CONFLICTING DATA:
-SARS-CoV-2 variants mutate & evade immune system & cause huge epidemics via re-infection (nytimes.com/2021/03/01/hea…) @nmrfaria
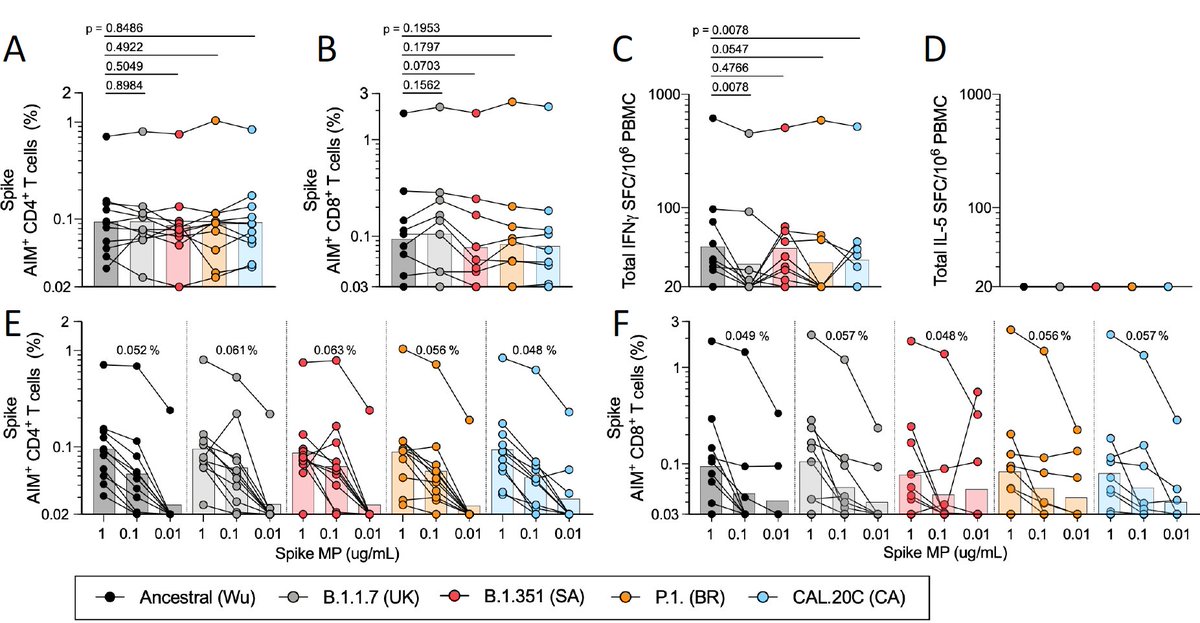
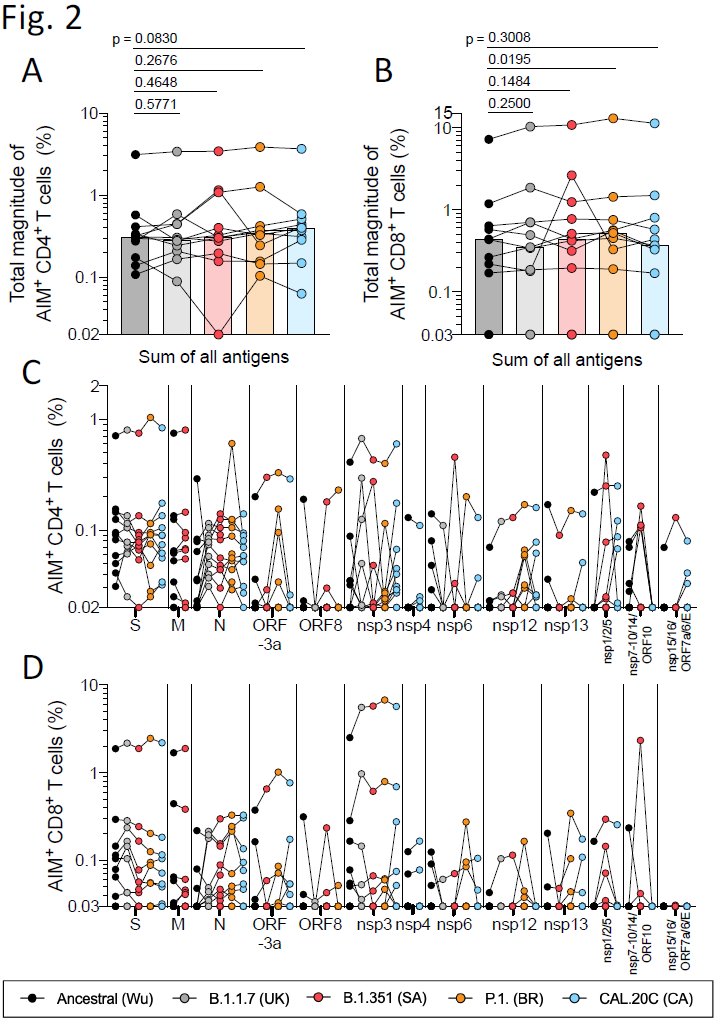
-T-cells play key role in disease severity & are robust to same mutations
@SetteLab @profshanecrotty
-SARS-CoV-2 variants mutate & evade immune system & cause huge epidemics via re-infection (nytimes.com/2021/03/01/hea…) @nmrfaria
-T-cells play key role in disease severity & are robust to same mutations
https://twitter.com/Alba_Grifoni/status/1366773272520519681@aetarke
