
1/ A trainee approached me re: a "hypothetical" case. A patient p/w acute weakness 90 min after onset of R arm/leg without other neuro deficits. The neurology consultant advised IV tPA after CT/CTA head and neck showed no hemorrhage (and also no LVO). The ED attending balked.
2/ Trainee's ?: Can you have a stroke with only motor involvement? Can you have a stroke that causes weakness of the arm and leg, but not the face?... a short tweetorial
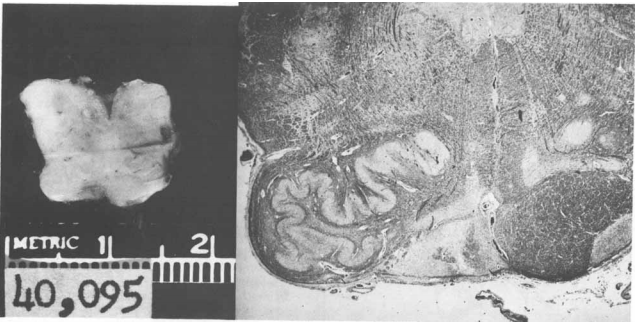
3/ C. Miller Fisher described several lacunar stroke syndromes, including pure motor hemiparesis (PMH). He found the most common anatomical locations responsible for PMH (based on autopsy studies) to be the internal capsule and basis pontis. jamanetwork.com/journals/jaman… 



4/ Strokes in those locations typically involved the face/arm/leg. So can a cerebral infarction involve only the arm and leg and spare the face? Allan Ropper (with CMF) described a case of PMH due to medullary pyramid infarction sparing the face. pubmed.ncbi.nlm.nih.gov/570681/ 


6/ These same authors demonstrated that PMH can also be caused by cortical infarcts. jamanetwork.com/journals/jaman… 

7/ Melo et al. found PMH represented 14% of consecutively admitted stroke pts. The weakness distributions were as follows: face, upper limb, and lower limb (50%); face and upper limb (29%); upper limb (10%); and upper and lower limb (9%). n.neurology.org/content/42/4/7…
8/ In part, through these clinicopathological correlation studies, we were able to map out the corticospinal tract. As Miller Fisher said, we learn neuro-anatomy "stroke by stroke" 

9/ Notice that the corticobulbar tract diverges from the corticospinal tract in the pons. So lesions below this take-off are likely to spare the face! Also, notice how the UMNs splay at the cortex, making it possible for small cortical lesions to (uncommonly) spare the face.
10/ So... yes PMH is an ischemic stroke syndrome, usually caused by deep infarcts of the internal capsule or pons. Face-sparing PMH usually localizes to the medullary pyramids.
11/ Hypothetical case f/up: Pt did not receive IV tPA and dedicated neck imaging revealed spontaneous cervical spine epidural hematoma!! Unclear why not seen on CTA of neck. Medicine is hard. End.
#MedEd #FOAMed #NeuroTwitter #StrokeTwitter @AaronLBerkowitz @caseyalbin @ZachThrelkeldMD @Tracey1milligan @umarylandneuro @MDNeurocritcare @ChaturvediNeuro @msphippsmd @EM_RESUS @MedTweetorials @drdangayach @StrokeAHA_ASA @AANMember @MGHNeurology @harvardneuromds
• • •
Missing some Tweet in this thread? You can try to
force a refresh





