
Welcome to this weeks #ResusciTuesdays. We will be learning about REBOA in medical cardiac arrest. REBOA stands for ‘Resuscitative Endovascular Balloon Occlusion of the Aorta’. Its aim is to occlude the aorta and therefore improve blood flow to the brain and coronary vessels. 

REBOA is sometimes talked about alongside other interventions in cardiac arrest such as ECMO and SAAP (Selective Aortic Arch Perfusion - learn more here: intensivecarenetwork.com/selective-aort…). In this we will just be talking about simple balloon occlusion.
In Trauma, REBOA is used by some services to prevent exsanguinating haemorrhage. There is still a lot of ongoing debate about its use in Trauma, but it has been incorporated into clinical practice in places and there are ongoing trials such as @UKREBOATrial 
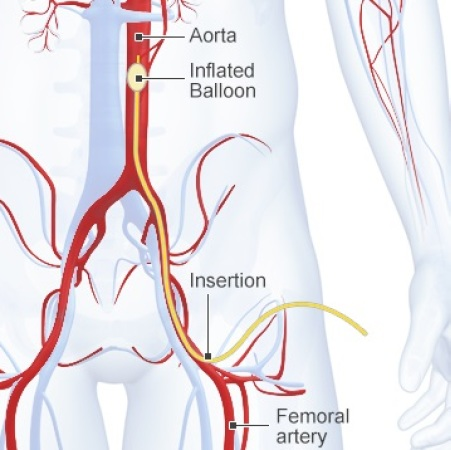
There are two different levels at which the aorta may be occluded. Zone 1 (above the coeliac axis) and Zone 3 (at the bifurcation of the aorta). Zone 1 occludes blood flow to all sites below the diaphragm whereas zone 3 only occludes lower limb and pelvic vessels. 

The possible benefits of REBOA in medical arrest are clear. Occluding the aorta will lead to improved perfusion of the heart, possibly improving the chance of ROSC and improved perfusion of the brain will decrease the risk of ischaemic brain injury.
However, there are also drawbacks. After a cardiac arrest, patients often suffer from ischaemia to distal organs. This will be exacerbated if REBOA is used. This case series from @LDNairamb showed high rates of occlusive lower limb thrombus after REBOA. website60s.com/upload/files/v…
So we know how it works and we know that its use in exsanguinating haemorrhage is being investigated. But what about medical cardiac arrest? What evidence do we have? Is there ANY evidence available? And how can we begin to improve the evidence base?
Well firstly there is very little evidence. There is no RCT or systematic review. So we have to work with what we have. To understand the evidence available, we need to understand a few of the proxy values that are used in cardiac arrest research to predict outcomes.
One of these is the Cerebral Perfusion Pressure (CPP) which essentially tells you how much blood is getting to the brain. It is calculated as CPP=MAP-ICP. If we deploy a balloon in the aorta then the blood to the brain increases as we increase the MAP in the proximal vessels.
Another key value is the coronary blood flow. This is important as it prevents ischaemia to the heart which prevents long term damage and has been shown to increase the likelihood of a successful shock from a defibrillator.
In a study where swine were induced into a VF cardiac arrest and REBOA was placed, it was found that the CPP increased by 60% and the coronary blood flow increased by 8.5%. pubmed.ncbi.nlm.nih.gov/31121206/ Although this is not in Humans, we would expect to see similar results.
The question is whether this corresponds to an increase in ROSC and survival. This study does not take into account the impact of distal organ ischaemia so cannot be used to influence clinical practice, but it does lay the groundwork for human trials.
There are a small number of case reports of REBOA in human non-traumatic cardiac arrest. The first of these was from 1996 where 2 patients had a cardiac arrest with an IABP in-situ and so this was continuously inflated to achieve complete aortic occlusion. pubmed.ncbi.nlm.nih.gov/8959773/
The largest case series to date from from a Norwegian HEMS service who utilised REBOA in 10 medical cardiac arrests. Six of the ten patients achieved a ROSC and one survived to hospital discharge. pubmed.ncbi.nlm.nih.gov/31707942/
It is therefore clear that there is more evidence needed before REBOA can be effectively utilised in non-traumatic arrest. But what form can we expect this evidence to take?
Well the @UKREBOATrial will provide evidence on the use of REBOA for exsanguinating haemorrhage. It may provide some helpful evidence on the risk of ischaemic complications which can be applied to cardiac arrest patients as both groups are in a low flow state.
There will also likely initially be some feasibility studies looking at whether there are enough patients presenting to hospital (or prehospital services) who may benefit from this intervention, and if so whether there are any unforeseen complexities in implementing this.
If it seems that there may be a role for REBOA in medical arrest and there are no apparent unforeseen complexities then further studies such as RCTs taking place which will give us the real answers about its efficacy.
But for now as there is not enough evidence available it is difficult to support its use outside of a research setting.
We hope you enjoyed this #ResusciTuesdays tweetorial! If you don’t already follow us then be sure to hit that follow button for more content like this, plus information about the upcoming ERC congress and information about webinars to further your resuscitation knowledge!
• • •
Missing some Tweet in this thread? You can try to
force a refresh






