
First up for tweet-ucation on this final day of live #CHEST2021 is “The Wave of the Future: Beyond the Ultrasound Basics"! 1/
Dr. Orlando Garner (@ogarnerccm) will discuss "Brain Drain: Neuro-Ultrasound for the non-Neurointensivist." #CHEST2021 2/
Transcranial US anatomy and probe positioning. #CHEST2021 3/ 

You can assess midline shift. #CHEST2021 4/ 

Increased ICP will be seen as MCA decreased diastolic flow and a sharp upstroke initially, or even diastolic flow reversal in the setting of cerebral arrest. #CHEST2021 5/ 

Find the MCA anterior to the thalamus in the circle of willis. #CHEST2021 6/ 

You can estimate the ICP using the pulsatility index. #CHEST2021 7/ 

You can also use US to evaluate for vasospasm. #CHEST2021 8/ 

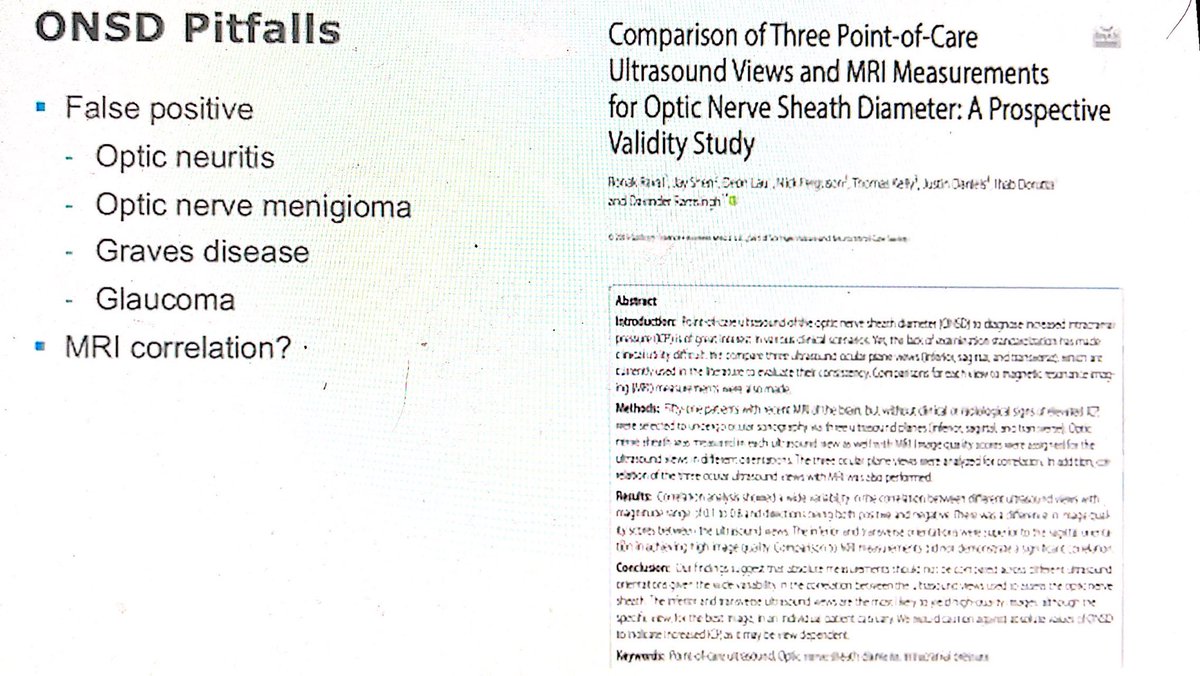
Measure the optic nerve sheath (bilaterally enlarged in increased ICP). Unilateral enlargement should change your differential (things like optic neuritis). #CHEST2021 9/ 



