
1. Congrats Dr. Heinemann and authors that evaluated the long-term post-transplant outcomes for pts with autoimmune liver diseases comparing living & deceased after brain death donor liver transplantation using the European Liver Transplant Registry. #ph260720 #AJT @amjtransplant
2. In this study, the authors studied 29902 patients from transplanted (including 1003 living donor liver transplant [LDLT] patients) for autoimmune liver diseases between 1998-2017.
onlinelibrary.wiley.com/doi/abs/10.111…
#ph260720 #ELTR #LDLT @ELITA_ELTR
onlinelibrary.wiley.com/doi/abs/10.111…
#ph260720 #ELTR #LDLT @ELITA_ELTR
3. onlinelibrary.wiley.com/doi/abs/10.111… After risk-adjustment, both adult and pediatric LDLT recipients had a higher hazard of death if they had primary sclerosing cholangitis (PSC). This hazard was equivalent between the graft types for other liver diseases (AIH, ALD & PBC).
#ph260720 #PSC
#ph260720 #PSC
4. This is a controversial finding. Why do similar research questions yield dramatically different results? What are the implications of these findings and what should future studies seek to address? I’ll explore some of these points in this thread. #ph260720 #PSC 
5. You have a patient with PSC listed for liver transplantation. The patient has a potential living donor available. How do you proceed? #ph260720 #PSC #LDLT
6. First of all, what is PSC? Primary sclerosing cholangitis is a liver disease where the bile ducts (small tubes that carry bile from the liver to the gallbladder and intestines) become inflamed and scarred. This causes stasis of bile which damages the liver.
#ph260720 #PSC
#ph260720 #PSC

7. For severely damaged livers, or end-stage liver disease, liver transplantation is the only definitive treatment.
#ph260720 #amjtransplant @UHNTransplant
#ph260720 #amjtransplant @UHNTransplant

8. What is living donor liver transplantation (LDLT)? This is a type of liver transplantation in which portion of the liver from a healthy living person is removed and placed into someone whose liver is no longer working properly. #ph260720 #LDLT @TVASurg pie.med.utoronto.ca/TVASurg/projec…
9. After LDLT, the donor’s remaining liver regrows and returns to its normal size, volume and capacity within a couple of months after surgery. At the same time, the transplanted liver grows and restores the normal liver function in the recipient.
#ph260720 #LDLT
#ph260720 #LDLT

10. LDLT represents the main graft type used in many countries in Asia, whereas the predominant liver graft type in the West come from deceased donors The LDLT procedure is complex and high-risk (Petrowsky et al COOT 2019).
#ph260720 #LDLT @CO_Organ_Transp
#ph260720 #LDLT @CO_Organ_Transp

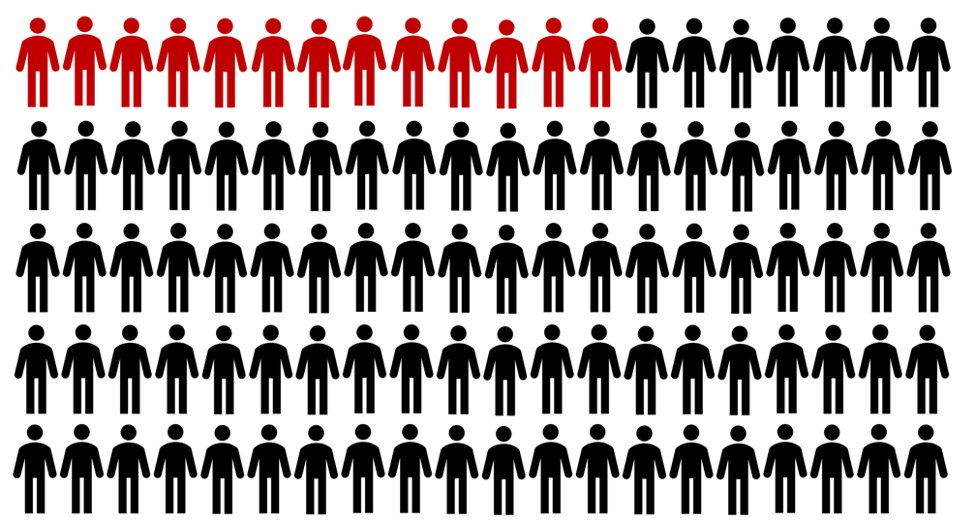
11. There are more liver transplant candidates than there are donors, resulting in 1 in 8 patients dying while awaiting a life-saving transplant. LDLT can offer waitlist candidates the option of earlier transplantation, and therein decrease waitlist mortality.
#ph260720 #UNOS
#ph260720 #UNOS
12. The Model for End-Stage Liver Disease (MELD)-based liver graft allocation for transplantation was introduced in 2002. This score is based on three laboratory variables. A higher MELD score determines txp priority and reflects a greater degree of urgency.
#ph260720 #UNOS
#ph260720 #UNOS

