Happening now! I'll try to live tweet as I'm able.
Note: there are a few times where Q&As are welcome from the public! Questions can be pasted in the chat and will be answered during specific time slots. See the agenda for those times.
#LongCOVID
1/
Note: there are a few times where Q&As are welcome from the public! Questions can be pasted in the chat and will be answered during specific time slots. See the agenda for those times.
#LongCOVID
1/
https://twitter.com/ahandvanish/status/1414971350071001097
First up Dr. Stanley Perlman on neurologic complications of coronaviruses generally (not just this one).
This study (from 20 years ago!!) shows that there is a discrepancy when the body tries to get rid of the virus, it causes inflammation/damage.
2/
This study (from 20 years ago!!) shows that there is a discrepancy when the body tries to get rid of the virus, it causes inflammation/damage.
2/

-A specific coronavirus is theorized to be the initiator of multiple sclerosis (this is still at the theory stage)
3/
3/

Comparing to MERS:
-MERS has much higher morbidity (35%)
-don't know much about the brain because only 2 autopsies have been performed
4/
-MERS has much higher morbidity (35%)
-don't know much about the brain because only 2 autopsies have been performed
4/
Curiously he said neuro symptoms were not as common in SARS-1.
This is likely not direct virus invasion except maybe in nasal cavity?
CNS damage likely from poorly understood effects of inflammatory mediators (endothelial dysfunction).
Sequelae can last for over a year...
5/
This is likely not direct virus invasion except maybe in nasal cavity?
CNS damage likely from poorly understood effects of inflammatory mediators (endothelial dysfunction).
Sequelae can last for over a year...
5/

Next up is Tom Solomon, talking about hospitalized patients.
-1/3 of patients develop neurologic symptoms after initial phase
-respiratory & systemic symptoms often develop first
-but some patients have neuro features as first symptoms
-encephalopathy most common (49%)
6/
-1/3 of patients develop neurologic symptoms after initial phase
-respiratory & systemic symptoms often develop first
-but some patients have neuro features as first symptoms
-encephalopathy most common (49%)
6/

Three mechanisms:
-inflammatory response
-pro-thrombotic state (including microvascular clots)
-virus invasion of endothelial cells?
7/
-inflammatory response
-pro-thrombotic state (including microvascular clots)
-virus invasion of endothelial cells?
7/
Jennifer Frontera up next, again on only hospitalized patients. "COVID seems to predispose patients to neurovascular events."
1.6% of COVID patients vs 0.2% of flu patients have strokes.
8/
1.6% of COVID patients vs 0.2% of flu patients have strokes.
8/

There are so many mechanisms that may underlie stroke (I notice antiphospholipid antibodies on this chart!)
9/
9/

I missed the context but she just mentioned a collagen marker in relation to the blood-brain barrier breakdown? curious if anyone knows more about this
11/
11/
Talking about cognitive consequences, including Alzheimer's - what happens with COVID patients will be important to follow.
Some neurodegenerative markers are *higher* than patients with Alzheimer's. Unknown if this is temp or ongoing
12/
Some neurodegenerative markers are *higher* than patients with Alzheimer's. Unknown if this is temp or ongoing
12/

Dr. Elizabeth Whittaker up on COVID's neurologic effects on kids. Curiously she makes the note that most of them test negative on PCR!
13/
13/

Exhaustion, altered awareness and confusion are some of the most common symptoms in kids :(
At six months, the most common symptoms were neurological (same as our study!)
14/
At six months, the most common symptoms were neurological (same as our study!)
14/

-Are early biomarkers of inflammation and neuronal damage in children associated with long term neurocognitive effects? #LongCovid
-Long COVID happens in about 8% of kids.
15/
-Long COVID happens in about 8% of kids.
15/
Clarification on tweet 11/:
A blood brain barrier study found fibrinogen in the parenchemya (shouldn't be there, must be coming out of blood vessels). Blood vessels with "disrupted collagen vascular basal lamina suggesting breakdown of the blood brain barrier."
cc @jenbrea 16/
A blood brain barrier study found fibrinogen in the parenchemya (shouldn't be there, must be coming out of blood vessels). Blood vessels with "disrupted collagen vascular basal lamina suggesting breakdown of the blood brain barrier."
cc @jenbrea 16/
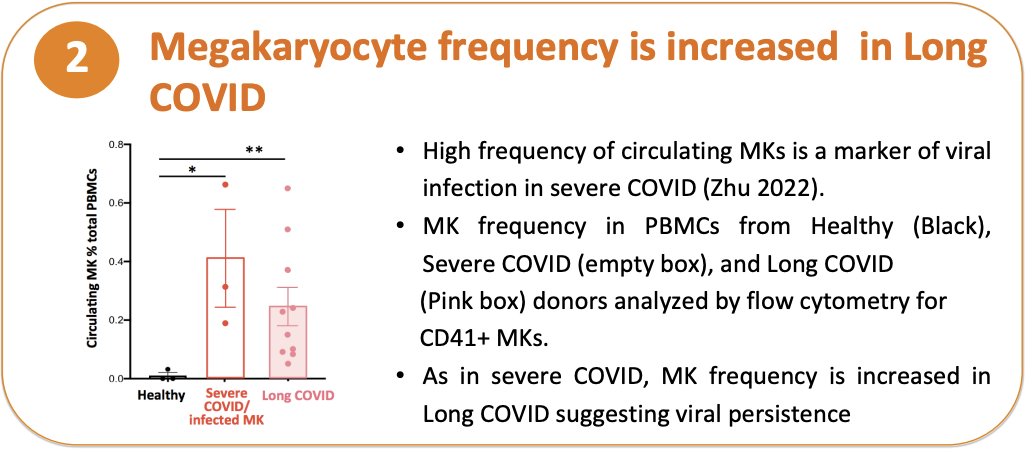
Many of these talks are only hospitalized patients. Next is Dr. Shelli Farhadian on antibodies in CSF. Despite infecting brains of mice, they can't find antibodies in CSF.
COVID patients have more CSF B cells than controls, possibly autoimmunity targeting neuro tissue? 17/
COVID patients have more CSF B cells than controls, possibly autoimmunity targeting neuro tissue? 17/
On neuroimaging: Dr Dima Hammoud is talking about the recent biobank study, which showed a loss of brain volume in both hospitalized but also nonhospitalized COVID patients
18/
18/

Hypometabolism (PET) is also a common finding, in nonhospitalized patients as well - one study found some improvement between month 1 and 6 but still cognitive deficits compared to controls 19/ 

(For people who are interested in imaging, check out the work of Dr. Jarred Younger and Dr. Michael VanElzakker (@MBVanElzakker)!
20/
20/
Dr. Markus Glatzel on neuropathological findings.
Neuroinflammation is most common, but virus is also found in the brain in some cases.
"The blood brain barrier crossing is probably the most important route the virus takes into the brain."
22/
Neuroinflammation is most common, but virus is also found in the brain in some cases.
"The blood brain barrier crossing is probably the most important route the virus takes into the brain."
22/

When the virus is found, it's found near blood vessels/endothelial cells, and also has been found in brain parenchyma (echoing Dr. Frontera above)
23/
23/

Collagen coming up again! In relation to "string vessels" which are thin connective tissue strands with no endothelial cells/blood flow.
Found in Alzheimer's, found in high levels in COVID patients
cc @jenbrea
24/

Found in Alzheimer's, found in high levels in COVID patients
cc @jenbrea
24/


@jenbrea (BTW questions are open for submission in the live stream!! ask your questions!!) 25/
@jenbrea Dr. Rebecca Folkerth is talking about sudden death even in patients who have recovered, and her hypothesis that there are actually neuro/vascular reasons for this
26/
26/
Break is over - Dr. Alex Sigal is up next on the effects of coinfection with other viruses (i.e. HIV) with COVID.
Interestingly this is different by variant! The first wave had no difference between HIV+ and HIV- patients, but the second wave (a different variant) did!
28/
Interestingly this is different by variant! The first wave had no difference between HIV+ and HIV- patients, but the second wave (a different variant) did!
28/

I'm out of spoons so going to take a break during the next few, which are mostly on autopsy findings and delirium
31/
31/
Hopped on to the final panel discussion.
Q from Avi Nath: the fear is that there may be a large population of accelerated dementia/Alzheimer's. Loss of smell is also a sign in these. What's the relationship between these diseases and COVID?
32/
Q from Avi Nath: the fear is that there may be a large population of accelerated dementia/Alzheimer's. Loss of smell is also a sign in these. What's the relationship between these diseases and COVID?
32/
Answer from Dr. Masliah: Microglial activation plays a role, we've seen this in COVID, still hard to tell but I do think there will be an overlap
33/
33/
Day 2 has started! Quickly summing up the first two:
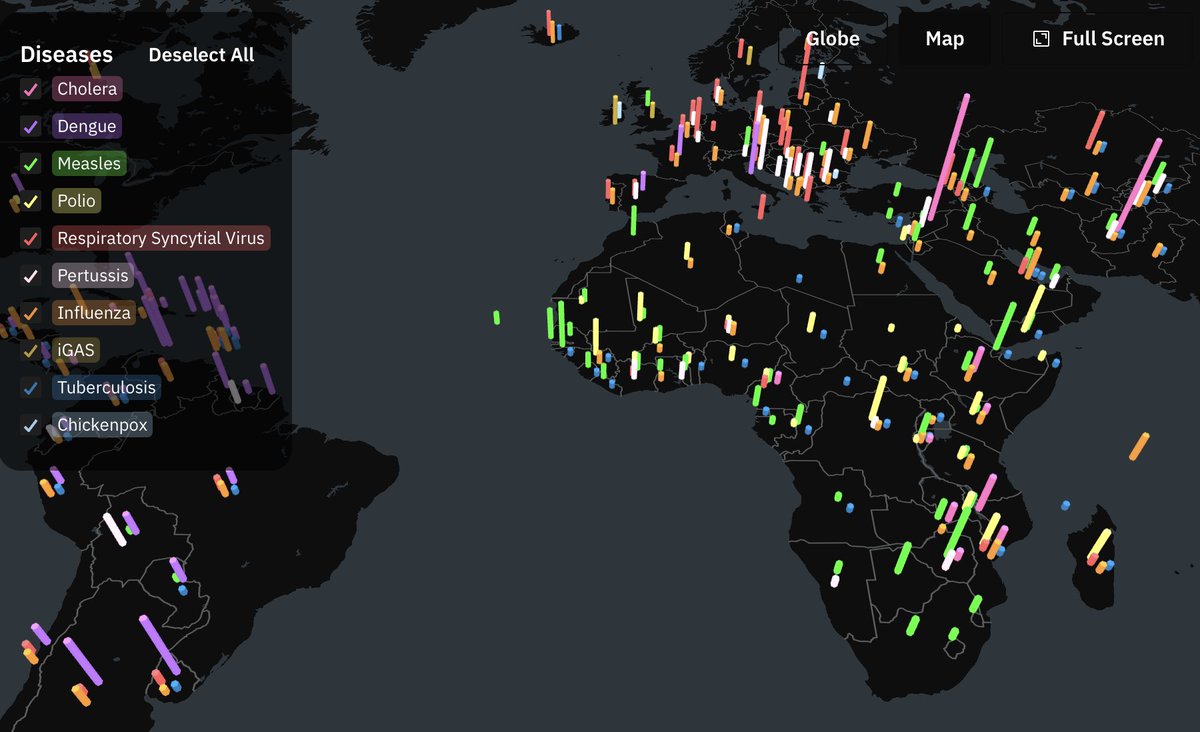
Dr. Avi Nath talked about other illnesses with long term sequelae - some, like polio, happen years (even up to 40 years!!!) after onset. Dengue is another one that can happen over years (15-16 years in one case).
34/
Dr. Avi Nath talked about other illnesses with long term sequelae - some, like polio, happen years (even up to 40 years!!!) after onset. Dengue is another one that can happen over years (15-16 years in one case).
34/
@patientled Dr. Koralnik also talked about mostly non-hospitalized long haulers. These are the trajectories of pos vs neg patients. Negative COVID patients were more likely to miss more work, validating @Dr2NisreenAlwan et al's study!
36/
36/

@patientled She is diving into the pathophysiologies of #LongCOVID and is highlighting neuroinflammation:
38/
38/

@patientled She mentions that basic bloodwork panels are often normal, but has seen low CD4 in some patients, others with inflammatory markers, some elevated IgG in the CSF
39/
39/
@patientled Q&A: do different variants have different levels of neurotropism?
A: we haven't started to study this, but this does happen in HIV variants - global studies should take this into account.
41/
A: we haven't started to study this, but this does happen in HIV variants - global studies should take this into account.
41/
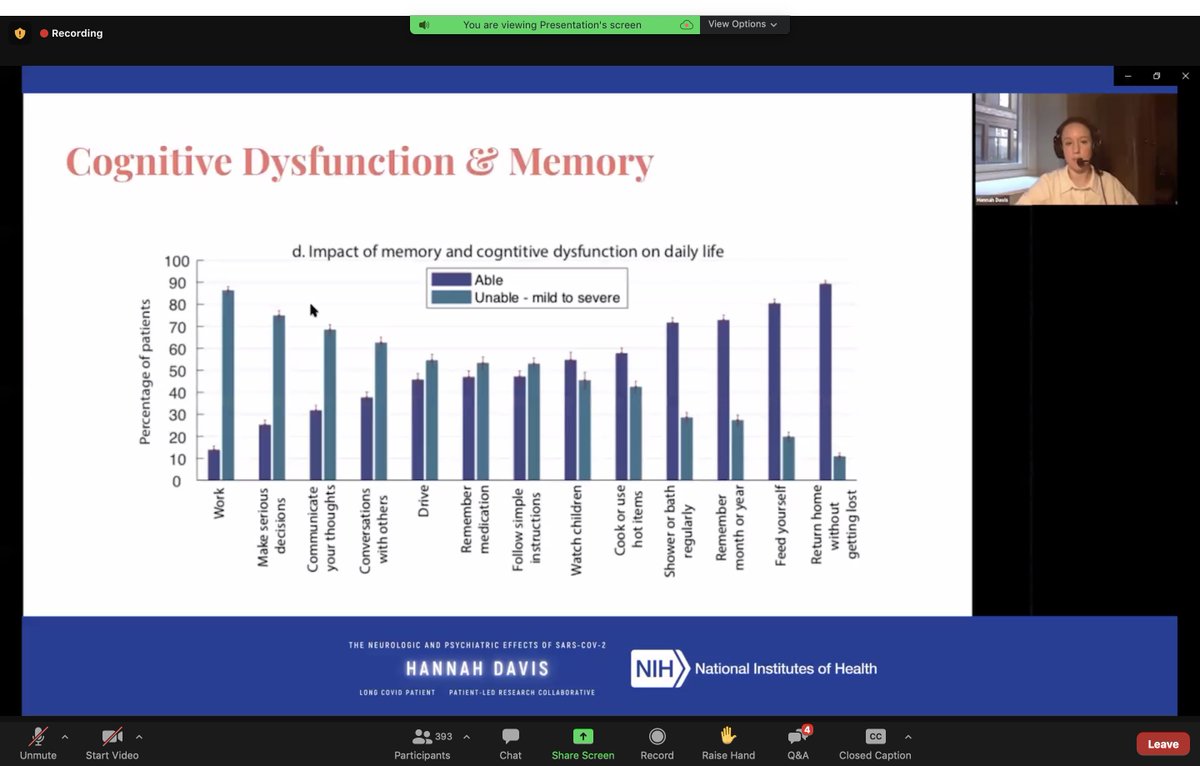
@patientled @AthenaAkrami Neuropsychiatric symptoms are more likely not to change over time or to slightly increase over time #LongCOVID
44/
44/

@patientled @AthenaAkrami (We will post this talk afterwards since it is chock-full of information) 45/
@patientled @AthenaAkrami She brings up the important point that so many of these symptoms that may not seems neurologic at first actually likely have neurologic underpinnings:
46/
46/

Next up @chiluvs1!!
She is giving a powerful narrative history on how she used to be, "a salute to what my brain could do."😭
"My brain was amazing, functional, analytical, until March 2020. My brain became a burden." #LongCOVID
48/
She is giving a powerful narrative history on how she used to be, "a salute to what my brain could do."😭
"My brain was amazing, functional, analytical, until March 2020. My brain became a burden." #LongCOVID
48/
@chiluvs1 "Watching myself lose my superpowers month by month was a traumatic experience and still is. It makes talking to you today extremely difficult."
49/
49/
@chiluvs1 I cannot communicate how amazing this talk is. Please watch it when available. It captures the enormous, all-encompassing effect of not only losing her brain, but how her loss impacted the community's ecosystem & was deprioritized by the med community by being a Black woman. 50/
Next up @PamBelluck who has been reporting on the neuropsychiatric effects of COVID and #LongCOVID all year! She is currently talking about the abrupt onset psychosis of a young patient which lasted for months
51/
51/
Dr. Mejia up next talking about how Black & Hispanic patients disproportionately die from COVID, & that is just the tip of the iceberg (we *still* have no data on how Long COVID impacts these populations!)
She mentions gaps in access to neurology care, up to 20% difference
52/
She mentions gaps in access to neurology care, up to 20% difference
52/

She talks about how everyone, and especially clinicians, need to be learning about anti-racism to close these gaps in medical care:
54/
54/

Dr. Dravid is talking about a cohort in Pune of mostly hospitalized patients. I think this point is really interesting - that despite loss of smell (anosmia) and taste being talked about a lot, it is really not a symptom that shows up in the majority of patients
55/
55/

Didn't live tweet the panel but it can be seen when the recording is out!
On brain organoids for COVID - Dr. Mankowski mentions that it seems like glial cells rather than neurons may be infected?
56/
On brain organoids for COVID - Dr. Mankowski mentions that it seems like glial cells rather than neurons may be infected?
56/

Last speaker was on a predictive model to predict COVID positivity which TBH I am pretty unexcited about & don't think these models should be used at this time because we just don't have enough societal awareness of the biases especially from the early waves. 57/
Next up: Dr. Masliah mentions that of all patients with dementia, those with vascular dementia are at greater risk:
58/
58/

Dr. Dua mentions @LongCovidSOS's call for recognition, research, and rehabilitation for #LongCOVID!
59/
59/

• • •
Missing some Tweet in this thread? You can try to
force a refresh