
**Tachyarrhythmia case**
- Middle-aged patient admitted with septic shock on norepinephrine. Home meds include metoprolol 100 qday.
- Baseline rhythm: sinus at HR ~100.
- STAT call to bedside for HR in 170s-180s with escalating norepi requirements.
- The monitor screenshot:
1/
- Middle-aged patient admitted with septic shock on norepinephrine. Home meds include metoprolol 100 qday.
- Baseline rhythm: sinus at HR ~100.
- STAT call to bedside for HR in 170s-180s with escalating norepi requirements.
- The monitor screenshot:
1/

2/
-Initial read: narrow-complex tachycardia.
-First therapy: Adenosine
-Result: rhythm not converted but adenosine confirms underlying P-waves with atrial rate of ~180
-Interpretation: SVT at rate of ~180 with 1:1 conduction
-Differentials considered: sinus tach vs atrial tach.
-Initial read: narrow-complex tachycardia.
-First therapy: Adenosine
-Result: rhythm not converted but adenosine confirms underlying P-waves with atrial rate of ~180
-Interpretation: SVT at rate of ~180 with 1:1 conduction
-Differentials considered: sinus tach vs atrial tach.
3/
- Further history: RN confirms that "HR has been ~100 all day". Such high rate makes sinus tachycardia less likely.
- Next step: amio 150 bolus: worsened hypotension but rhythm persists.
- Due to hemodynamic instability, decision made to cardiovert --> was unsuccessful x2!!
- Further history: RN confirms that "HR has been ~100 all day". Such high rate makes sinus tachycardia less likely.
- Next step: amio 150 bolus: worsened hypotension but rhythm persists.
- Due to hemodynamic instability, decision made to cardiovert --> was unsuccessful x2!!
4/
Next step: Quick review of trends on telemetry. Looks like the HR gradually escalated from ~100 over a few minutes! (images)
This is quite unusual for a tachyarrhythmia to do that. So is this indeed sinus tachycardia?
But the HR is 180!?!
~~~
Let's pause and analyze:
Next step: Quick review of trends on telemetry. Looks like the HR gradually escalated from ~100 over a few minutes! (images)
This is quite unusual for a tachyarrhythmia to do that. So is this indeed sinus tachycardia?
But the HR is 180!?!
~~~
Let's pause and analyze:

5/
Technically, this is a long RP NCT. Other than sinus tach & atrial tach, the differential includes:
(iii)Atypical (slow-slow) AVNRT: However, a re-entrant arrhythmia should have been terminated by adenosine/cardioversion, so less likely. (More on this:litfl.com/avnrt-for-two/)
Technically, this is a long RP NCT. Other than sinus tach & atrial tach, the differential includes:
(iii)Atypical (slow-slow) AVNRT: However, a re-entrant arrhythmia should have been terminated by adenosine/cardioversion, so less likely. (More on this:litfl.com/avnrt-for-two/)

6/
(iv)PJRT: a rare form of AVRT. Since this is a reentrant arrhythmia as well, it should have been terminated with adenosine/cardioversion
Hence, we are indeed left with 2 options: sinus tach vs atrial tach
-An important feature to make this distinction is the P-wave morphology
(iv)PJRT: a rare form of AVRT. Since this is a reentrant arrhythmia as well, it should have been terminated with adenosine/cardioversion
Hence, we are indeed left with 2 options: sinus tach vs atrial tach
-An important feature to make this distinction is the P-wave morphology
7/
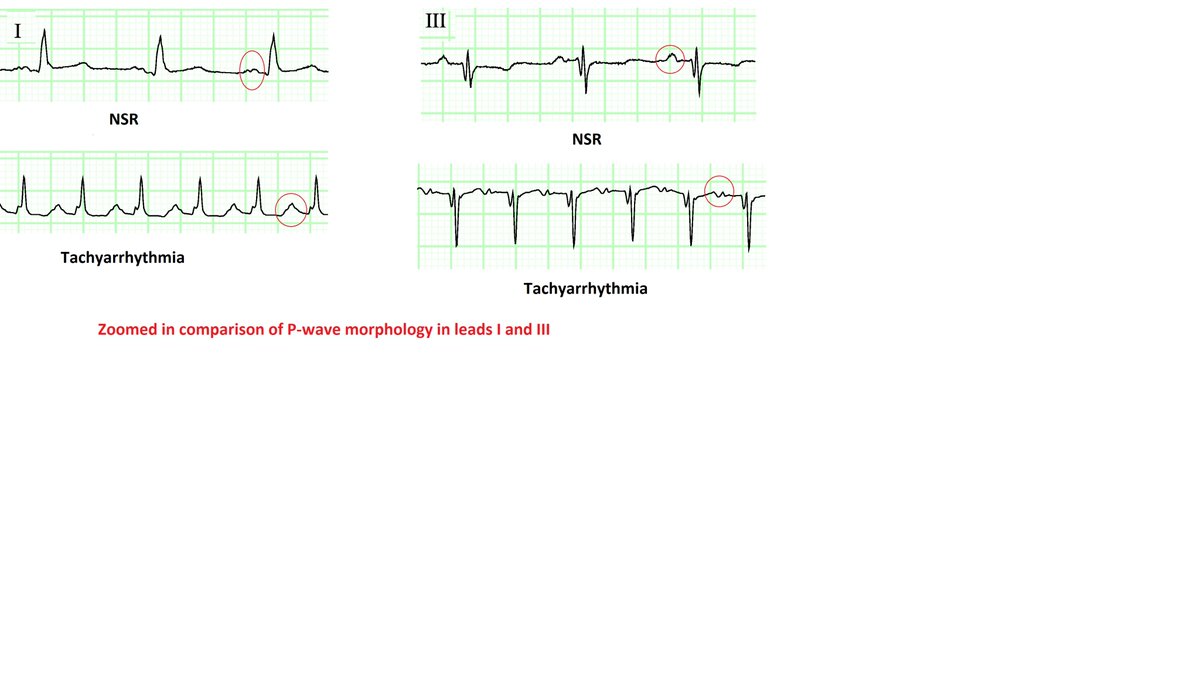
Let's review the telemetry in further detail:
The most likely point of tachycardia origin is identified in the attached image. Note the subtle difference in P-wave morphology in lead I.
However, this difference could not be picked up in any other monitor leads.

Let's review the telemetry in further detail:
The most likely point of tachycardia origin is identified in the attached image. Note the subtle difference in P-wave morphology in lead I.
However, this difference could not be picked up in any other monitor leads.


8/
The telemetry ECGs typically have aggressive filters and hence may miss subtle changes in morphology.
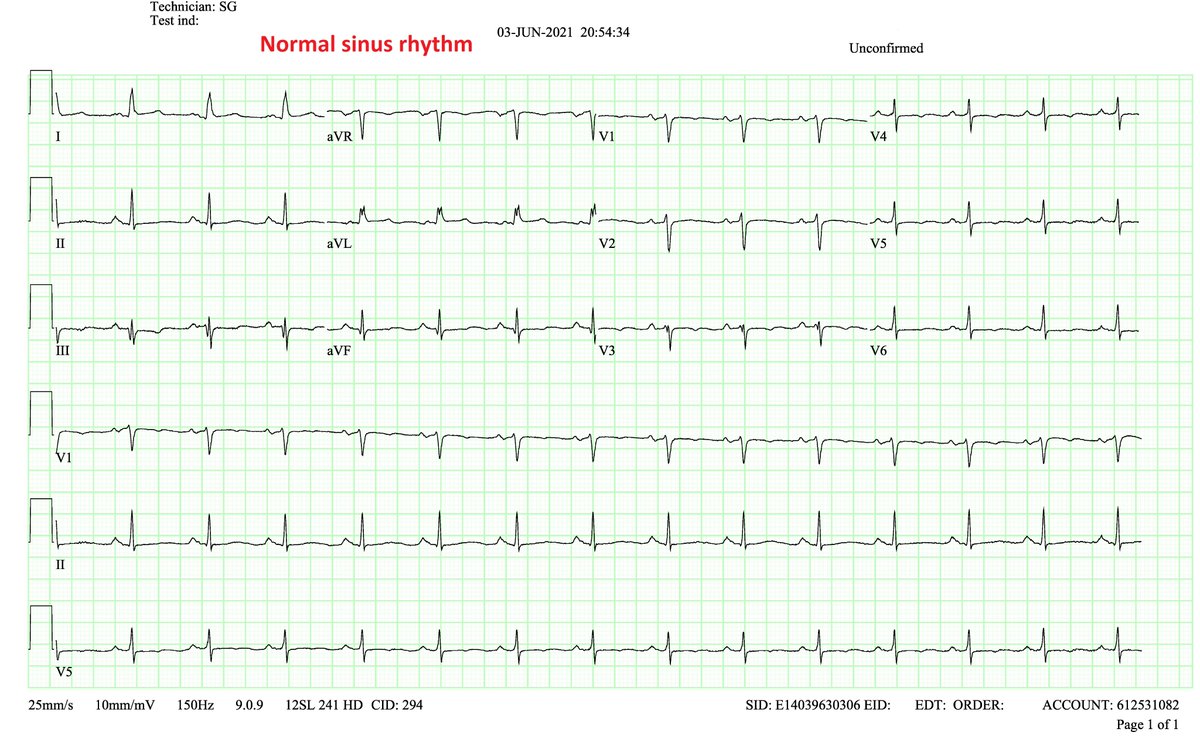
A 12-lead ECG will have higher precision. In the image, subtle changes in P-wave morphology can be appreciated in both lead I and III
The all other leads look about the same


The telemetry ECGs typically have aggressive filters and hence may miss subtle changes in morphology.
A 12-lead ECG will have higher precision. In the image, subtle changes in P-wave morphology can be appreciated in both lead I and III
The all other leads look about the same

9/
This is highly suggestive of ectopic (non-sinus) focus of atrial excitation. Since the difference in P-wave morphology is difficult to identify & the P-axis is about the same, the location of the ectopic focus is likely close to the SA node.
Provisional diagnosis: Atrial tach
This is highly suggestive of ectopic (non-sinus) focus of atrial excitation. Since the difference in P-wave morphology is difficult to identify & the P-axis is about the same, the location of the ectopic focus is likely close to the SA node.
Provisional diagnosis: Atrial tach
10/
(Focal) atrial tachycardias (ATs) can be further classified as:
(a)Automatic ATs: due to enhanced automaticity
(b)Non-automatic ATs: due to microreentry or triggered activity
Automatic ATs have some unique characteristics:
(i)They don't terminate with adenosine/cardioversion
(Focal) atrial tachycardias (ATs) can be further classified as:
(a)Automatic ATs: due to enhanced automaticity
(b)Non-automatic ATs: due to microreentry or triggered activity
Automatic ATs have some unique characteristics:
(i)They don't terminate with adenosine/cardioversion
11/
... ,while non-automatic ATs do
(ii) Automatic ATs often accelerate over several seconds (warm-up): this was seen in our case {image}. Also, they gradually slow down on termination (cool-down).
Hence, the mainstay of treatment in automatic AT is sympathetolysis.
... ,while non-automatic ATs do
(ii) Automatic ATs often accelerate over several seconds (warm-up): this was seen in our case {image}. Also, they gradually slow down on termination (cool-down).
Hence, the mainstay of treatment in automatic AT is sympathetolysis.

12/
Back to the case...
Norepi was switched to phenylephrine. As this was happening, the tachyarrhythmia converted back to sinus rhythm while exhibiting a "cool-down" behavior (HR reduced over several seconds).
/End
(This is my interpretation but I may be missing something)
Back to the case...
Norepi was switched to phenylephrine. As this was happening, the tachyarrhythmia converted back to sinus rhythm while exhibiting a "cool-down" behavior (HR reduced over several seconds).
/End
(This is my interpretation but I may be missing something)

CCing #EPeeps and EKG gurus for their thoughts:
@narrowQRS @smithECGBlog @amalmattu @ecgrhythms @KTamirisaMD @epfellow @apoor_gami @hhuang123 @MoeenSaleem @rhythmkeys @netta_doc @krishmd @SergioPinski @adribaran @ECGfan @rdschaller
Also, cc: @siddharth_dugar @Katelyn14398447
@narrowQRS @smithECGBlog @amalmattu @ecgrhythms @KTamirisaMD @epfellow @apoor_gami @hhuang123 @MoeenSaleem @rhythmkeys @netta_doc @krishmd @SergioPinski @adribaran @ECGfan @rdschaller
Also, cc: @siddharth_dugar @Katelyn14398447
• • •
Missing some Tweet in this thread? You can try to
force a refresh









