
So as a junior myeloma faculty, I see a lot of consults for MGUS. Heres a tweetorial on how to interpret light chain values in the setting of kidney disease, as light chains are often checked to look for plasma cell disorders when patients have CKD.
🧵 #mmsm #MedTwitter
🧵 #mmsm #MedTwitter
So some basics first-
As immunoglobulins are made by normal plasma cells, free light chains are produced in excess of heavy light chains and spilled over in the kidneys.
As immunoglobulins are made by normal plasma cells, free light chains are produced in excess of heavy light chains and spilled over in the kidneys.
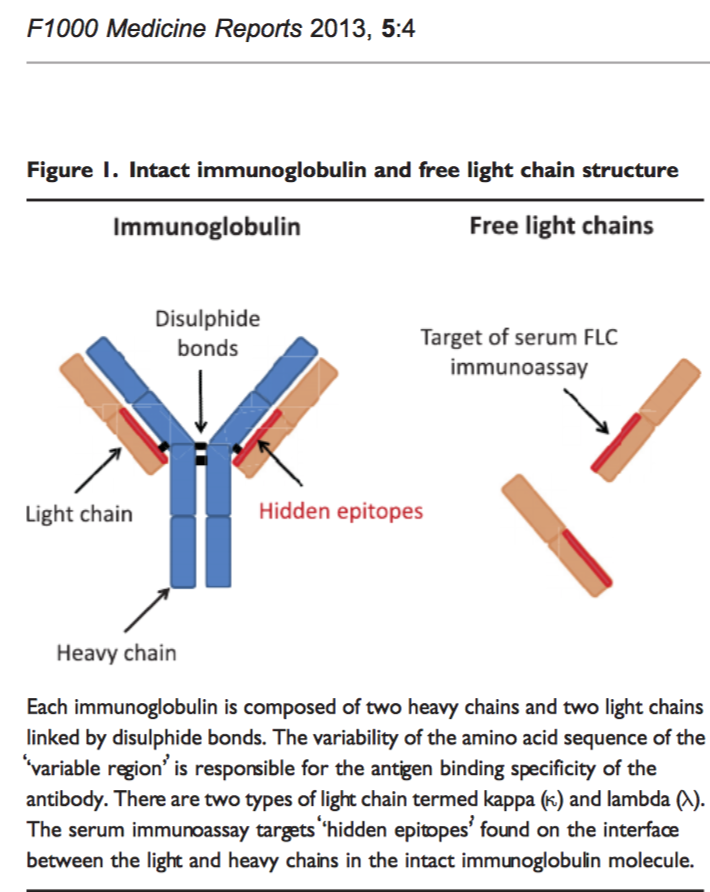
These excess "polyclonal FLC" are then released into the serum, from where they are rapidly removed by the kidneys with a half-life of 2 to 6 h..
So when creatinine clearance falls, it is only expected for these FLC to rise!
So when creatinine clearance falls, it is only expected for these FLC to rise!
You would expect for in renal failure due to non monoclonal plasma cell causes to result in a "proportional" rise of both kappa and lambda, with a preserved ratio!
But is that really the case?
But is that really the case?
Well-
Normally kappa FLC are produced more often than lambda.. BUT lambda more frequently forms dimers, which doubles their molecular weight and slows their renal clearance...
Normally kappa FLC are produced more often than lambda.. BUT lambda more frequently forms dimers, which doubles their molecular weight and slows their renal clearance...
Thus in normal situations, kappa/lambda ratio is actually usually slightly less than 1, since lambda sticks around in blood more than kappa.
But when there is kidney dysfunction, the reticuloendothelial system becomes an important route for clearance!
Because this route is not influenced by the weight of FLC, the median kappa/lambda FLC ratio increases with CKD stage. Hence, the serum ratio starts reflecting the higher kappa production rate as the GFR decreases!
So thats why most "MGUS" consults in patients with CKD have a "kappa" light chain higher than lambda! And hence an abnormal ratio, even though there isnt really a monoclonal cause.
Before you move to next tweet in thread, a poll!
Whats the average kappa light chain in somebody on dialysis? (due to a non-plasma cell mediated cause)
All values in mg/L
Whats the average kappa light chain in somebody on dialysis? (due to a non-plasma cell mediated cause)
All values in mg/L
130!!!! So thats how high the kappa light goes!
And hence,an adjusted kappa/lambda ratio from "0.26 to 1.65" to "0.37 to 3.1" has been suggested to better pick up "monoclonal" causes of light chain elevation in patients with kidney disease.
Reference:
cjasn.asnjournals.org/content/3/6/16…
And hence,an adjusted kappa/lambda ratio from "0.26 to 1.65" to "0.37 to 3.1" has been suggested to better pick up "monoclonal" causes of light chain elevation in patients with kidney disease.
Reference:
cjasn.asnjournals.org/content/3/6/16…

There were some simplifications here in this thread, but will be helpful for fellows interpreting these values, and for non-hematologists who place these consults!
Thanks for reading, and thanks to my amazing team at @huntsmancancer for guiding me through these situations (END)
Thanks for reading, and thanks to my amazing team at @huntsmancancer for guiding me through these situations (END)
• • •
Missing some Tweet in this thread? You can try to
force a refresh



