1/ This week the #MedEdTwagTeam is bringing you a final #TweetorialTuesday summarizing the #feedback threads from @GStetsonMD & @JenniferSpicer4 over last 10 weeks. 

2/ If you missed any of our threads, you can go to the @MedEdTwagTeam handle and follow so you don’t miss out!
Check out our pinned tweet, which has "Moments" for each of our #tweetorial series.
Check out our pinned tweet, which has "Moments" for each of our #tweetorial series.

3/ Week 1 provided an overview, and Week 2 emphasized the importance of relationships & culture as the foundation of effective feedback.
@GStetsonMD emphasized these 2 articles:
1⃣The Educational Alliance: pubmed.ncbi.nlm.nih.gov/25406607/
2⃣Feedback as Coaching: pubmed.ncbi.nlm.nih.gov/30907439/
@GStetsonMD emphasized these 2 articles:
1⃣The Educational Alliance: pubmed.ncbi.nlm.nih.gov/25406607/
2⃣Feedback as Coaching: pubmed.ncbi.nlm.nih.gov/30907439/

4/ We also emphasized the importance of both modeling & promoting a growth mindset rather than a fixed mindset.
Here's a short article in @MedEd_Journal describing applications of Carol Dweck's growth mindset theory in #MedEd
…ary-wiley-com.proxy.library.emory.edu/doi/10.1111/me…
Here's a short article in @MedEd_Journal describing applications of Carol Dweck's growth mindset theory in #MedEd
…ary-wiley-com.proxy.library.emory.edu/doi/10.1111/me…

5/ In Week 3, we discussed some common components of effective feedback.
My discussion of appropriate "timing" seemed to resonate with learners and reminded us that sometimes learners are not in an emotional space for feedback (e.g., after a code or after an overnight call).
My discussion of appropriate "timing" seemed to resonate with learners and reminded us that sometimes learners are not in an emotional space for feedback (e.g., after a code or after an overnight call).

6/ In Week 4, @GStetsonMD described methods for feedback and provided us with the ART model:
A: Ask learners for their impression.
R: Reflect on what they said by paraphrasing it
T: Tell them your feedback focusing on their impressions.
See his thread for specific examples!
A: Ask learners for their impression.
R: Reflect on what they said by paraphrasing it
T: Tell them your feedback focusing on their impressions.
See his thread for specific examples!

7/ In Week 5 & 6 we discussed formative & summative feedback.
During week's 5 formative feedback thread, we emphasized the coaching model. Trust is the key and allows daily feedback.
Daily feedback may sound like a lot - but remember, it's short, quick, & specific.
During week's 5 formative feedback thread, we emphasized the coaching model. Trust is the key and allows daily feedback.
Daily feedback may sound like a lot - but remember, it's short, quick, & specific.

8/ Then, in Week 6, I discussed summative feedback, focused on the dreaded end-of-rotation feedback discussion.
But remember, it you have a learner-centered conversation anchored in your learner's previously identified goals, this can be a really impactful conversation!
But remember, it you have a learner-centered conversation anchored in your learner's previously identified goals, this can be a really impactful conversation!

9/ In Week 7, I discussed written feedback.
Be aware of our tendency to use "coded language" pubmed.ncbi.nlm.nih.gov/25693989/
Evaluate the narrative for bias/stereotypes. Resources:
*⃣handout @ucsfmed: meded.ucsf.edu/sites/meded.uc…
*⃣website to check for gender bias: slowe.github.io/genderbias/
Be aware of our tendency to use "coded language" pubmed.ncbi.nlm.nih.gov/25693989/
Evaluate the narrative for bias/stereotypes. Resources:
*⃣handout @ucsfmed: meded.ucsf.edu/sites/meded.uc…
*⃣website to check for gender bias: slowe.github.io/genderbias/

10/ In Week 8, @GStetsonMD emphasized avoiding the term "struggling learner" when we have learners who aren't meeting expectations.
There are MANY reasons this may happen. It's our job to identify the BEHAVIOR, discuss it openly (& bidirectionally) with our learners, & HELP them
There are MANY reasons this may happen. It's our job to identify the BEHAVIOR, discuss it openly (& bidirectionally) with our learners, & HELP them

11/ Here is an example he provided of how to have a conversation after identifying the behavior, cause, & frequency.
This is the "Tell" portion of an ART feedback conversation:
*⃣Name the behavior
*⃣Explain the impact
*⃣Ask the learner's reflections
*⃣Co-create goals
This is the "Tell" portion of an ART feedback conversation:
*⃣Name the behavior
*⃣Explain the impact
*⃣Ask the learner's reflections
*⃣Co-create goals

12/ In Week 9, I tackled the difficult problem of soliciting feedback, especially when hierarchy exists.
To get better feedback, consider asking peers & learners.
When soliciting feedback from learners, first ask for feedback on SPECIFIC areas, then GENERAL thoughts.
To get better feedback, consider asking peers & learners.
When soliciting feedback from learners, first ask for feedback on SPECIFIC areas, then GENERAL thoughts.