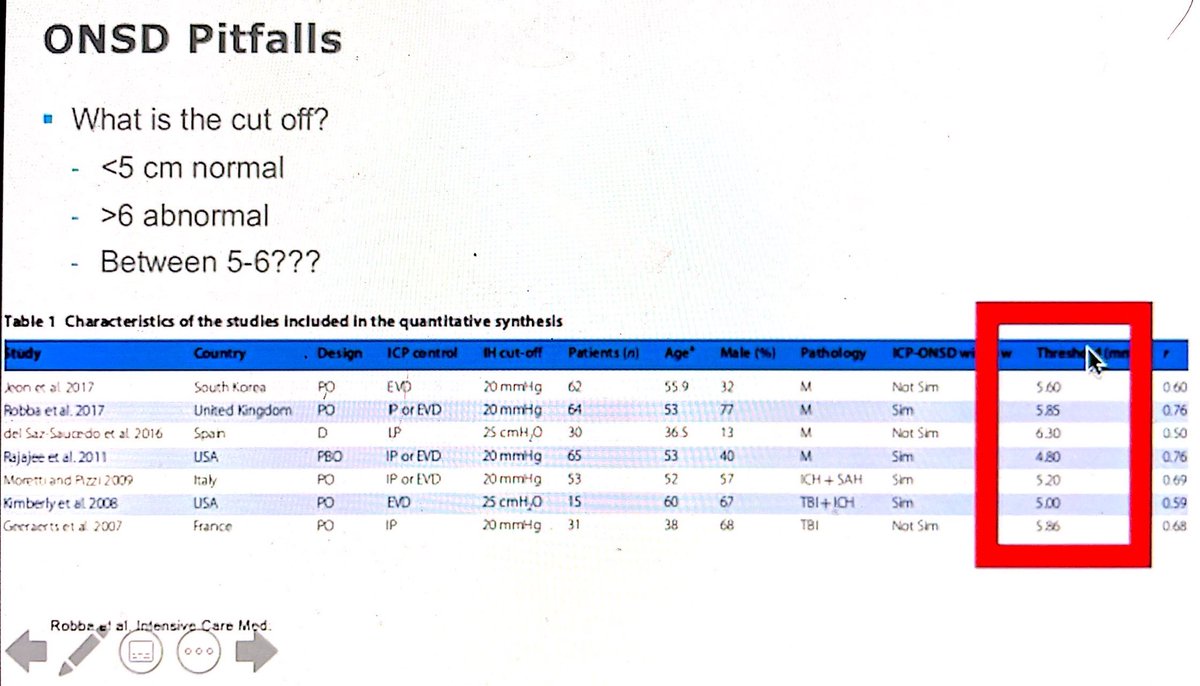
ONSD pitfalls #CHEST2021 10/ 



Take home points! #CHEST2021 11/ 
Dr. Ali Omranian will discuss "From the Neck Down: Upper Airway Ultrasonography and Confirmation of Tube and Line Placement." #CHEST2021 12/
(SLIDE)
(SLIDE)

