
#IssaTweetorials
#EPeeps
1/10
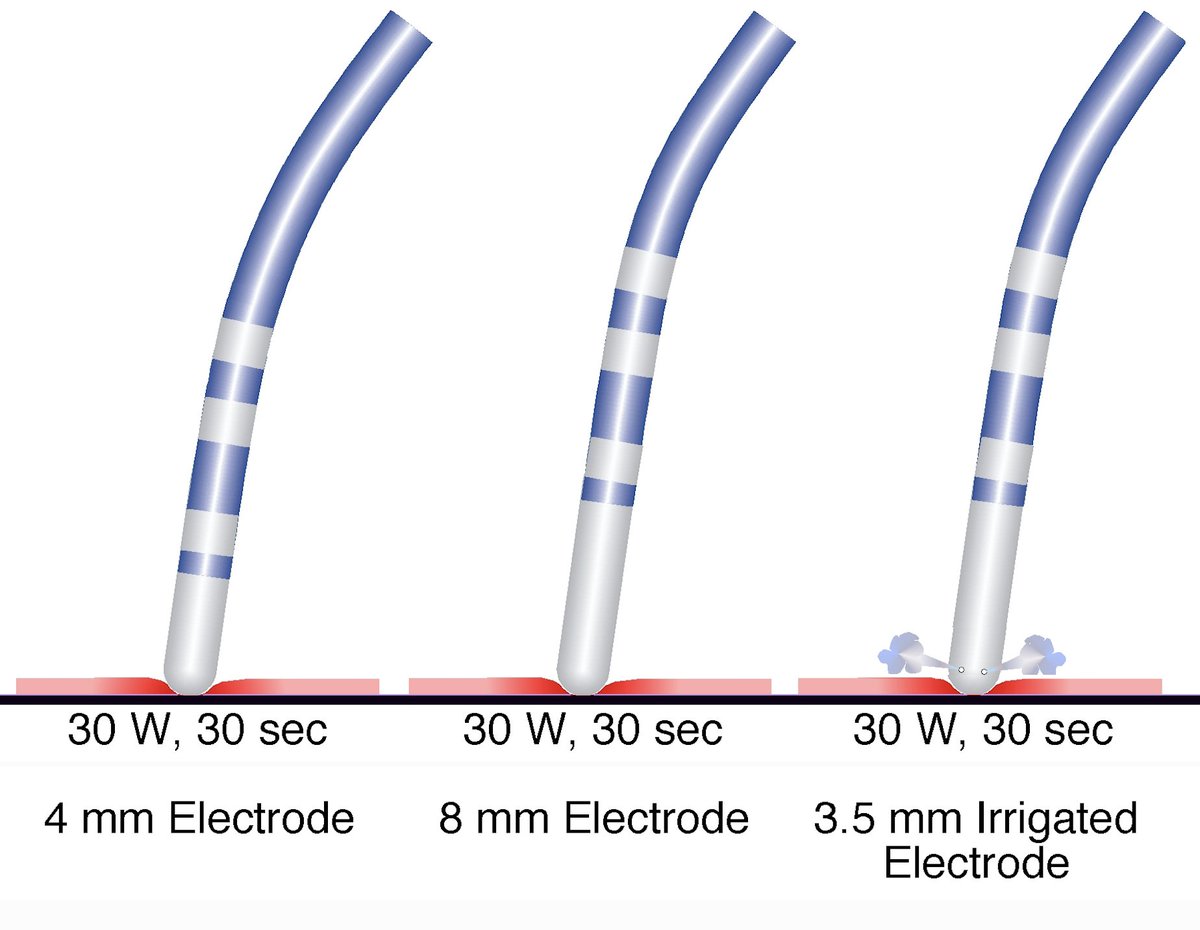
Q: If you could deliver 30 W of RF energy for 30 sec using any of the ablation (abl) electrodes shown in the figure, which RF ablation catheter creates larger ablation lesion size?
A: Let’s talk about how the RF abl lesion is formed.
#EPeeps
1/10
Q: If you could deliver 30 W of RF energy for 30 sec using any of the ablation (abl) electrodes shown in the figure, which RF ablation catheter creates larger ablation lesion size?
A: Let’s talk about how the RF abl lesion is formed.
2/10
The size of the lesion created by RF is determined by the amount of tissue heated to >>50°C.
Heat is generated when charged ions in tissue oscillate rapidly (following the alternating RF current) converting RF energy to kinetic/thermal energy (Ohmic/Resistive Heating)
The size of the lesion created by RF is determined by the amount of tissue heated to >>50°C.
Heat is generated when charged ions in tissue oscillate rapidly (following the alternating RF current) converting RF energy to kinetic/thermal energy (Ohmic/Resistive Heating)

