
I just talked at #ERAEDTA21 about proton pump inhibitors and nephrotoxicity
It was an epidemiological take
If anyone is interested here’s my talk condensed in a n/14🧵
It was an epidemiological take
If anyone is interested here’s my talk condensed in a n/14🧵
Fact: PPIs cause interstitial nephritis. It’s something we commonly see in nephrology and made up 11% of renal biopsies in the Scottish biopsy registry in 2017, just behind IgA nephropathy, the commonest diagnosis
srr.scot.nhs.uk/Biopsy-Registr…
srr.scot.nhs.uk/Biopsy-Registr…
But how common is it in the population? This nice nested c-c study from New Zealand suggested an incidence of 12 people per 100,000 treated in a year....so pretty uncommon
pubmed.ncbi.nlm.nih.gov/24646856/
pubmed.ncbi.nlm.nih.gov/24646856/
But PPIs are very commonly prescribed: this data from @openprescribing by @EBMDataLab (fun!! Go and play) suggests more nearly 1 in 10 people in England are prescribed a PPI 

So if there are a substantial number of cases of undiagnosed TIN is this contributing to the population burden of CKD? Large studies using routine data have enabled us to look at the association between PPIs and CKD (and AKI) outcomes: 

However, there is a substantial issue with residual confounding across these studies: patients taking PPIs have more health problems than those who don’t, as summarised memorably by @Nephro_Sparks, and this effect can be hard to remove 

We summarised the potential sources of confounding in relation to this difficult research question here: pubmed.ncbi.nlm.nih.gov/28201528/
And there is a long history of observational associations with PPIs.
This excellent paper uses different epidemiological approaches to address confounding in relation to a potential interaction between clopidogrel and PPIs
(COI it’s by my bestie)
bmj.com/content/345/bm…
This excellent paper uses different epidemiological approaches to address confounding in relation to a potential interaction between clopidogrel and PPIs
(COI it’s by my bestie)
bmj.com/content/345/bm…
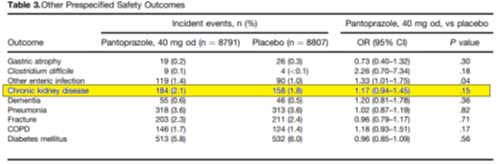
Data from the COMPASS trial among 17,598 pts with stable CVD/PAD randomly assigned to pantoprazole or placebo followed up for a median of 3 years showed no difference for development for CKD
pubmed.ncbi.nlm.nih.gov/31152740/
pubmed.ncbi.nlm.nih.gov/31152740/
Despite the lack of a clear causal link there are many calls to deprescribe PPIs where they are not clearly indicated with a range of tools, risk scores and algorithms to help decide this
(e.g. deprescribing.org/wp-content/upl… )
(e.g. deprescribing.org/wp-content/upl… )

The risks of getting it wrong are substantial: the Oxford Vascular study found that absolute risk of major UGI bleed among people ≥75 yrs was 9·2 (95% CI 6·7-12·2) per 1000 patient-years and 62% were disabling or fatal
thelancet.com/journals/lance…
thelancet.com/journals/lance…
Decision making is made harder by the withdrawal of ranitidine due to contamination with potentially carcinogenic nitrosamines 

PPIs cause int nephritis but absolute rates are low
Obs studies show association w kidney outcomes but confounding problematic & no evidence of major kidney harm from RCTs
We should minimise use of PPIs but there can be associated harms
Withdrawal of ranitidine is a problem
Obs studies show association w kidney outcomes but confounding problematic & no evidence of major kidney harm from RCTs
We should minimise use of PPIs but there can be associated harms
Withdrawal of ranitidine is a problem
Also thanks the other speakers @perezgomezmv and Sergey Brodsky and to co-chair Dr Catalina Martin Cleary (is she on here? I can't find her) for describing me as fierce which has made my year
• • •
Missing some Tweet in this thread? You can try to
force a refresh





