1/ Alright, time to give this #EmoryNCCTweetorials a swirl!
The setup: Neuro ICU at @EmoryNeuroCrit
The pt: Basilar stroke s/p tPA & MT. Now intubated & undergoing stroke workup
You’re called to the bedside for sats in the 80s!
@MedTweetorials #MedEd #tweetorial #neurotwitter
The setup: Neuro ICU at @EmoryNeuroCrit
The pt: Basilar stroke s/p tPA & MT. Now intubated & undergoing stroke workup
You’re called to the bedside for sats in the 80s!
@MedTweetorials #MedEd #tweetorial #neurotwitter
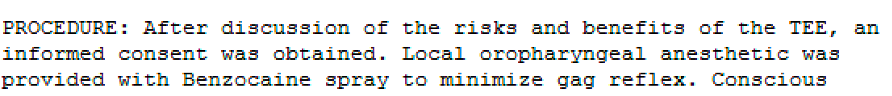
2/ RN lets you know that the patient just completed their TEE....
O2 is beeping, 88% ➡️87%➡️ 86%
O2 is beeping, 88% ➡️87%➡️ 86%
3/ Time to quickly go over your checklist
✅Auscultate breath sounds?
Normal.
✅Change sensor on O2 sat probe?
Still 86%.
✅Check ETT placement?
Unchanged from the day prior.
✅Compliance/Plugging issue?
Normal Peak and Plateau pressure. Nothing clogged.
✅Auscultate breath sounds?
Normal.
✅Change sensor on O2 sat probe?
Still 86%.
✅Check ETT placement?
Unchanged from the day prior.
✅Compliance/Plugging issue?
Normal Peak and Plateau pressure. Nothing clogged.
4/ Fine…time to jack up the FiO2 to 100%
.
.
.
Still satting at 86%. 🤔 Is this a PTX?
U/S shows the following
.
.
.
Still satting at 86%. 🤔 Is this a PTX?
U/S shows the following
5/Patient looking more and more uncomfortable. He's becoming less interactive. What’s going on?!
6/ Time to 📞 a friend (& attending extraordinaire @CajalButterfly ), who calmly assesses the situation.
“Send a blood gas”
“Send a blood gas”
8/ Yes! It’s methemoglobinemia!
A brief review,
In normal Hgb, Iron is in the ferrous state (Fe2+), which allows binding and release of oxygen. In methemoglobin, the altered Hgb has its Iron oxidized in its ferric state (Fe3+), which does not bind to oxygen at all!
A brief review,
In normal Hgb, Iron is in the ferrous state (Fe2+), which allows binding and release of oxygen. In methemoglobin, the altered Hgb has its Iron oxidized in its ferric state (Fe3+), which does not bind to oxygen at all!
9/ This causes normal heme to have an increased affinity to oxygen ➡️less oxygen gets to the tissues ➡️ produces a left shift on the oxygen-hemoglobin dissociation curve
10/ Symptoms range from being asymptomatic to having cyanosis, dyspnea, headache, seizures, fatigue, shock, and respiratory failure.
It can be hereditary or acquired.
From the acquired group, the MCC are medication including dapsone, chloroquine, inhaled nitric oxide….
It can be hereditary or acquired.
From the acquired group, the MCC are medication including dapsone, chloroquine, inhaled nitric oxide….
11/ And a topical inhalants commonly used to do things like anesthetize a patient’s pharynx for TEE
.
.
.
Benzocaine spray.
Sure enough, a look back through our patient’s chart confirms our suspicion!
.
.
.
Benzocaine spray.
Sure enough, a look back through our patient’s chart confirms our suspicion!
12/ Treatment includes discontinuing the offending agent and increasing oxygen to help oxygen delivery.
For mild cases, you can use Vitamin C IV 1-10g (although it can take a while to work).
For mild cases, you can use Vitamin C IV 1-10g (although it can take a while to work).
13/ For moderate/severe cases where methemoglobin is >20%, or in patients with significant symptoms, you can use methylene blue IV at 1-2mg/kg aka Smuff’s Blood (though caution in patients with G6PD deficiency).
14/ So why does the pulse ox sensor show an oxygen saturation at 85% even if PaO2 is high? It’s the way the pulse ox uses the ratio of light being absorbed at two different wavelengths to calculate the results.
15/ Oxygenated🩸absorbs more light at the 940nm, whereas deoxygenated🩸absorbs light more at 660nm.
Methemoglobin absorbs light equally at 940nm and 660nm thereby “confusing” the pulse ox into thinking oxygen saturation is ~85% when it may actually be much lower
Methemoglobin absorbs light equally at 940nm and 660nm thereby “confusing” the pulse ox into thinking oxygen saturation is ~85% when it may actually be much lower
16/ Here’s a great paper going over everything ncbi.nlm.nih.gov/books/NBK53731…
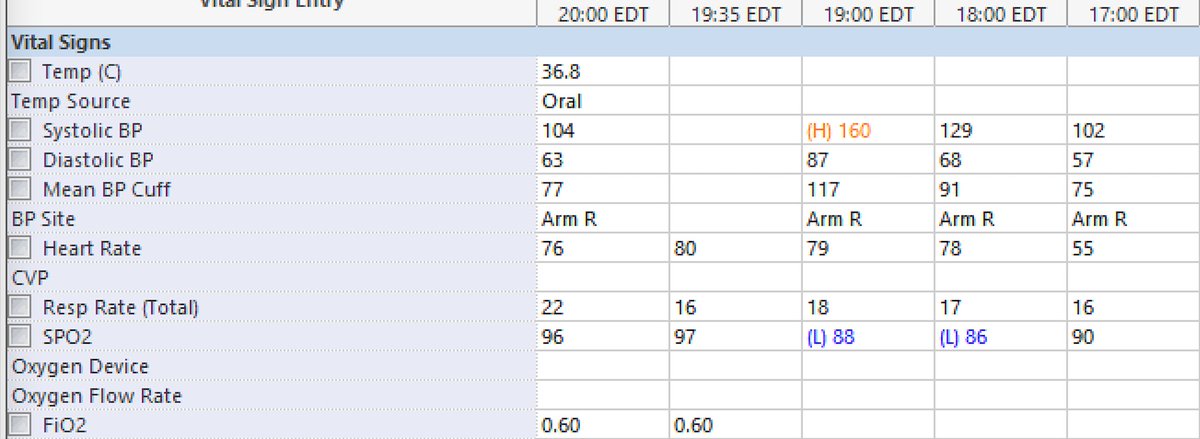
Back to our case.
Reading from right to left, you can see the SpO2 go from 90% at 1700 ➡️ 86% at 1800 [given methylene blue about 30-45 minutes later] ➡️ 88% at 1900 ➡️ 97% at 1935…all cured!
Back to our case.
Reading from right to left, you can see the SpO2 go from 90% at 1700 ➡️ 86% at 1800 [given methylene blue about 30-45 minutes later] ➡️ 88% at 1900 ➡️ 97% at 1935…all cured!
17/ Now you know that the next time you get pulled into a desatting patient’s room, your first question should always be, “did this person just have a TEE?” #justkidding #nobutreally
@sigman_md @mallyaa @EricLawson90 @maness_caroline
And a special thanks @caseyalbin!
@sigman_md @mallyaa @EricLawson90 @maness_caroline
And a special thanks @caseyalbin!
• • •
Missing some Tweet in this thread? You can try to
force a refresh