Canada is almost 70% fully vaccinated. Only 5 states are close to that level in the US. Why?
% Fully vaccinated disparity:
12 states 60-70%
19 states 50-60%
19 states 40-50%
nytimes.com/interactive/20…
% Fully vaccinated disparity:
12 states 60-70%
19 states 50-60%
19 states 40-50%
nytimes.com/interactive/20…

The 15% disparity between US and Canada is 50 million people. Not trivial difference.
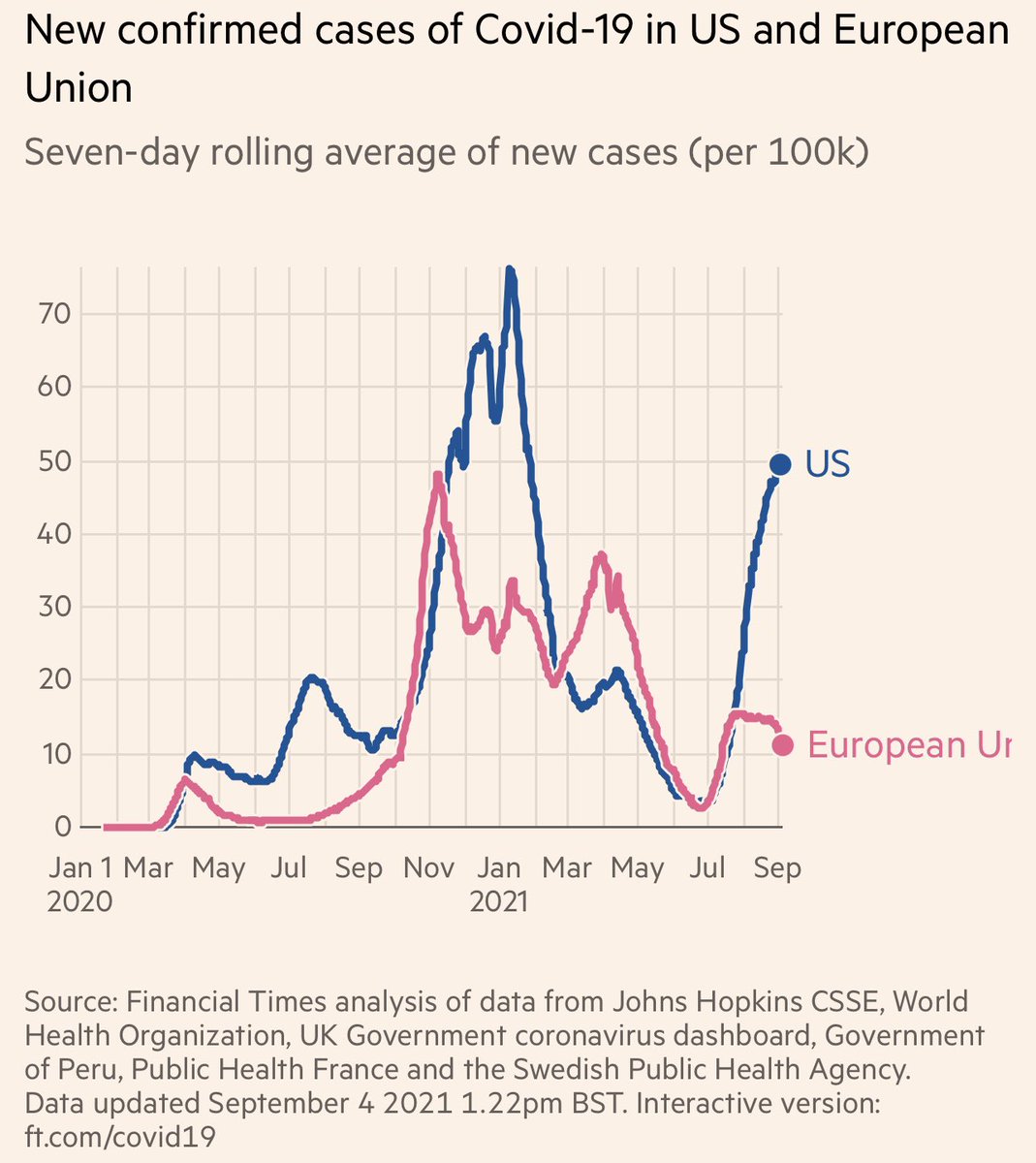
Now let's see what happens in well vaccinated country which also is a role model for adherence to other protective measures.
https://twitter.com/vincentrk/status/1440000231492526083
Basically we have overwhelming data, not just from the randomized trials, but also from multiple real world studies that vaccines are highly effective in preventing severe disease. Why we cannot translate this information into getting our vaccination rates to >70% is just sad.
https://twitter.com/vincentrk/status/1438935018127101956
• • •
Missing some Tweet in this thread? You can try to
force a refresh