13. Since the introduction of the MELD score, patients with PSC have been significantly more likely to receive a LDLT when compared to patients without PSC.
#ph260720 #LDLT @UHNTransplant
#ph260720 #LDLT @UHNTransplant

14. Almost 15% of all transplant recipients with PSC receive a LDLT (compared with 4% of non-PSC patients) despite only comprising 6% of the overall deceased donor liver transplant population.
#ph260720 #PSC
#ph260720 #PSC

15. Why are PSC patients receiving LDLT at a higher proportion than other diseases? PSC is a disorder poorly served by a score such as MELD which may not adequately capture unique clinical features better reflecting severity of illness. (Shocho Noun Project)
#ph260720 #PSC
#ph260720 #PSC

16. So, how are PSC patients doing on the transplant waitlist relative to non-PSC after the implementation of MELD score for organ allocation? #ph260720 #PSC
17. A study by Goldberg et al. found that after risk-adjustment, patients with PSC had a 16% lower hazard of death compared to non-PSC patients. #ph260720 #PSC
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…
18. Goldberg et al. called into question prevailing practices of preemptive referral of PSC pts for living donor txp or providing exception points to reduce inequities resulting from a sole reliance on MELD for allocation.
ncbi.nlm.nih.gov/pmc/articles/P…
#ph260720 #MELD @LTxJournal
ncbi.nlm.nih.gov/pmc/articles/P…
#ph260720 #MELD @LTxJournal
19. So, what have previous studies found for outcomes of LDLT vs. DDLT in PSC patients vs. other patients? Of note, these include patients who all made it to transplantation, and does not take into account patients who died while waiting for a transplant.
#ph260720 #LDLTvsDDLT
#ph260720 #LDLTvsDDLT
21. The authors (Goldberg et al.) used the OPTN/UNOS liver transplant data from the US (2002-2012). 2103 LDLTs and 46674 DDLTs were identified.
#ph260720 #LDLT @HEP_Journal
ncbi.nlm.nih.gov/pmc/articles/P…
#ph260720 #LDLT @HEP_Journal
ncbi.nlm.nih.gov/pmc/articles/P…
22. LDLT recipients txped at experienced centers with cholestatic liver disease (PSC) had 24% lower graft failure risk than DDLT recipients. The risk of death after txp equivalent btw LDLT and DDLT for less-experienced ctrs.
#ph260720 #LDLT @HEP_Journal
ncbi.nlm.nih.gov/pmc/articles/P…
#ph260720 #LDLT @HEP_Journal
ncbi.nlm.nih.gov/pmc/articles/P…
23. Kashyap et al. found superior post-transplant survival for LDLT (5 year 92.5% vs. 84.9% for DDLT p=0.002). After risk-adjustment, LDLT was associated with a 60% lower hazard of death post-transplant compared to DDLT.
#ph260720 #UNOS @JournalofGISurg
pubmed.ncbi.nlm.nih.gov/20617395/
#ph260720 #UNOS @JournalofGISurg
pubmed.ncbi.nlm.nih.gov/20617395/
24. What about recurrence? It has been hypothesized that because LDLT includes a graft with some genetic similarity to the recipient, the risk of PSC recurrence maybe higher. So, is LDLT associated with an increased risk of PSC recurrence?
#ph260720 #PSCrecurrence
#ph260720 #PSCrecurrence
25. What proportion of patients with PSC experience disease recurrence within 5-years of liver transplantation?
#ph260720 #PSC
#ph260720 #PSC
26. Studies from North America (Gordon et al. liver Transpl 2016) and Japan (Egawa et al. Am J Transplant 2011) using multicenter national transplant data have found that the recurrence rate of PSC after liver transplantation ranges from 21% to 32% at 5 years.
#ph260720 #PSC
#ph260720 #PSC

27. So, what about disease recurrence of PSC after liver transplantation comparing graft types? #ph260720 #PSC
28. Heinemann et al. in their ELTR analysis, found that primary disease recurrence as a cause of death was higher in PSC patients having undergone living donor liver transplant versus. Dcsd donor liver txp (2.6% vs. 0.7%;p=0.044).
#ph260720 #ELTR @ELITA_ELTR @amjtransplant
#ph260720 #ELTR @ELITA_ELTR @amjtransplant
29. Heinemann et al. also found in their ELTR analysis that the risk-adjusted hazard of death from primary disease recurrence and biliary complications were higher in PSC pts after living donor vs. deceased donor liver transplantation.
#ph260720 #ELTR @ELITA_ELTR @amjtransplant
#ph260720 #ELTR @ELITA_ELTR @amjtransplant
30. Other groups have failed to corroborate a higher likelihood of PSC recurrence in living donor liver transplantation vs. deceased donor liver transplantation (Gordon et al. Liver transpl 2016 and Aravinathan Am J Transplant 2016)
#ph260720 #PSC @LTxJournal @amjtransplant
#ph260720 #PSC @LTxJournal @amjtransplant
31. So, why are we seeing opposite findings in studies evaluating living and deceased donor liver transplant for PSC? And what are the clinical questions that remain to be answered?👇 #ph260720 #PSC
32. Heinemann et al. considered age, recipient sex, and year of transplant as relevant confounders which were adjusted for in the cox proportional hazard models. Could there be additional factors that should be accounted for?
#ph260720 #PSC @amjtransplant @ELITA_ELTR
#ph260720 #PSC @amjtransplant @ELITA_ELTR
33. Gordon et al. adjusted for age, sex, race, blood type, MELD, and status prior to txp (ICU, hospital or home). Kashyap et al. adjusted for age, sex, MELD, and BMI. These factors were considered confounders. But, what is confounding?
#ph260720 #PSC @HEP_Journal @JournalofGISurg
#ph260720 #PSC @HEP_Journal @JournalofGISurg
34. Confounding is a distortion of the association between an exposure and an outcome that occurs when the study groups differ with respect to other factors that influence the outcome.
#ph260720 #confounding @JohnsHopkinsEPI
#ph260720 #confounding @JohnsHopkinsEPI
35. In the image, age would be considered a confounder, as it is associated with both the exposure (physical inactivity) and the outcome (heart disease).
#ph260720 #confounding @JohnsHopkinsEPI
#ph260720 #confounding @JohnsHopkinsEPI

36. What about residual confounding and unmeasured confounding? How are they related and why are they relevant in studies evaluating the effect of graft type on survival after liver transplantation for PSC?
#ph260720 #confounding @JohnsHopkinsEPI
#ph260720 #confounding @JohnsHopkinsEPI
37. Residual confounding occurs when a confounder has not been adequately adjusted for in the analysis, e.g., by using too large categories (e.g., smoking vs. non-smoking). When in reality, there are several degrees of smoking status.
#ph260720 #confounding @JohnsHopkinsEPI
#ph260720 #confounding @JohnsHopkinsEPI

38. What is unmeasured confounding? This is the effect of variables that are confounders, but not measured /available in a registry. As a result, they cannot be properly adjusted for, potentially giving rise to biased effect estimates.
#ph260720 #confounding @JohnsHopkinsEPI
#ph260720 #confounding @JohnsHopkinsEPI

39. Moreover, the definition of PSC recurrence should meet strict diagnostic criteria, as proposed by Graziadei et al. It is unclear whether such rigorous classification is maintained in large multicenter registries such as UNOS and ELTR.
#ph260720 #PSC @HEP_Journal
#ph260720 #PSC @HEP_Journal

40. Why do inferences differ btw studies evaluating the effect of graft type (living or deceased donor) on survival after liver txp for PSC? These include statistical methods, the impact of residual and unmeasured confounding, as well as variable misclassification.
#ph260720 #PSC
#ph260720 #PSC
41. So, in deciding whether a living donor liver transplantation is appropriate for a patient with PSC, what questions remain to be addressed? See below 👇
#ph260720 #PSC
#ph260720 #PSC
42. Because not all patients make it to transplant, we should look at intention-to-treat survival. Essentially: what is the survival from the time of listing also taking into account patients dying on the waitlist?
#ph260720 #survival @sapisochin @NicoGoldaracena @JHepatology
#ph260720 #survival @sapisochin @NicoGoldaracena @JHepatology

43. What are confounding factors which should be addressed in future risk-adjusted analyses involving liver txp for PSC? Time between diagnosis and listing? Overlapping etiologies (e.g., PSC/AIH)? Degree of duct involvement? Ischemia time? Comment below.
#ph260720 #PSC
#ph260720 #PSC
44. The definition of graft failure and disease recurrence must be standardized. A recipient death with a functioning graft (i.e., death from a non-graft related cause) does not help in future graft failure prognostication.
#ph260720 #graftfailure
#ph260720 #graftfailure
45. Robust methods to account for patient clustering w/in centers and heterogeneity of post-txp outcomes across centers (e.g., higher center experience associated with improved survival hazard for LDLT in PSC) ncbi.nlm.nih.gov/pmc/articles/P…
#ph260720 #PSC @HEP_Journal
#ph260720 #PSC @HEP_Journal
46. Heinemann et al. presents an interesting study. While liver txp remains a life-saving and excellent option for PSC pts, the exact impact of graft type on survival (LDLT vs. DDLT) remains to be clarified. #ph260720 #PSC @amjtransplant @ELITA_ELTR
onlinelibrary.wiley.com/doi/abs/10.111…
onlinelibrary.wiley.com/doi/abs/10.111…
47. What do you think future studies in liver transplantation for PSC should seek to address?
#ph260720 #livertransplant #PSC
#ph260720 #livertransplant #PSC
• • •
Missing some Tweet in this thread? You can try to
force a refresh