@SetteLab @profshanecrotty
Background
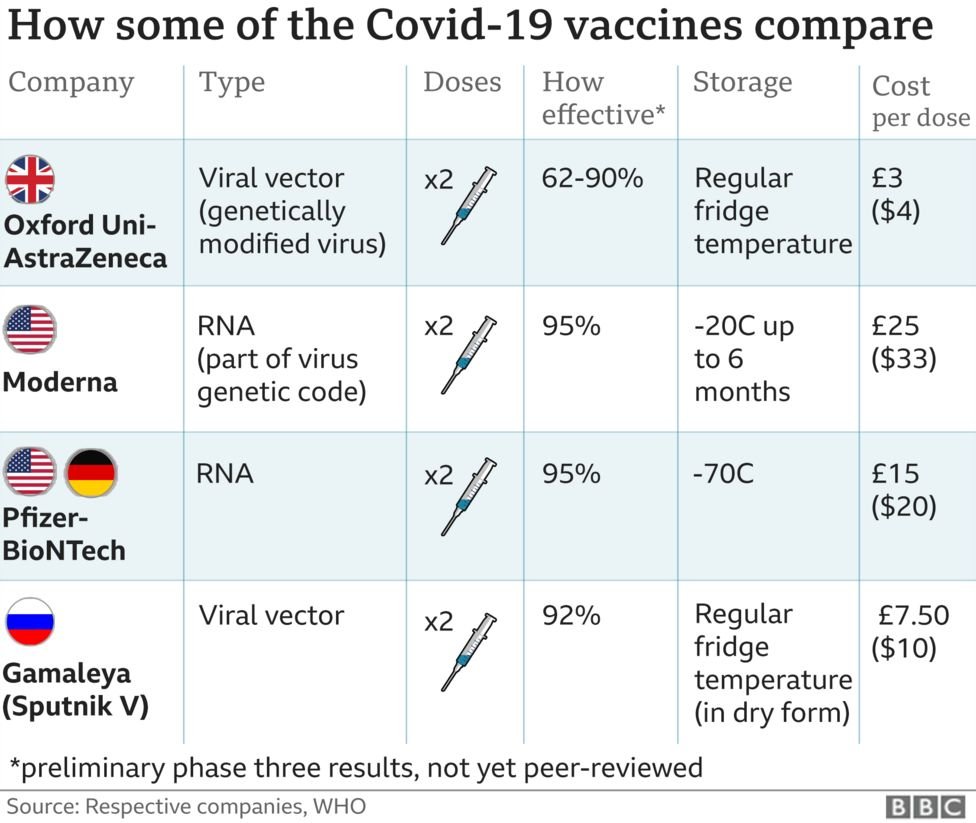
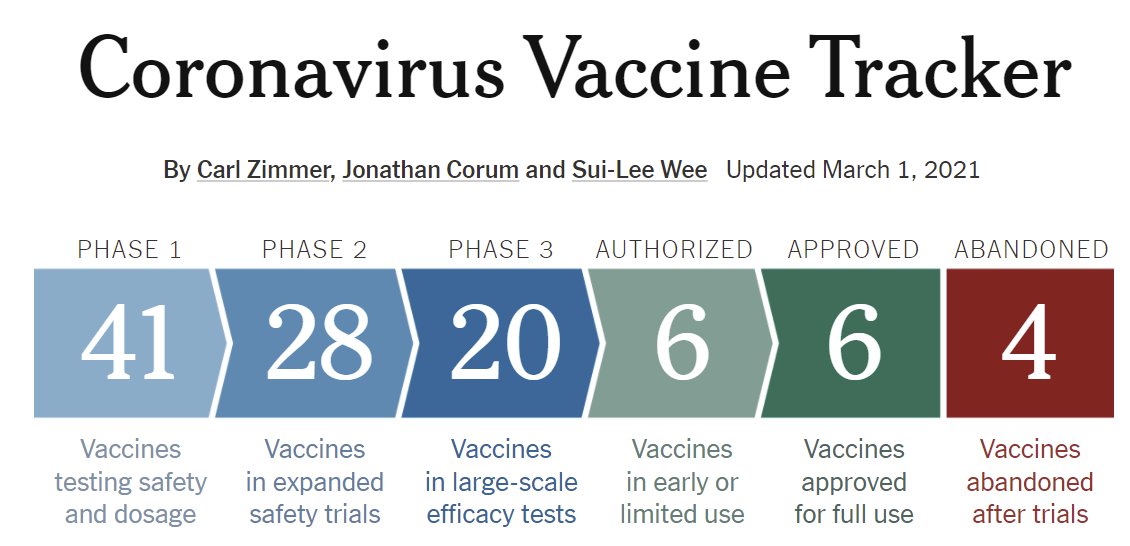
With waves of cases subsiding & development of many vaccines for COVID-19, many hoped we'd be past the worst of the pandemic (at least those countries w/ access to vaccines).
nytimes.com/interactive/20…
With waves of cases subsiding & development of many vaccines for COVID-19, many hoped we'd be past the worst of the pandemic (at least those countries w/ access to vaccines).
nytimes.com/interactive/20…
New SARS-CoV-2 virus variants have thrown a potential monkey wrench in that optimism.