You can use US to evaluate a tracheal intubation #CHEST2021 13/ 

Normal longitudinal view of upper airway #CHEST2021 14/ 

The linear probe gives the best view of the airway. #CHEST2021 15/ 

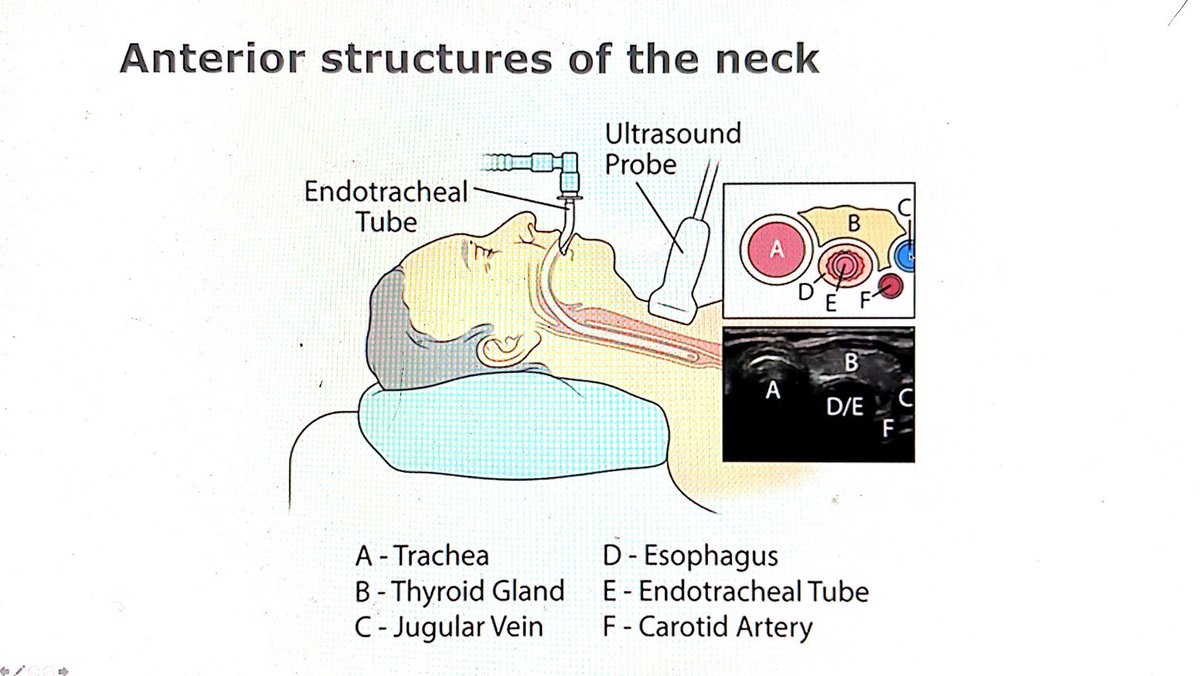
Anterior structures of the neck #CHEST2021 16/ 
Algorithm for US evaluation after intubation. #CHEST2021 17/ 