3/10
According to Ohm’s law, the amount of power per unit volume (resistive heating) equals the square of current density times the impedance (resistance) of the tissue, which in turn, is a function of the square of RF current density.
According to Ohm’s law, the amount of power per unit volume (resistive heating) equals the square of current density times the impedance (resistance) of the tissue, which in turn, is a function of the square of RF current density.

4/10
RF current density (and power dissipation per unit volume) decreases rapidly (with the 4th power of distance) as it distributes radially from abl electrode. Thus, only a thin (<2 mm) rim of tissue in contact with the electrode is directly heated by RF (Resistive Heating)
RF current density (and power dissipation per unit volume) decreases rapidly (with the 4th power of distance) as it distributes radially from abl electrode. Thus, only a thin (<2 mm) rim of tissue in contact with the electrode is directly heated by RF (Resistive Heating)

5/10
Heat is then conducted into deeper layers of myocardium (Conductive Heating), which extends the abl lesion size.
Heat is also conducted back to the circulating blood pool and to the metal ablation electrode. This heat loss opposes myocardial heating and lesion formation.
Heat is then conducted into deeper layers of myocardium (Conductive Heating), which extends the abl lesion size.
Heat is also conducted back to the circulating blood pool and to the metal ablation electrode. This heat loss opposes myocardial heating and lesion formation.

6/10
When power output is fixed, a larger abl electrode creates smaller lesion size by 2 mechanisms:
(1) It exposes more of the electrode surface area to the cooling effect of blood.
(2) It reduces RF current density (due to larger surface area), which reduces tissue heating.
When power output is fixed, a larger abl electrode creates smaller lesion size by 2 mechanisms:
(1) It exposes more of the electrode surface area to the cooling effect of blood.
(2) It reduces RF current density (due to larger surface area), which reduces tissue heating.

7/10
Active cooling of the abl electrode and tissue surface by irrigation increases the amount of heat loss from the tissue (acting as a heat sink) and can reduce lesion size in the setting of a fixed RF power delivery.
Active cooling of the abl electrode and tissue surface by irrigation increases the amount of heat loss from the tissue (acting as a heat sink) and can reduce lesion size in the setting of a fixed RF power delivery.
8/10
In our question, power delivered to tissue is fixed. However, the proportion of heat stolen from tissue by abl electrode & blood is least (& current density is higher) with small non-irrigated electrode. Thus, heat remaining in tissue is maximized & lesion size is larger.
In our question, power delivered to tissue is fixed. However, the proportion of heat stolen from tissue by abl electrode & blood is least (& current density is higher) with small non-irrigated electrode. Thus, heat remaining in tissue is maximized & lesion size is larger.

9/10
So, why do we use large or irrigated abl electrodes?
The temperature of small non-irrigated abl electrodes rises quickly, which limits RF energy delivery (in temp-controlled mode) and can precipitate coagulum formation, which increases impedance and limits power delivery.
So, why do we use large or irrigated abl electrodes?
The temperature of small non-irrigated abl electrodes rises quickly, which limits RF energy delivery (in temp-controlled mode) and can precipitate coagulum formation, which increases impedance and limits power delivery.

10/10
When RF power output is unlimited, cooling of the abl electrode passively (by using a larger electrode size) or actively (by using saline irrigation) helps to avoid electrode-tissue interface overheating, allowing for greater power delivery and creation of larger lesions.
When RF power output is unlimited, cooling of the abl electrode passively (by using a larger electrode size) or actively (by using saline irrigation) helps to avoid electrode-tissue interface overheating, allowing for greater power delivery and creation of larger lesions.

• • •
Missing some Tweet in this thread? You can try to
force a refresh