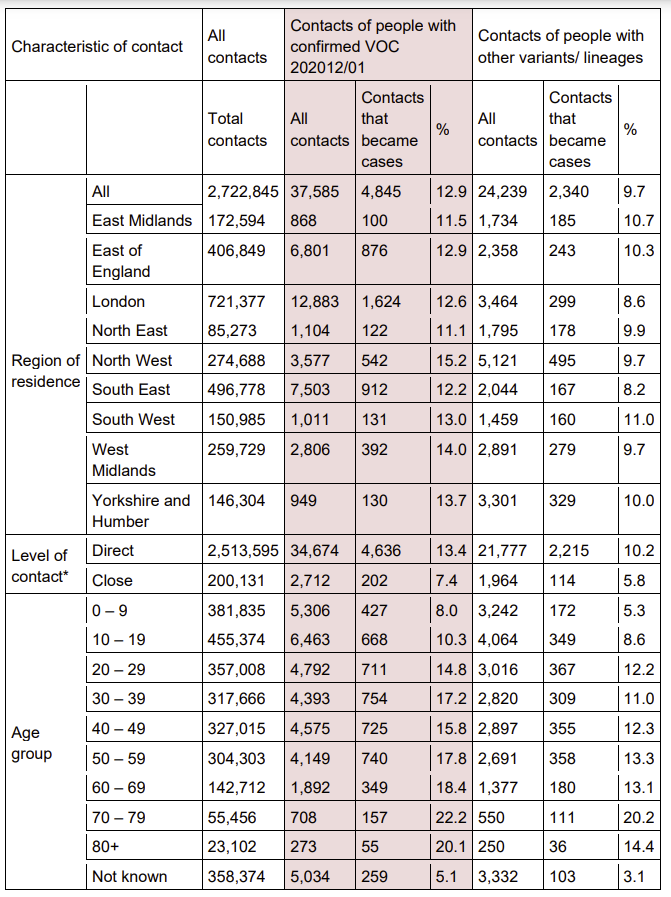
One variant (B.1.1.7) is both more transmissible (medrxiv.org/content/10.110…) & more deadly (medrxiv.org/content/10.110…).
One variant (B.1.1.7) is both more transmissible (medrxiv.org/content/10.110…) & more deadly (medrxiv.org/content/10.110…).
Controlling B.1.1.7 requires more severe restrictions until we can vaccinate & reach higher fraction immune required to keep transmission of this variant in check, Rt<1. Thankfully, vaccines (& nAb) seem to be nearly equally effective against this variant. medrxiv.org/content/10.110…
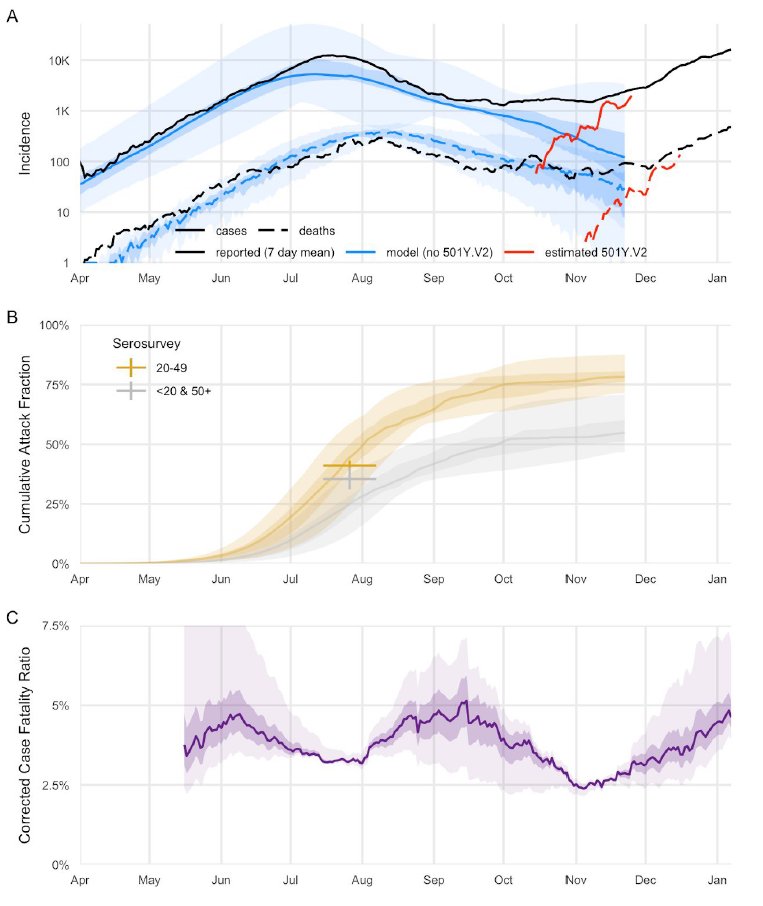
2 other variants (B.1.351, P.1) have increased in frequency in S Africa & Brazil. The reasons for their spread aren't clear b/c the only epidemiological data currently available is rate & timing of spread.