Caveats #CHEST2021 18/ 

US for intubation confirmation has been studied. #CHEST2021 19/ 



Philippe Rola (@ThinkingCC) will discuss "Avoiding the Michelin Men: How to Approach Venous Congestion". #CHEST2021 20/
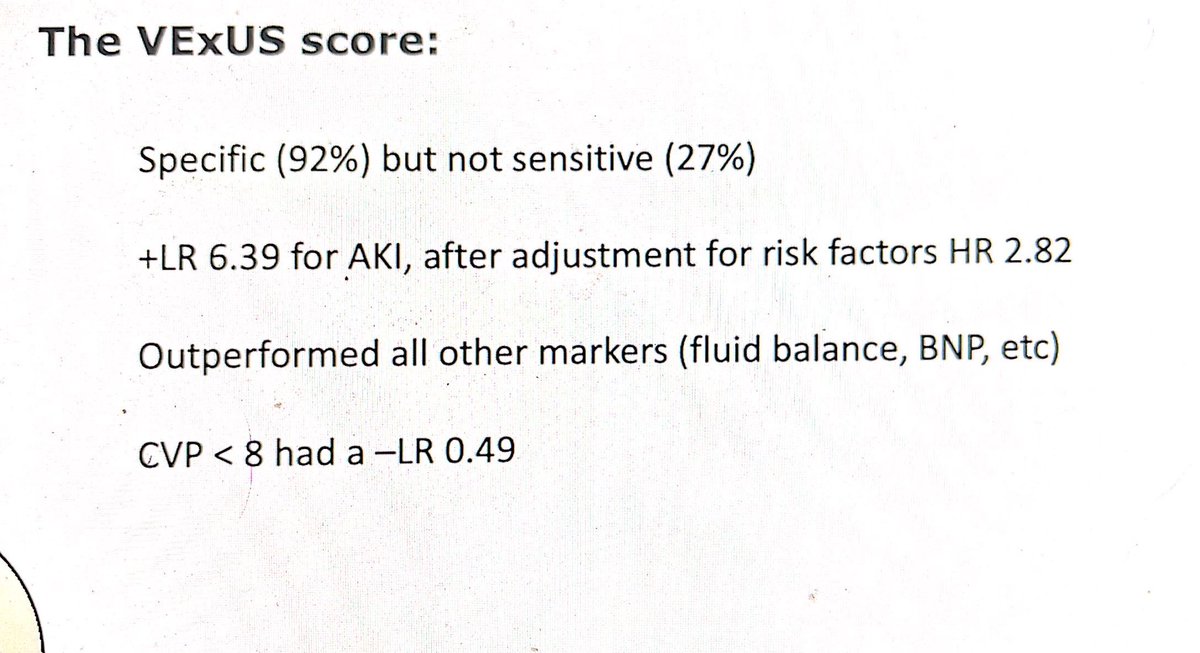
Asking the IVC whether a patient is fluid responsive is a beginner's question. #CHEST2021 21/ 
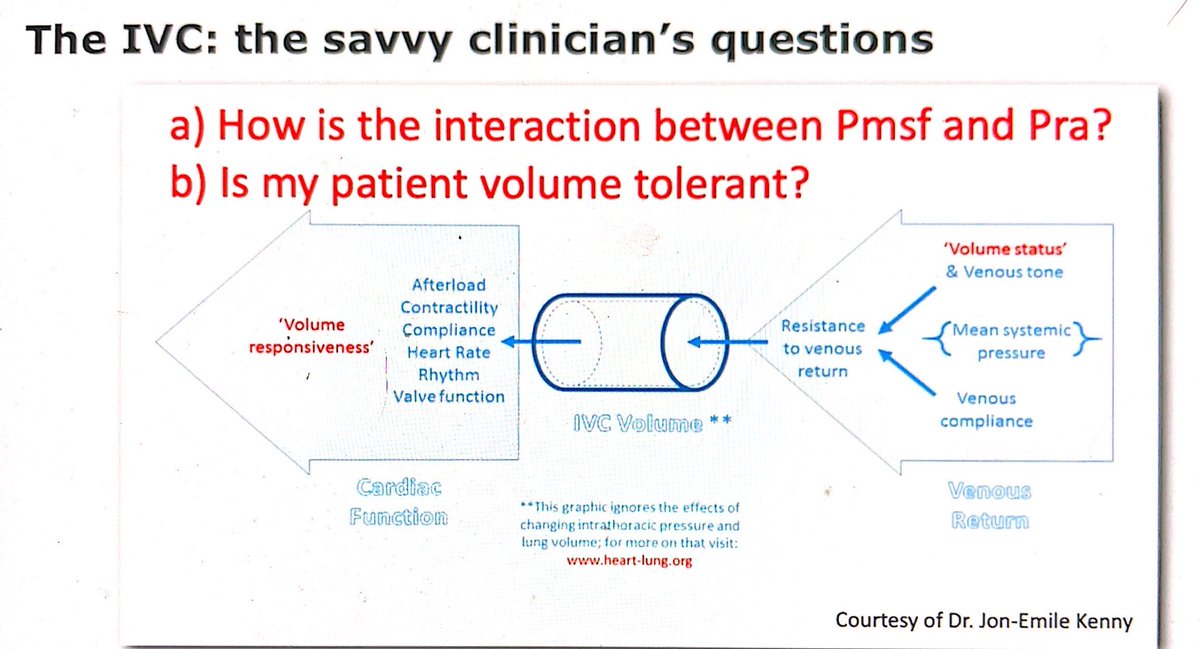
This study looked at the VExUS score for grading venous congestion. #CHEST2021 22/ 






Possible future fluid management philosophies to consider. #CHEST2021 23/ 

Dr. Alfredo Jardino will discuss "Waves of Breathlessness: POCUS for Ventilator Liberation." #CHEST2021 24/
Non-POCUS vent weaning protocols #CHEST2021 25/ 

POCUS weaning protocols #CHEST2021 26/ 

42% of weaning failures are related to the heart with decreased LV function after removed of positive pressure. #CHEST2021 27/ 

