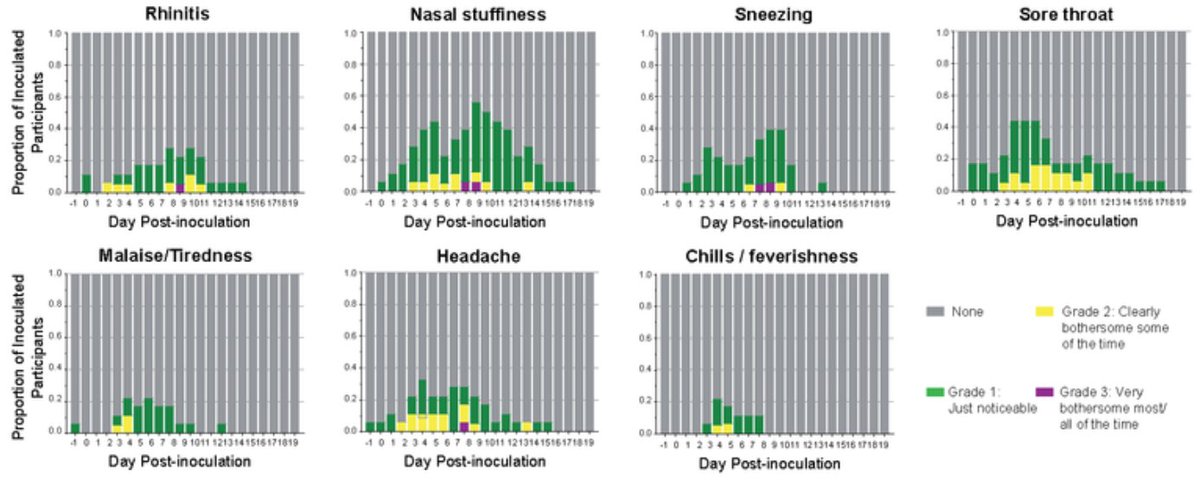
My first tweetorial! On our new #InnateImmunity and viral interference study @JExpMed. It started with puzzling observations that pointed to the importance of kinetics. We saw a robust interferon response in the upper airway in all COVID patients studied, mild and severe: 

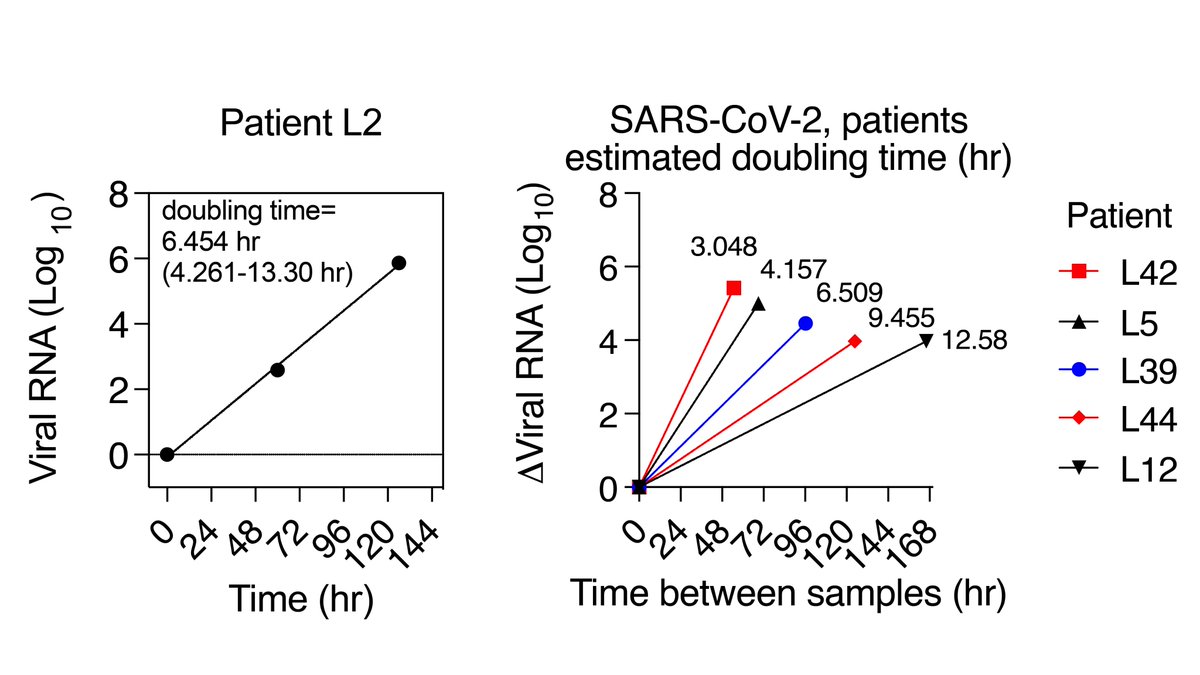
..But these samples were from different times in the disease course. To get at timing, we studied serial swabs from patients picked up early in infection, when the viral load was still going up. We measured virus and CXCL10, a biomarker of the interferon response… 

…both went up, then down, almost perfectly in synch… except for lag in the antiviral response in the first few days of infection. Replication in the first few days was exponential and fast! (avg. doubling time 6 hr).... 
….but it was all over when the interferon response kicked in. So we asked- what happens if we alter the kinetics of the IFN response with the common cold? We infected with rhinovirus prior to COVID (in organoids, not patients!), and this completely blocked COVID replication: 
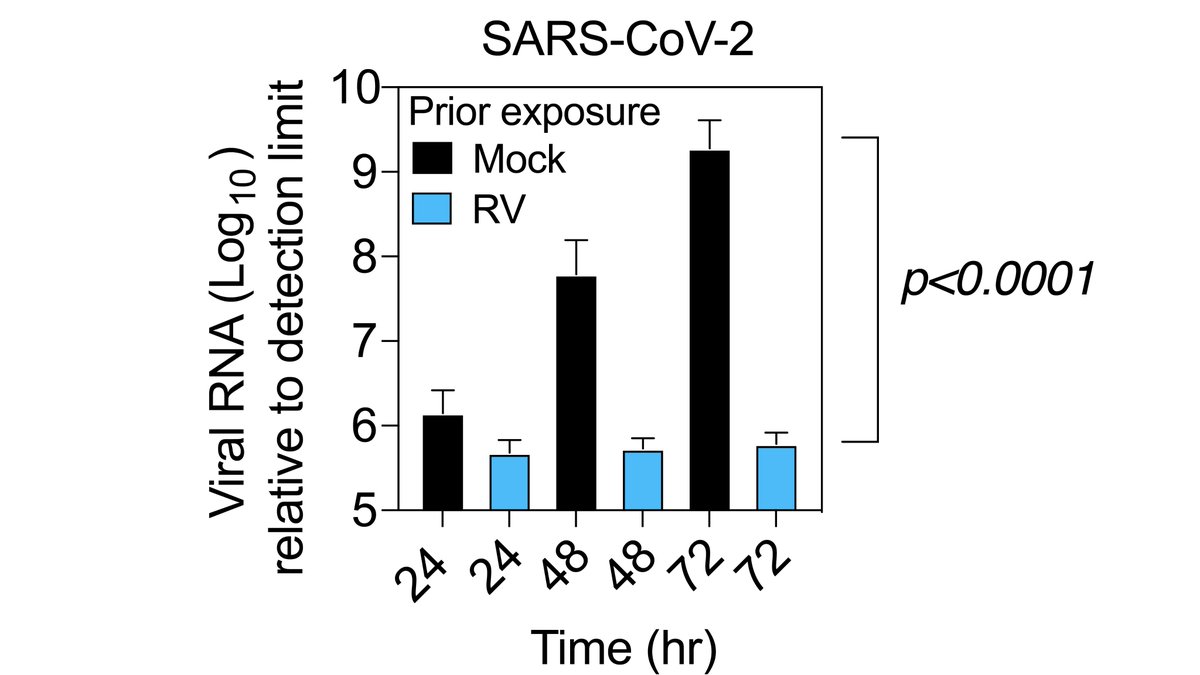
..by jump-starting the interferon response, which started much earlier in epithelial cells which had seen rhinovirus a few days before. Rhinovirus induced ISGs, even in uninfected cells, for at least 5 days (all cells ISG high, but <2% of cells RV-positive at day 5)... 

Interference from RV required the interferon response, but during infection with COVID only (high infectious dose), the interferon response had no impact on early viral replication. At a lower infectious dose, however, interferon response did slow COVID down significantly... 

This also prompted us to speculate, based on work by @mugecevik and others, that one mechanism for increased transmissibility of variants could be better blockade of IFN responses (outruns IFN response> higher NP viral load). This seems to be the case in preprint from @KroganLab
..which describes IFN antagonism by the UK variant (alpha), as @carlzimmer explains in @NYtimes nytimes.com/2021/06/07/hea…
..Our study also raises a question about the extent to which heterologous innate immunity happens "in real life".. could periods of high common cold virus circulation this potentially mitigate against spread of other viruses? 

But picture may be more complex- timing and host innate immune status matter. With intact innate immunity, both RV and COVID decreased during co-infection, but if we blocked these responses, both viruses increased. See full paper for details --rupress.org/jem/article/21…
Thank you, #COVID19 scientists and #scicomm pros for your great work and communication during this pandemic, which informed/inspired this study.🙏🙏🙏
• • •
Missing some Tweet in this thread? You can try to
force a refresh