For B.1.1.7 we also had increased s attack rates: assets.publishing.service.gov.uk/government/upl…
For B.1.1.7 we also had increased s attack rates: assets.publishing.service.gov.uk/government/upl…
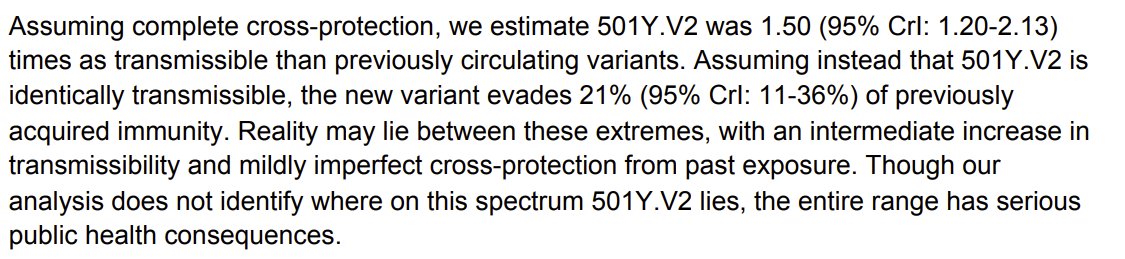
For S Africa, data are consistent either w/ 50% increased transmissibility or 21% increased immune evasion (ability to infect those w/ immunity from previous infection) or combination of these 2. @cap1024
cmmid.github.io/topics/covid19…