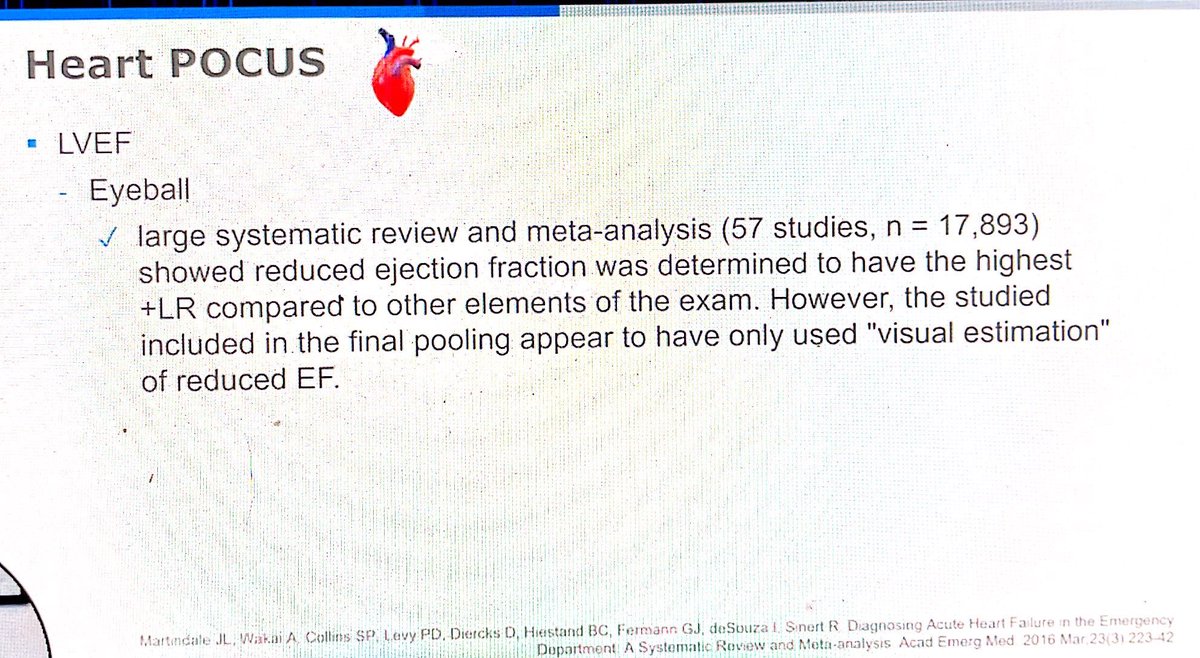
Start with an eyeball test of the LVEF. #CHEST2021 28/ 
The EPSS is 100% sensitive for predicting severe systolic dysfunction. #CHEST2021 29/ 



Can estimate filling pressures using E/A and E/e' ratios. #CHEST2021 30/ 

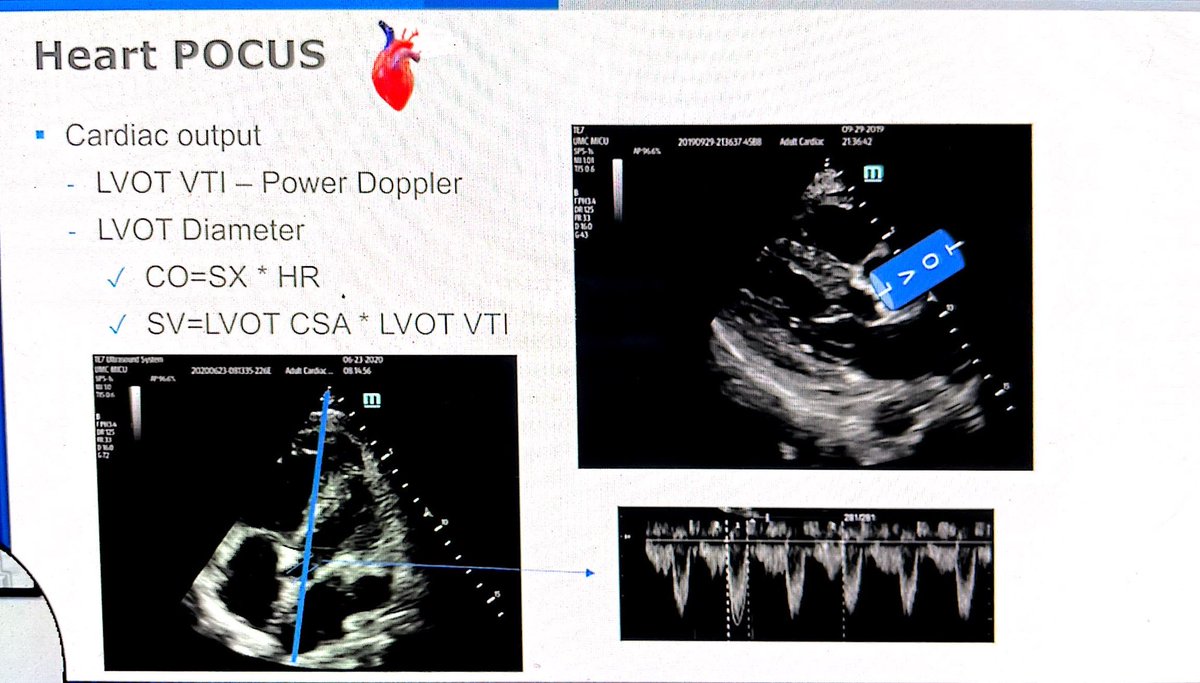
You can assess your cardiac output . #CHEST2021 31/ 
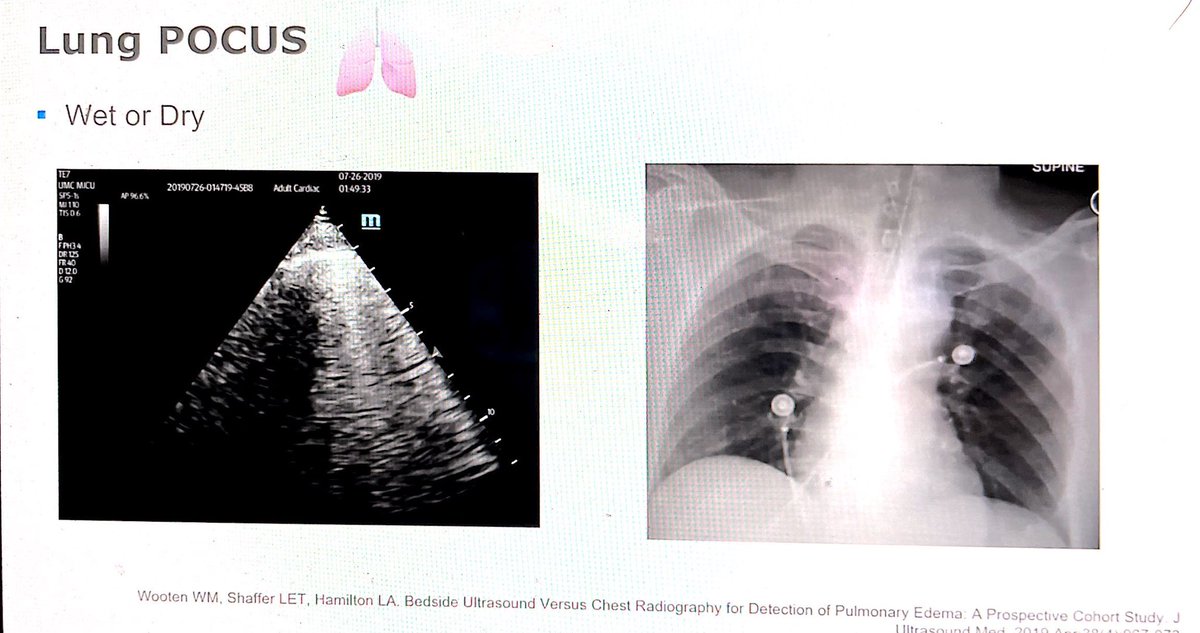
Lung POCUS can also be helpful, #CHEST2021 32/ 

B-lines can help identify pulmonary edema even with a normal CXR. #CHEST2021 33/ 
Hepatization of the lung can reflect de-recruited lung. #CHEST2021 34/ 

You can evaluate whether there is a pleural effusion. #CHEST2021 35/ 

Lung US score #CHEST2021 36/ 

The diaphragm makes 80% of the inspiratory effort. You can evaluate thickness fraction and diaphragmatic excursion. #CHEST2021 37/ 

Diaphragmatic thickness fraction can be measured during inspiration and exhalation. #CHEST2021 38/ 

Diaphragmatic excursion can also be evaluated. #CHEST2021 39/39 

• • •
Missing some Tweet in this thread? You can try to
force a refresh













