A Tale of Two Pandemics
The pandemic won’t be over until most of the world is vaccinated, but access is a HUGE challenge.
Globally, we must scale up manufacturing and vaccinate the 50M health workers & 1B people over 60. In the US, we must proactively reach the unreached. 1/
The pandemic won’t be over until most of the world is vaccinated, but access is a HUGE challenge.
Globally, we must scale up manufacturing and vaccinate the 50M health workers & 1B people over 60. In the US, we must proactively reach the unreached. 1/
Vaccine inequity is a serious problem, both ethically and epidemiologically. It increases the risk that dangerous variants will emerge. Wealthy countries have excess vaccines while lower and middle-income countries go without. 2/ 

The reality is that global vaccine supply will lag the need for at least a year. Open IP is a step, but we need much more—transfer of vaccine technology and hubs for production. We can also be more strategic in use of the vaccine that is available. 3/
Right now, it’s crucial that we direct vaccines to where they’re needed most. Globally, that means prioritizing—and tracking data on—vaccination access and coverage among health care workers and people 60 and over. 4/
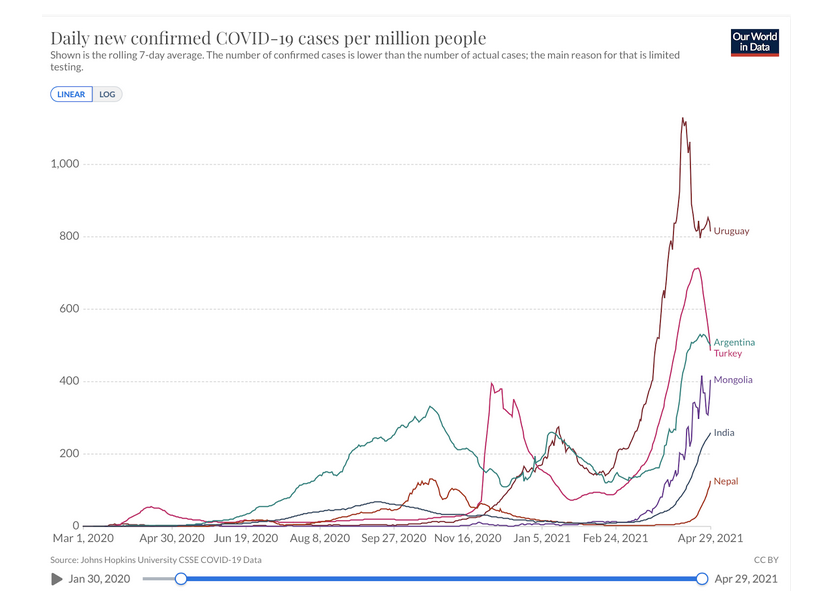
Globally wherever Covid is spreading, we must mask and distance, as these are the only measures that will make a short-term difference and are essential for the medium term. Vaccination won’t crush the curve for months in places with explosive spread now. 5/
There are an estimated 50M health care workers globally, including approximately 1.7M in Africa. Health worker deaths from Covid are preventable, yet more than 17,000 have died. To vaccinate each health care worker would require less than one week of vaccine production. 6/
Vaccinating health workers not only protects them, it also protects continued health care. This is particularly crucial in Africa, which faces millions of deaths from measles, TB, malaria & other diseases unless this is done. We should support countries that focus on this. 7/
It’s estimated that >80% of global Covid deaths are among people age 60+. There are ~1B people 60+ and <1/3 in countries with insufficient vaccine and significant risk of Covid, including 74 million in Africa. We should also support countries to get this group vaccinated ASAP. 8/
In the US, we’ve made a lot of progress on vaccination. By summer, we’ll see cases, hospitalizations and deaths come way down, as predicted. But we still have work to reach the unreached. The “build it and they will come” phase of vaccination is over.
https://twitter.com/DrTomFrieden/status/1351201887794683916?s=209/
Most (60%) adults in the US have already been at least partially vaccinated and more people are choosing to get vaccinated every day. But there’s a misperception that most unvaccinated people aren’t willing to get vaccinated. 10/
Many saw this @KFF survey as a negative sign. I saw it differently—only a small portion of people are strongly opposed to vaccination and many more people haven’t yet been vaccinated because of lack of access, NOT reluctance. bit.ly/3erZd8C 11/
Convenient access to vaccines is still the biggest challenge for the US vaccination program. According to another new @KFF survey, unvaccinated Hispanic adults are twice as likely as white adults to want a Covid vaccine ASAP. bit.ly/3eJcvxy 12/
In a @MorningConsult survey, 77% of white adults who want a shot have gotten one, but that number is only 60% for Black adults and 55% for Hispanic adults. bit.ly/2R1i2qc 13/
We must be proactive, which means reaching people where they are. We should be calling and sending reminders to patients. Vaccination must be widely available in doctors' offices, churches, schools, corner stores, supermarkets, bars, pop-ups at community events & more places. 14/
The Yankees, Mets and other teams are offering vaccination at ballgames. Great! atmlb.com/3hbbpfy 15/
Reluctance is also an issue, but convenience tends to overcome reluctance. More and more people understand that vaccination is a way TOWARD more freedom, rather than away from it. Holdouts will become fewer as vaccination becomes the norm. 16/
There’s light at the end of the tunnel, but we can’t be blinded by it. Transferring mRNA technology & stepping up production globally are essential and the most important step we can take to help end the pandemic. Not sharing this technology puts all of us at continued risk. 17/
Vaccination will save lives and prevent explosive spread everywhere—once it’s available. But in most places globally, the way to save lives right now is to mask, distance, and improve ventilation. Here’s what we need to do to in the months ahead to scale up vaccination. 18/
In the short term, we need to quickly expand supplies of materials and services to the global supply chain, save the most lives by using existing supply to vaccinate health workers and older people, and mask and distance to flatten the curve now where spread is uncontrolled. 19/
In the medium term, we need technology transfer to manufacturing hubs regionally so that effective vaccines, particularly mRNA vaccines, can be rapidly scaled up, especially for low- and middle-income countries. 20/
In the long term, we need to position mRNA as a platform to address Covid variants and other emerging threats and balance appropriate respect for IP with the public good of pandemic prevention, and increase the number of vaccine producers. 21/
We also need to strengthen readiness.
https://twitter.com/DrTomFrieden/status/139289675819214848022/
The pandemic is far from over. But if we work together effectively across borders, we can end this emergency and become more resilient against future health threats. We truly are all connected. We need to act that way. An outbreak anywhere is a threat everywhere. 23/end
• • •
Missing some Tweet in this thread? You can try to
force a refresh