cmmid.github.io/topics/covid19…
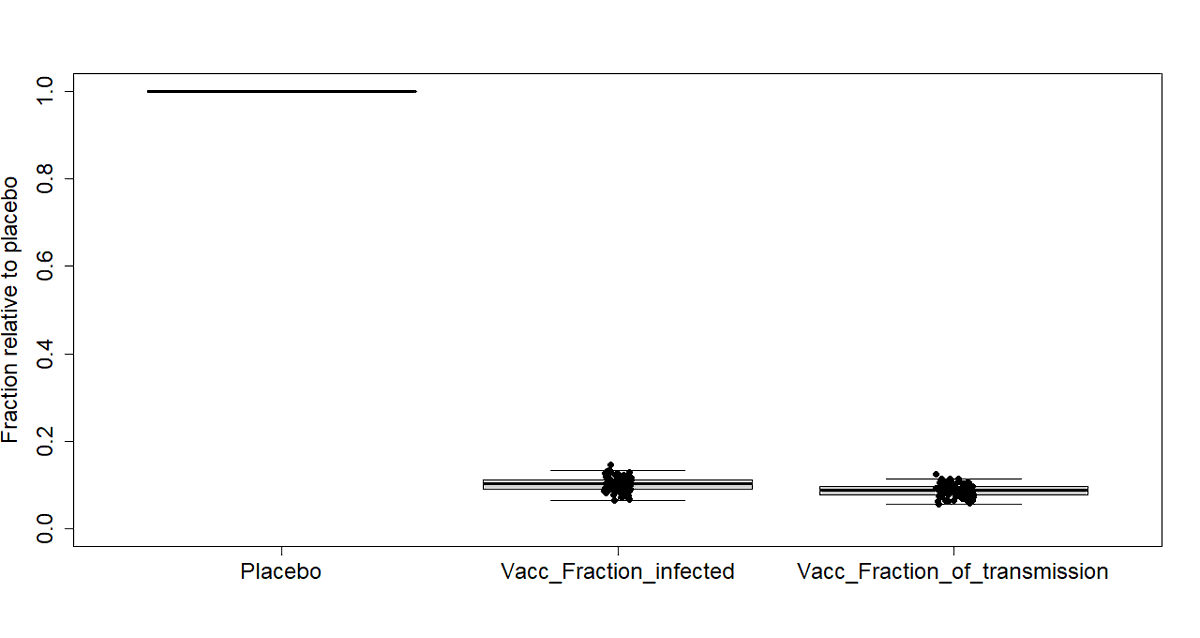
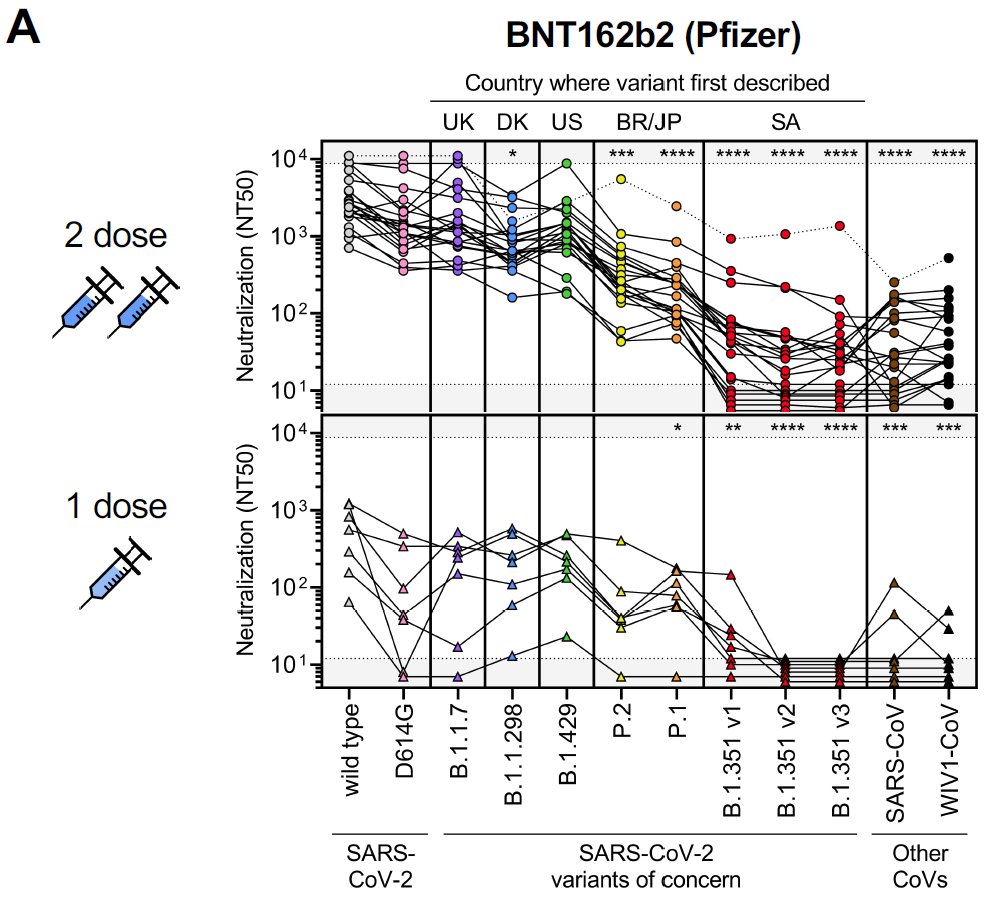
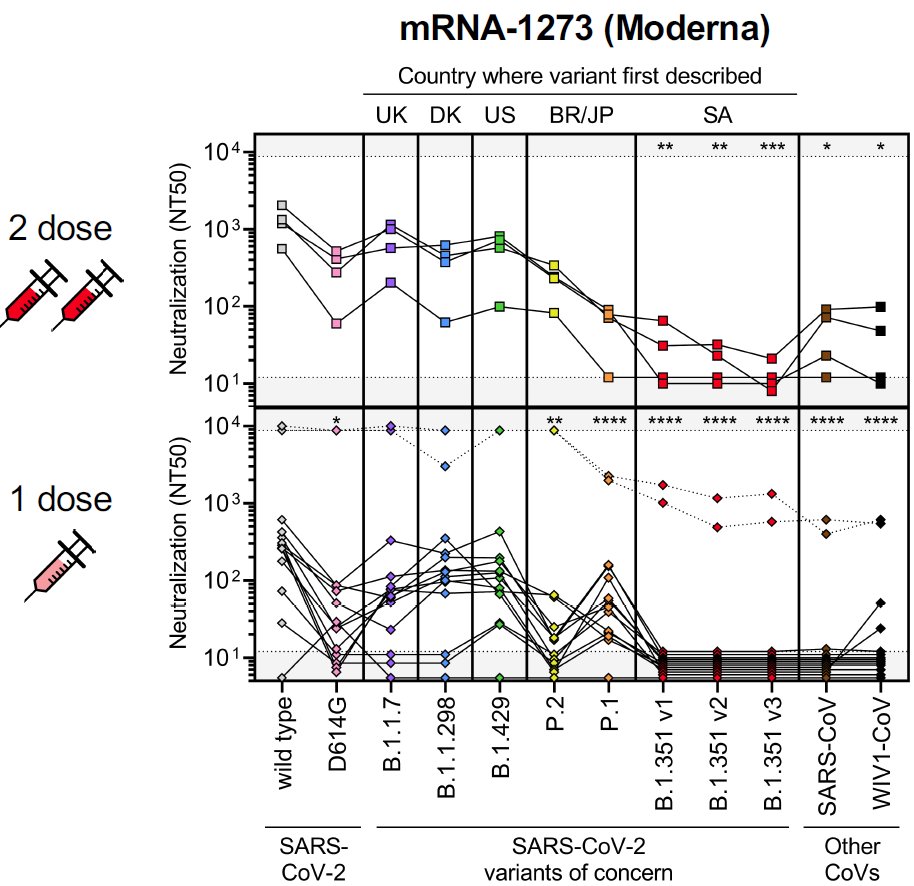
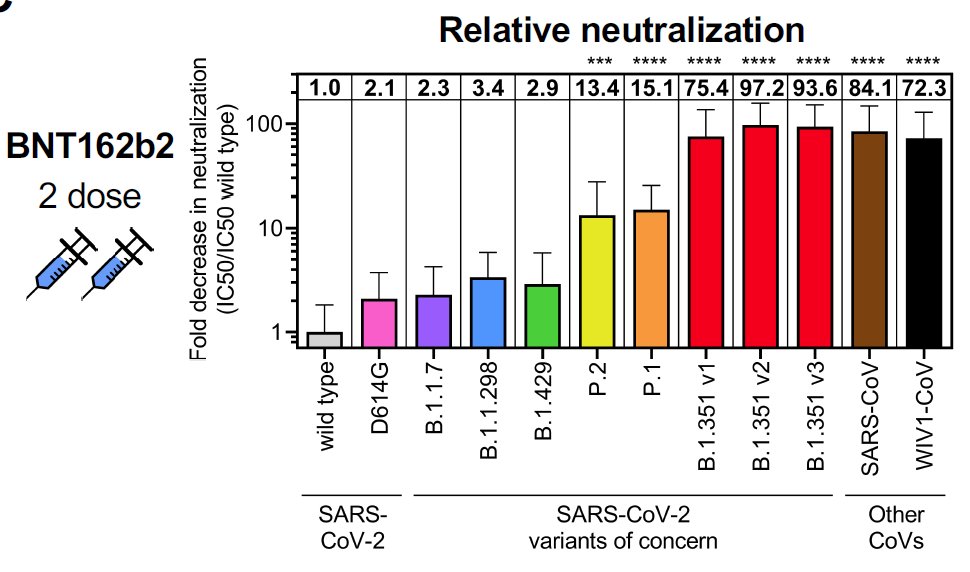
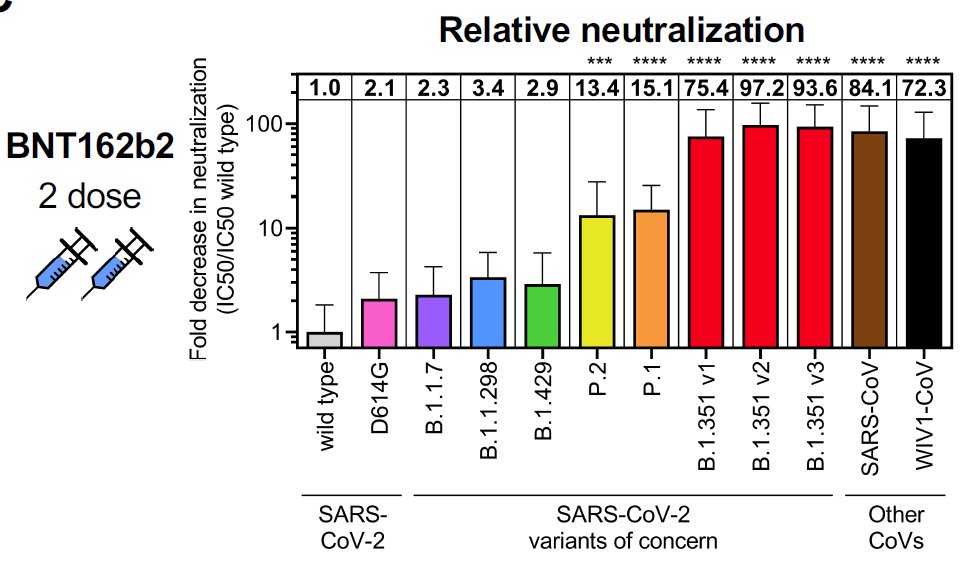
Neutralizing antibody (nAb) studies (here, from vaccinated sera) indicate 75-100 fold reduction in neutralization, suggesting that immune evasion is at least partially contributing to increased spread of variant.
medrxiv.org/content/10.110…


medrxiv.org/content/10.110…
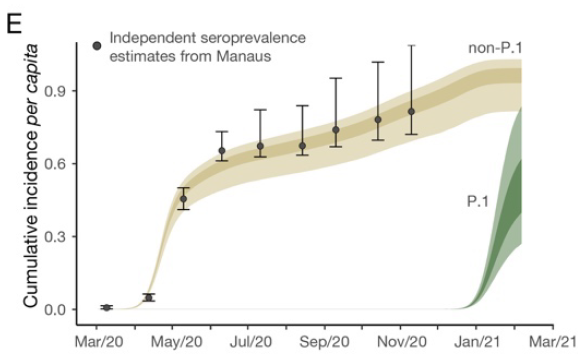
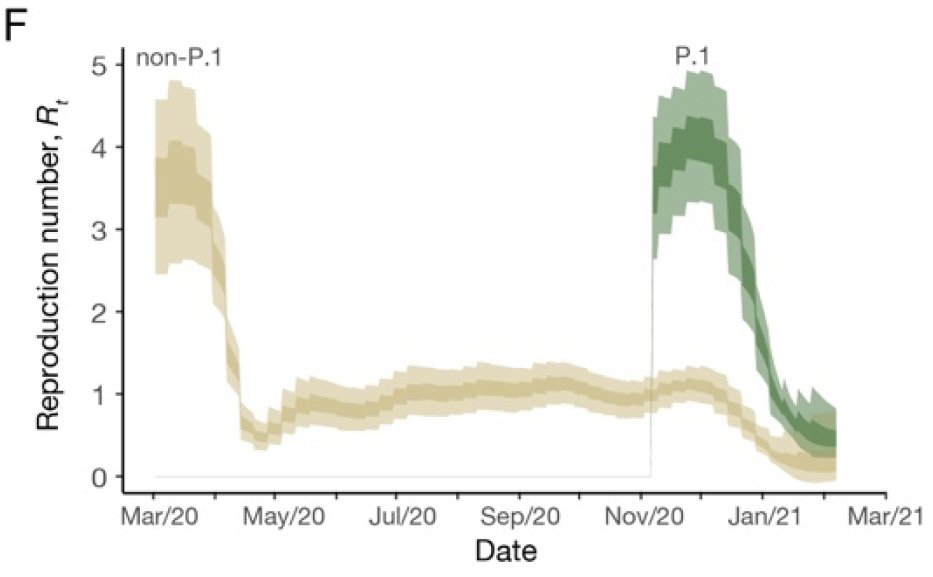
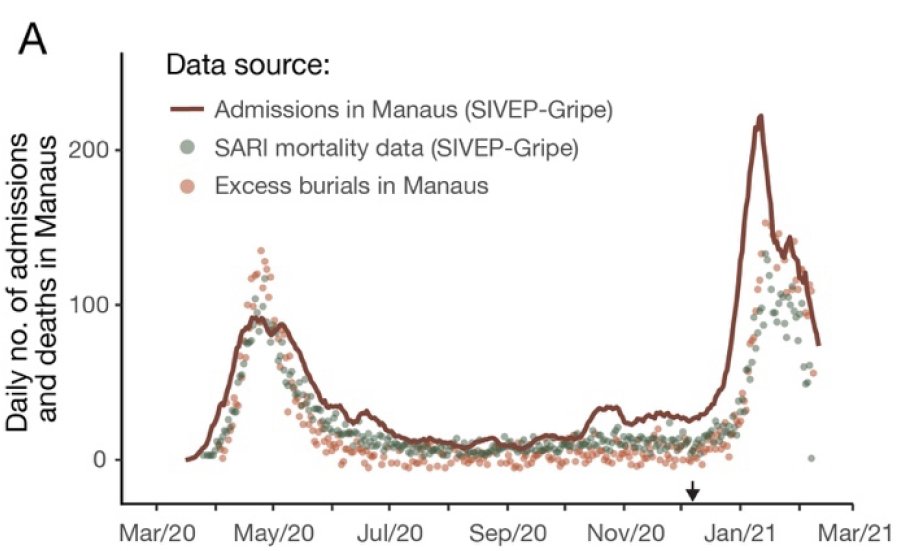
In Brazil P.1 is either 40-120% more transmissible OR evades 25-61% of immunity (& MAY be 10-80% more deadly) or combo of both. Hard to determine precise contribution, but nAb suggest *some* immune evasion (less than B.1.351?).
github.com/CADDE-CENTRE/N…


github.com/CADDE-CENTRE/N…


Immune evasion & re-infections is key part of story told by @nmrfaria @carlzimmer. Paper suggests seroprevalence was ~100% at time P.1 invaded. If this estimate was accurate (possibly not:
nytimes.com/2021/03/01/hea…

https://twitter.com/WesPegden/status/1336801382955933697), need huge immune evasion for spread.
nytimes.com/2021/03/01/hea…
That seems like a possible explanation, except new paper argues that mutations in all variants (P.1, B.1.351, B.1.1.7) have "negligible" impact on T-cells & T-cells play key role in disease severity.
biorxiv.org/content/10.110…


biorxiv.org/content/10.110…

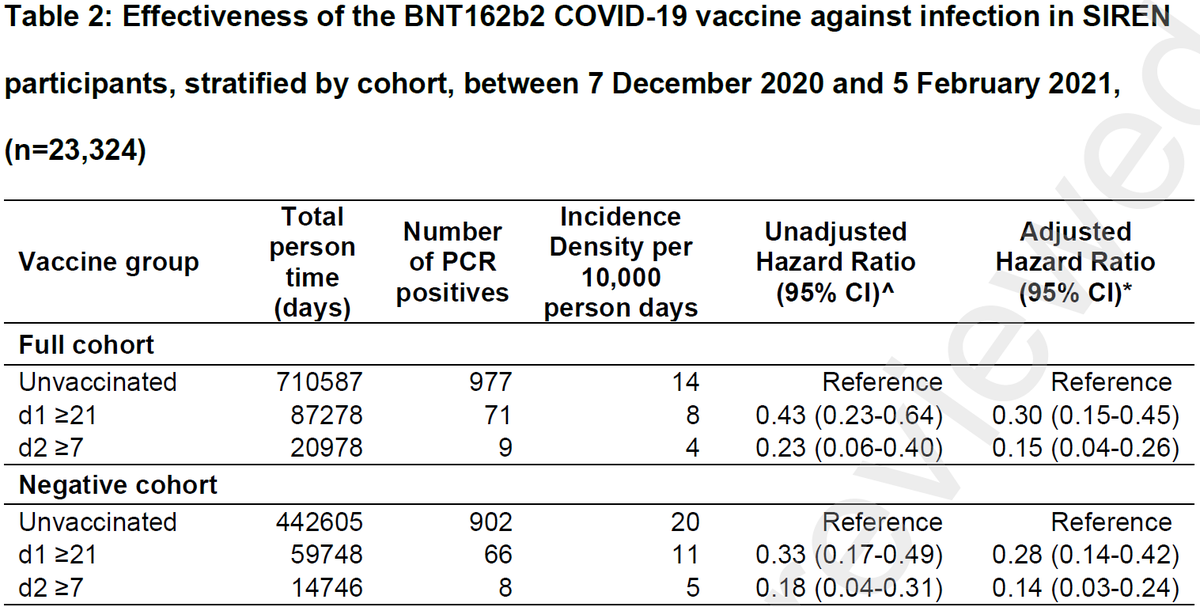
More generally, I see a disconnect b/w
-interpretation of immunity studies indicating that moderate reduction in neutralizing antibodies (from vaccines or prev infection) will have little effect on actual protection from infection/disease &
-epi studies claiming immune evasion.
-interpretation of immunity studies indicating that moderate reduction in neutralizing antibodies (from vaccines or prev infection) will have little effect on actual protection from infection/disease &
-epi studies claiming immune evasion.
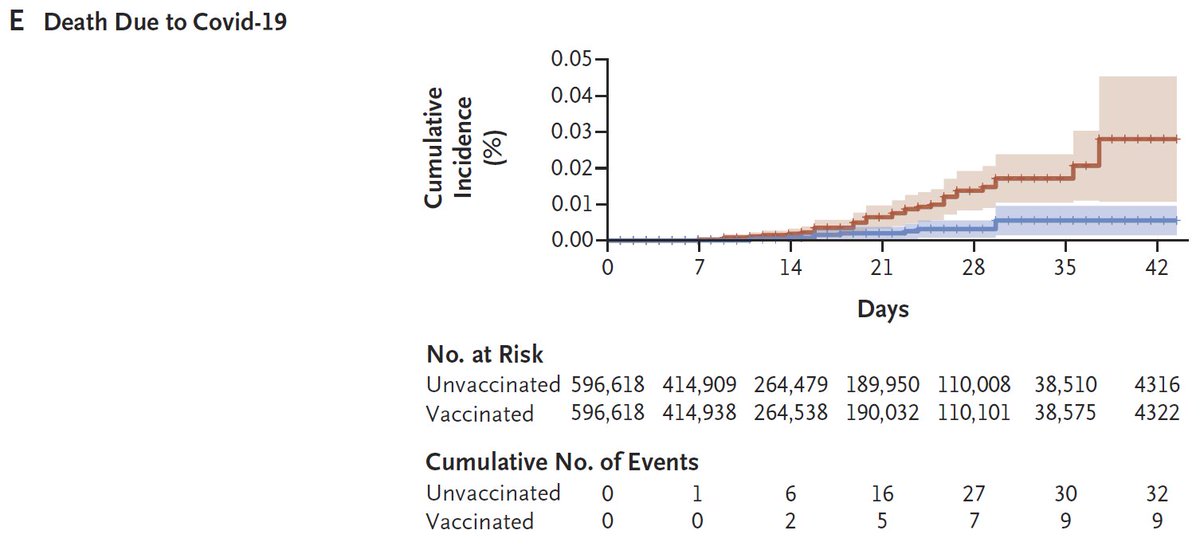
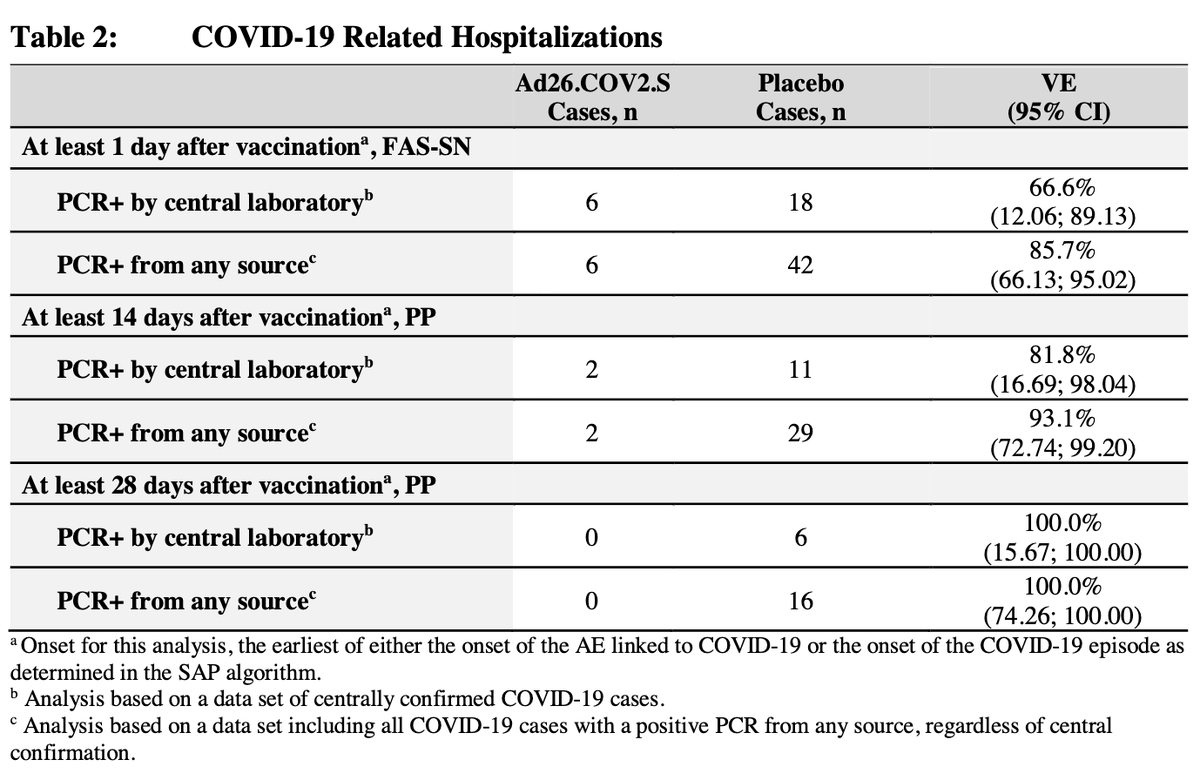
One could argue that disconnect is b/c virus variants evade immune system to cause infection but not disease. But that's not consistent with Brazil paper. Hospitalizations & deaths are as high or higher than 1st wave. Why didn't supposedly robust T-cells prevent severe disease? 
I *AM NOT* an immunologist. I've tried to follow/learn from people like @florian_krammer @profshanecrotty @VirusesImmunity @SetteLab but I have not seen an explanation that reconciles these data.
I'm confused by conflicting claims (need full thread)
-nAb are just 1 part of immune response & ~4-6 fold reduction isn't that important for disease
-nAb responses can be used by FDA to assess/change vaccine dosing (1 dose vs 2; 1/2 dose vs full) & to update vaccines for variants
-nAb are just 1 part of immune response & ~4-6 fold reduction isn't that important for disease
-nAb responses can be used by FDA to assess/change vaccine dosing (1 dose vs 2; 1/2 dose vs full) & to update vaccines for variants
To me, the data above suggest 2 possibilities:
H1)Acquired immunity in Brazil was much lower than paper suggests & higher 2nd wave was due to mostly NEW infections w/ more transmissible variant & relaxed restrictions (or both). T-cells & nAb (mostly) protected those prev exposed.
H1)Acquired immunity in Brazil was much lower than paper suggests & higher 2nd wave was due to mostly NEW infections w/ more transmissible variant & relaxed restrictions (or both). T-cells & nAb (mostly) protected those prev exposed.
Note that re-infection is actually not uncommon. 3 studies suggest protection from prev exposure is only 82%:
medrxiv.org/content/10.110…
83%:
medrxiv.org/content/10.110…
89%
nejm.org/doi/full/10.10…
So a moderate # of reinfections (often milder) is expected at this point.
medrxiv.org/content/10.110…
83%:
medrxiv.org/content/10.110…
89%
nejm.org/doi/full/10.10…
So a moderate # of reinfections (often milder) is expected at this point.
Could possibly test hypothesis H1 w/ reliable serological study. Need:
-Ab assay that doesn't show fast sero-reversion, like many nucleocapsid tests seem to @isabelrodbar
-unbiased serosurvey
-Ab assay that doesn't show fast sero-reversion, like many nucleocapsid tests seem to @isabelrodbar
-unbiased serosurvey
https://twitter.com/DiseaseEcology/status/1285696432478052355
H2)Immunity from previous infection or vaccination is NOT protective, even against severe disease & death, if re-infected with certain variants (P.1 & possibly B.1.351), possibly after some time (>6 mo?). If H2 is true, we'd need vaccine boosters ASAP.
I'm not sure if testing H2 would be possible by comparing those in Manaus, Brazil that were & weren't infected in 1st wave in 2nd wave. Tricky to remove biases in comparison (
https://twitter.com/DiseaseEcology/status/1365072677770174466), but alternative is poor: wait & see what happens as P.1 spreads elsewhere.
I'd love comments from immunologists, @nmrfaria & others on how to reconcile these data. I think similar Qs arise about B.1.351 in S Africa.
I think it matters b/c it determines the importance of vaccine boosters for variants. If H1 true, not huge priority. If H2, urgently needed
I think it matters b/c it determines the importance of vaccine boosters for variants. If H1 true, not huge priority. If H2, urgently needed
Some epi folks that might have ideas (immunologists tagged above)
@AdamJKucharski @rozeggo @_nickdavies @JoannaMasel @jLewnard @sarahcobey @SRileyIDD @KoelleLab @mlipsitch @sbfnk @LucaFerrettiEvo @ChristoPhraser
@AdamJKucharski @rozeggo @_nickdavies @JoannaMasel @jLewnard @sarahcobey @SRileyIDD @KoelleLab @mlipsitch @sbfnk @LucaFerrettiEvo @ChristoPhraser
Adding a randomized serological study from Brazil that suggested a much lower seroprevalence towards end of 1st wave (<26%).
thelancet.com/journals/langl…
thelancet.com/journals/langl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh