsequent new variants. (Influenza A/H3N2 below right from: nature.com/articles/natur…) 3/ 

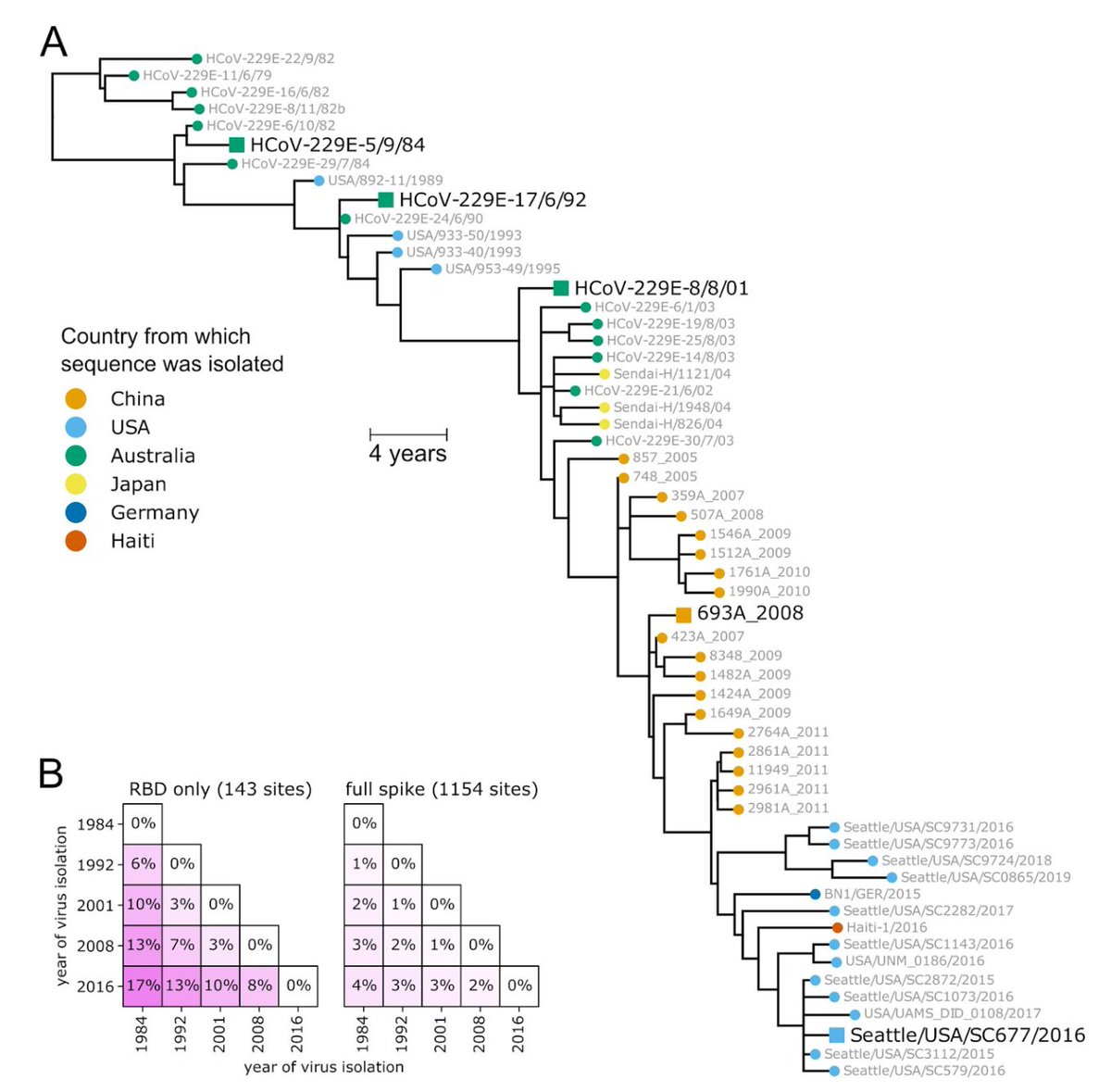
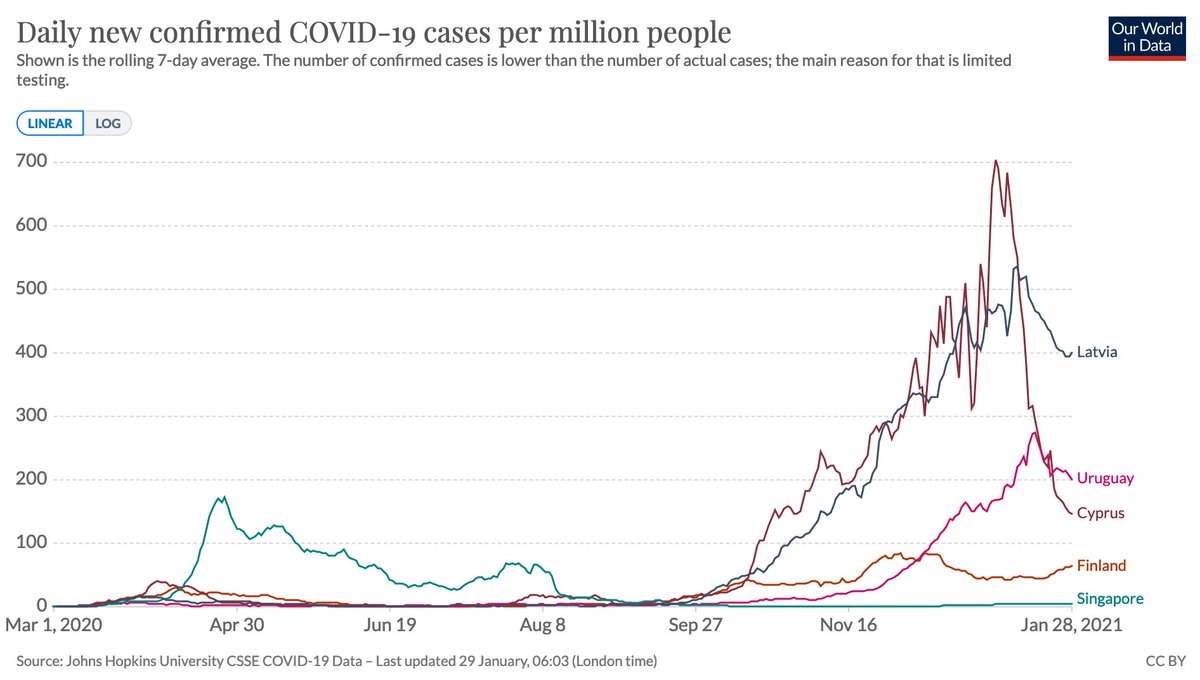
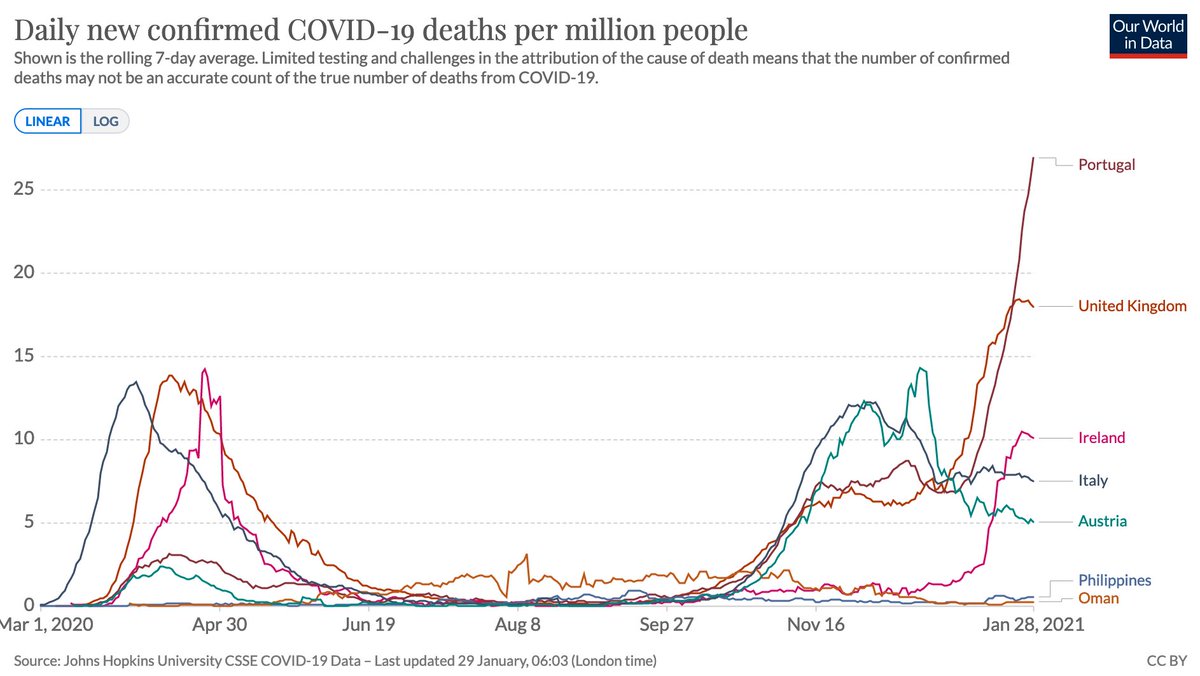
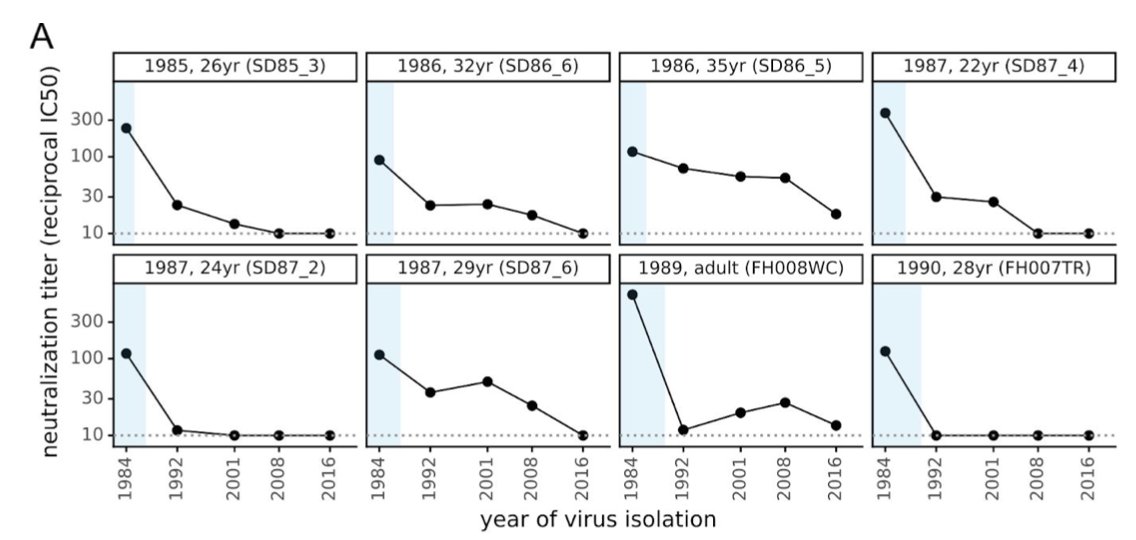
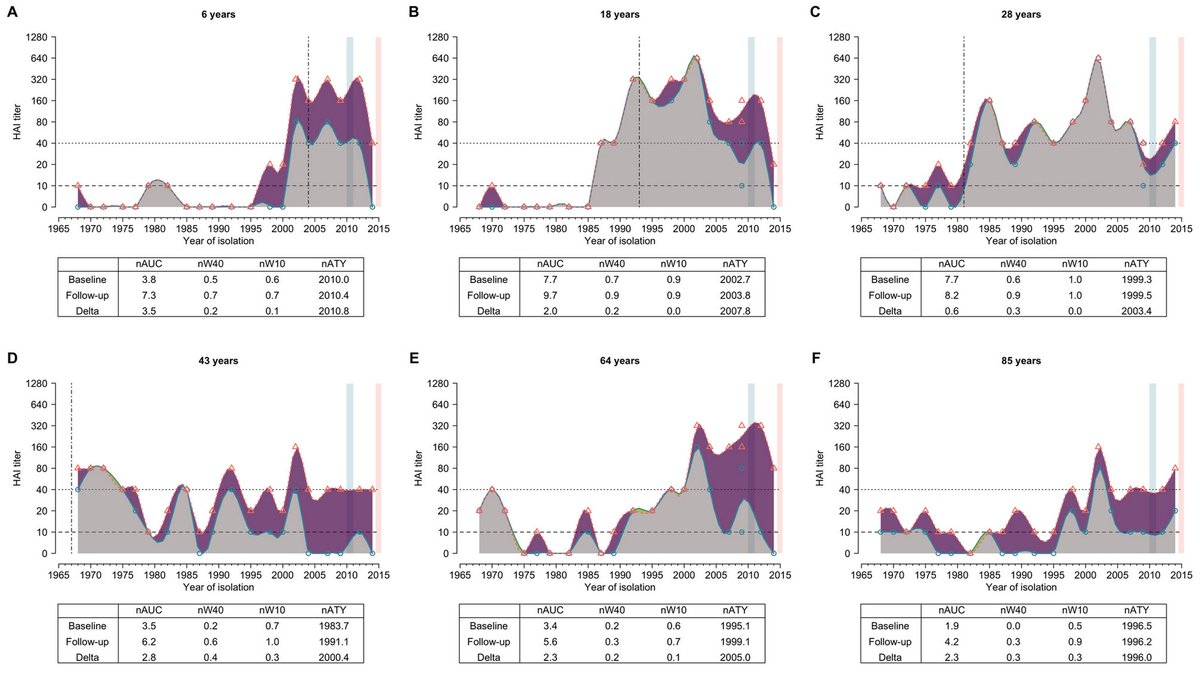
Likewise, they find antibodies in historical samples are progressively less effective against more recent viruses (below left), much like flu responses are less effective against strains that circulated before individuals were born (below right, from journals.plos.org/plospathogens/…) 4/ 

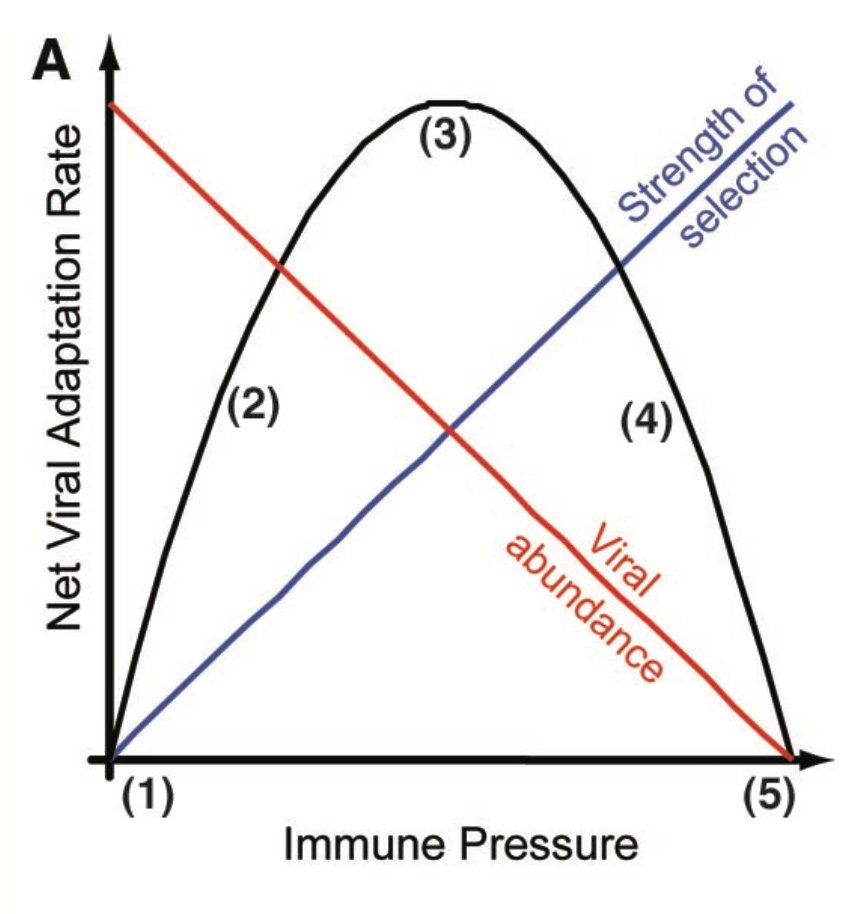