13/ In Week 10, @GStetsonMD closed with a discussion of how to receive feedback gracefully by highlighting 5 key strategies for cultivating this extremely important skill. 

14/ This figure from Week 10 emphasizes how hearing feedback can help us identify blindspots.
Our intentions are not always represented by our actions or their impact.
Remembering this can help us take feedback gracefully and consider how to realign our intentions & actions.
Our intentions are not always represented by our actions or their impact.
Remembering this can help us take feedback gracefully and consider how to realign our intentions & actions.

15/ Thank you for joining the @MedEdTwagTeam on this feedback journey.
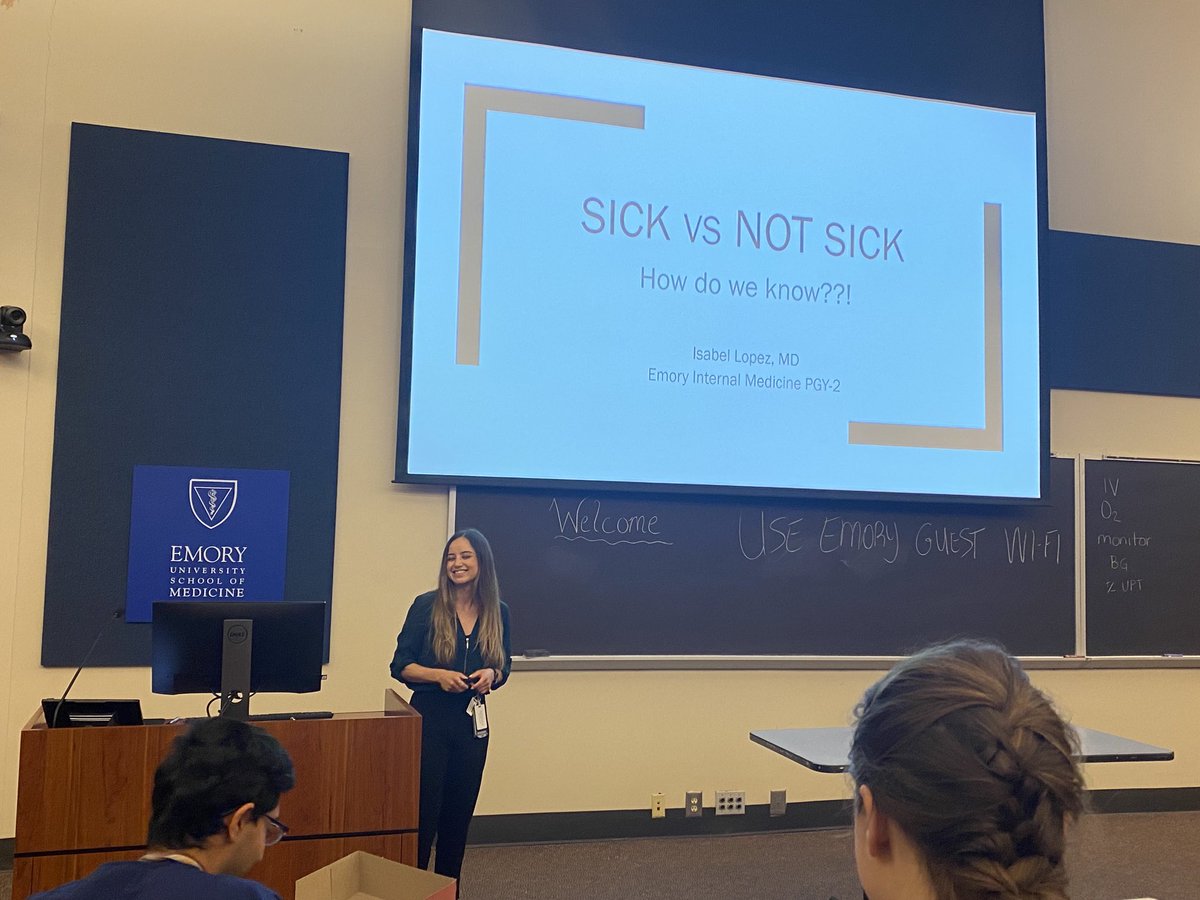
Next week, @GStetsonMD will start sharing threads on asking fair questions, then we will delve into a series on clinical teaching tips!
Let us know if there are specific topics that you want us to cover!
Next week, @GStetsonMD will start sharing threads on asking fair questions, then we will delve into a series on clinical teaching tips!
Let us know if there are specific topics that you want us to cover!

@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh