
New data suggests GP Online Triage/Consultations do NOT lead to increased patient demand: THREAD @MinalBakhai @HelenRSalisbury @mgtmccartney @keithgrimes @MartinRCGP @murrayellender @fhussain73 @bcdelaney1 @ClareGerada @prof_tweet @jacobnhaddad @dave_dlt @sib313 @DrLindaDykes
Three Norfolk @NHSNWCCG practices have used Total Online Triage since 2019. All patient requests for clinical help are entered into the online system, either by patient or receptionist. 

Total online triage is good for analysis of demand, since all demand is captured. No patient is told 'no appointments left, try again tomorrow'.
Many of the lessons will apply to practices using online consultations in other ways.
Many of the lessons will apply to practices using online consultations in other ways.
It’s often assumed that rapid online access to GP will increase demand, as patients realise how easy it is to get help.
Under this hypothesis, it would take months to see the full increase in demand, since patients would only gradually learn about the new easy-access system:
Under this hypothesis, it would take months to see the full increase in demand, since patients would only gradually learn about the new easy-access system:

Demand was completely flat from week 1, or even fell. This strongly suggests that all these patients were going to make contact anyway, regardless of the new system (there was minimal advance publicity of the change*).
* NARRATOR: This was a bad idea, but that's another story.
* NARRATOR: This was a bad idea, but that's another story.

I found this hard to believe too. After all, there are several sources of additional demand now:
🏥Secondary care delays
😢Mental health effects of pandemic
💉Clinical queries relating to vaccines
🏥Secondary care delays
😢Mental health effects of pandemic
💉Clinical queries relating to vaccines
AND YET, demand is down. So there must be even stronger countervailing factors which are keeping demand down.
Most importantly: patients are not selfish rational economic actors who will abuse any service that is easy to access and free at the point of use.
This is a common fallacy, and not what economists believe.
This is a common fallacy, and not what economists believe.
Humans are social beings, and we long to be part of a tribe/society in which people care for us and we care for them. Few institutions evoke these feelings as strongly as the NHS. People care about the NHS and have a strong impulse not to 'waste our time'.
⬆️This, I believe, is the strongest factor that keeps demand in check. Especially now.
There are also factors that act to reduce demand in an online triage system, compared to a traditional appointment system: 

Note that some of these factors only apply to practices which use online consultations to offer an efficient and rapid service to patients. Some practices deliberately make their online access slow and convoluted, out of a belief that this keeps demand down.
They may experience the worst of both worlds: they will still be exposed to the entirety of patient demand, without the efficiency of online triage or the reductions in demand that come from patients' confidence in good access.
I repeat: demand in these Online Triage practices is DOWN compared to pre-pandemic levels. Anyone following GP social media will recognise that this evidence goes completely against the dominant assumptions.
Can General Practice cope with this level of demand? Quick comparison: our pre-pandemic baseline demand was below the oft-cited figure of 72 GP appointments per 1000 patients per week. This is not a like-for-like comparison, so don't read too much into it. 
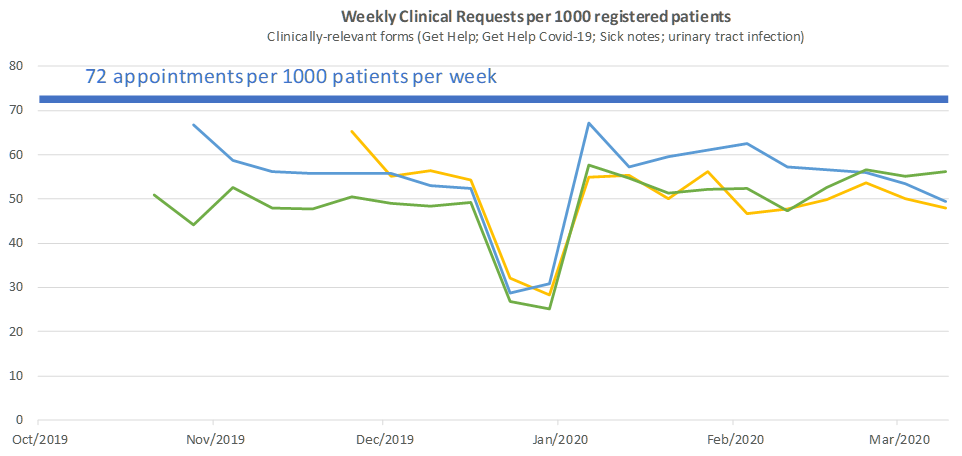
If this level of demand were repeated across England and was managed only by GPs, this would mean 16 clinical contacts per GP session. Some practices with efficient processes already manage this level of workload well.
Add in non-GP clinicians, and the 5000 GPs that are, ahem, on the way - and this reduces to a very manageable 12 contacts per session. 

I'm not saying that General Practice is adequately resourced. I'm aware this analysis misses much of the hidden workload that creeps in through letters, tasks and other routes.
But there are some important conclusions from this data:
But there are some important conclusions from this data:
1. Online Consultations/Triage do not lead to escalating demand. We don't have to go back to making patients queue on the phone for an hour, and lose the efficiencies that can come from digital transformation, in order to stop workload going up.
This way of working is in its early days. I have little doubt that approaches based on online triage could bring massive efficiencies - of the order of 50% - while improving the quality and continuity of care.
https://twitter.com/EdTurnham/status/1377738866422075395?s=20
2. The current difficulties in General Practice are NOT patients' fault.
Some practices are trying to 'educate' their patients, based on the unfounded assumption that demand is going up and up. The evidence shows that patients are contacting us LESS than usual.



Some practices are trying to 'educate' their patients, based on the unfounded assumption that demand is going up and up. The evidence shows that patients are contacting us LESS than usual.



My clinical experience fits with the evidence. Many patients are being TOO heroic, struggling alone with severe/worrying symptoms. The statements I quote above are likely to make this worse, while doing little to stop the small proportion of demand that is inappropriate.
By making an incorrect diagnosis of the problem, we prevent ourselves from finding real solutions. Let's stop going down the dead end of trying to suppress demand.
Let's instead embrace technology that enables efficient, high quality care for all patients that need it.
Let's instead embrace technology that enables efficient, high quality care for all patients that need it.
Addendum: I should have mentioned that all three practices made a 'big bang' launch, i.e. they went in less than 1 week from offering no online consultations to full Online Triage.
• • •
Missing some Tweet in this thread? You can try to
force a refresh