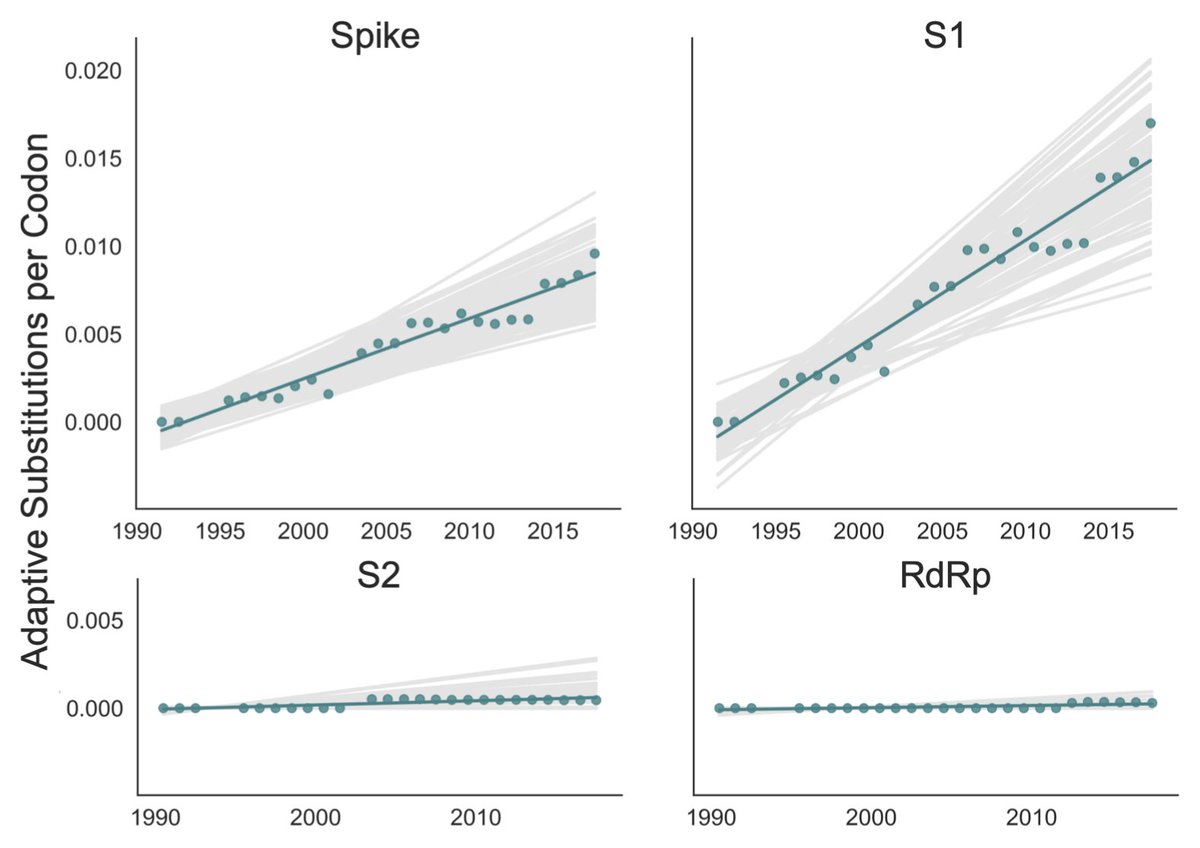
Second, it's worth reading this paper by Katie Kistler and @trvrb, which provides evidence of adaptive evolution in spike protein of two seasonal coronaviruses (OC43 and 229E), as we'd expect if virus was undergoing antigenic drift. elifesciences.org/articles/64509 5/ 
Like influenza, it's therefore plausible that vaccine updates will be needed in long-term to ensure good immune responses against circulating viruses. The frequency of updates will depend on rate of evolution, waning, and how well vaccines prevent disease for new variants. 6/
Finally, reposting this thread by @michaelmina_lab as a reminder that although we have much to learn about SARS-CoV-2, we shouldn't view antigenic evolution as a totally new evolutionary or immunological problem that we have no understanding of. 7/7
https://twitter.com/michaelmina_lab/status/1315861702433480704?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh