
My last live tweet-ucation for #CHEST2021 will be "Acute Respiratory Failure in Obstructive Lung Disease: Ventilation Strategies"! 1/
Dr. Daniel Ouellette will speak on "The role of NIPPV in obstructive lung disease." #CHEST2021 2/
This study showed reduced rates of intubation with the use of NIPPV for COPD exacerbations. #CHEST2021 3/ 







Per guidelines NIV should be used for patients with respiratory failure and a COPD exacerbation. #CHEST2021 4/ 

This meta-analysis shows moderate quality of evidence for the mortality and intubation rates. There was also a lower rate of complications of treatment and that quality of evidence was high. #CHEST2021 5/ 

HFNC was noninferior to NIV. #CHEST2021 6/ 



This smaller study also showed that HFNC was non-inferior. #CHEST2021 7/ 



This study showed that HFNC seems to have a similar benefit to NIV. #CHEST2021 8/ 



This meta-analysis compared different non-invasive O2 strategies and found that NIV improved important outcomes for patients with AECOPD, and several other interventions may be effective. #CHEST2021 9/ 







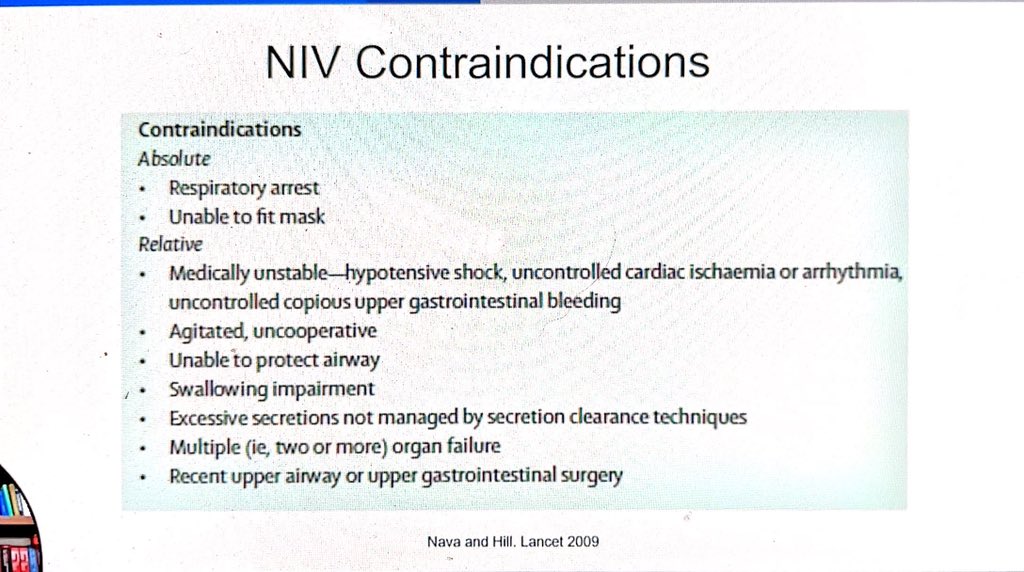
Contraindications to NIV. #CHEST2021 10/ 
Is there a role for NIV support AFTER intubation? #CHEST2021 11/ 

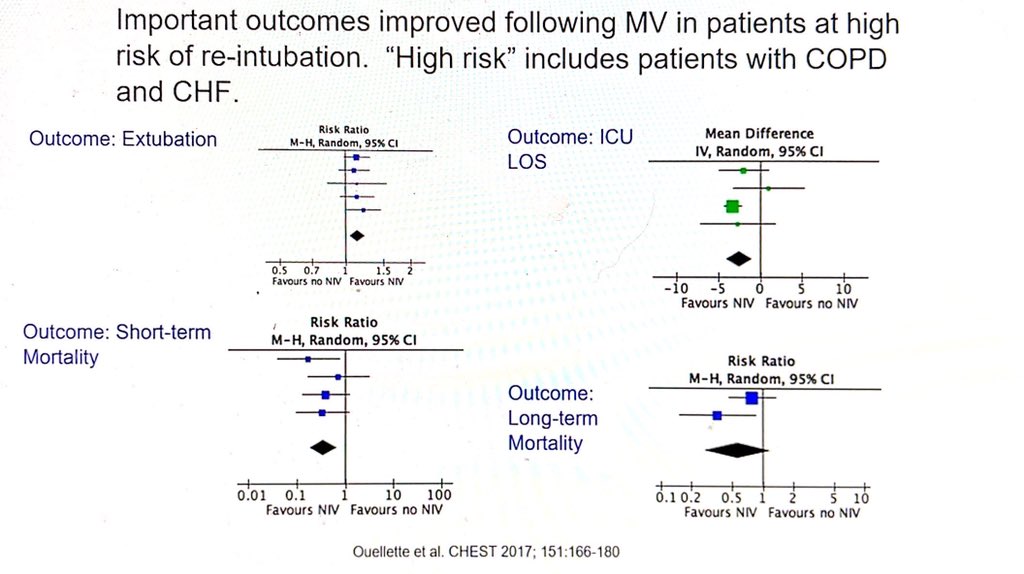
NIV following extubation for patients at high risk of re-intubation led to improved outcomes. #CHEST2021 12/ 
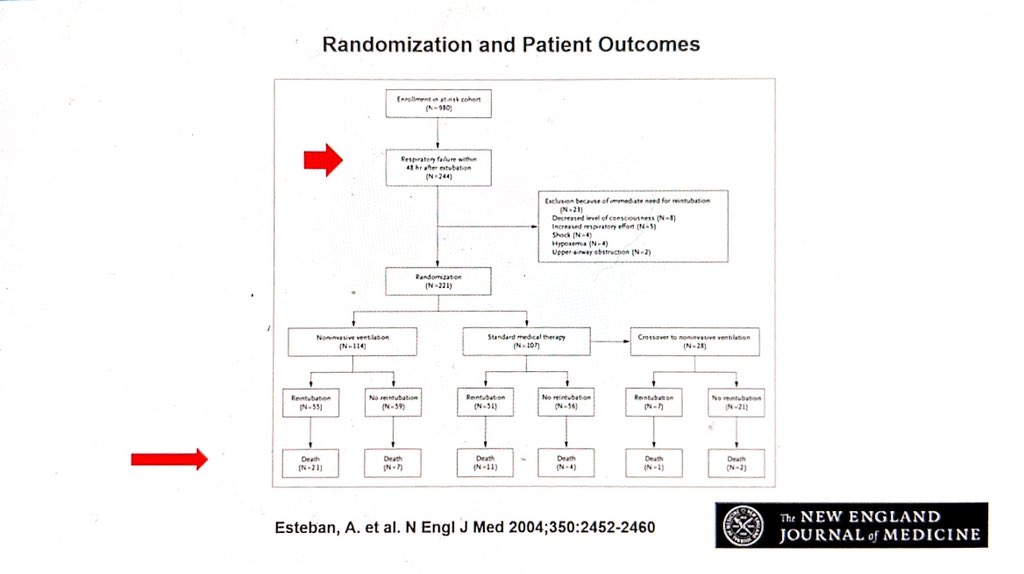
This NEJM 2004 study looked at a general population of patients with respiratory failure who were intubated. NIV was used after respiratory failure developed, and their outcomes were worse, though. The message is not to delay the use of NIV post-extubation. #CHEST2021 13/ 


HFNC is noninferior to NIV post-extubation. #CHEST2021 14/
NIV plus HFNC has improved outcomes. #CHEST2021 15/ 

Conclusions about post-extubation management for AECOPD. #CHEST2021 16/ 

Next is my dear friend and ventilator extraordinaire, Dr. Eduardo Mireles-Cabodevila will speak on "Ventilator strategies in obstructive lung disease"! #CHEST2021 17/
The mortality of mechanical ventilation for COPD is worse than asthma. #CHEST2021 18/ 

Obstructive lung diseases have increased airway resistance. #CHEST2021 19/ 

Resistance is the main driver. #CHEST2021 20/ 

Initially your goal is to minimize air trapping and later your goal shifts to liberation. You want to minimize time on the vent. #CHEST2021 21/ 

2 basic concepts include decreasing air trapping and minimizing dead space. #CHEST2021 22/ 
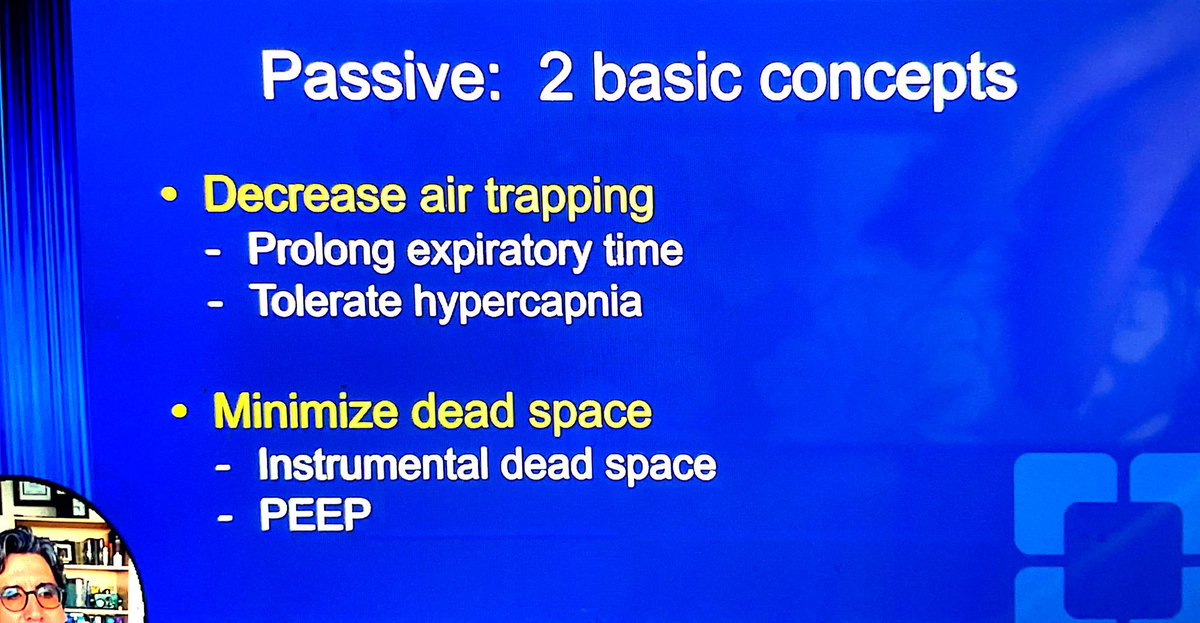
The time constant is the amount of time it takes the lungs to inflate or deflate. It is longer in obstructive lung diseases. #CHEST2021 23/ 
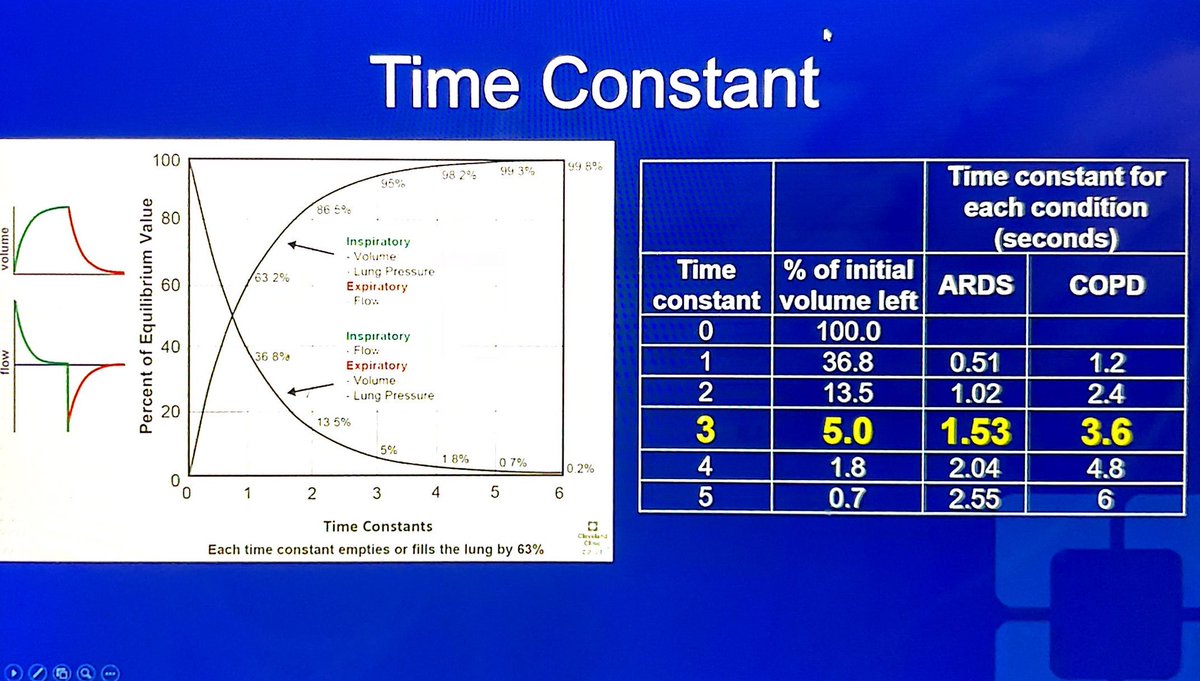
AutoPEEP worsens with a prolonged time constant. #CHEST2021 24/ 

With smaller TiV we normally increase the RR, but patients with COPD have a higher dead space so you need a higher RR to achieve good MiV. #CHEST2021 25/ 

You can either change the RR or the inspiratory time to improve the expiratory time. The rate is a more important determinant of expiratory time. #CHEST2021 26/ 

Peak pressures will be elevated due to the resistive load. #CHEST2021 27/ 

These factors are key in MV of patients with obstructive lung disease. #CHEST2021 28/ 

Why is PEEP important? #CHEST2021 29/ 

The message from this study is to monitor the plateau pressure as you apply PEEP to avoid over-distention. #CHEST2021 30/ 

Summary #CHEST2021 31/ 

Dr. Margaret Disselkamp will speak on "The burden of respiratory failure in asthma and COPD." #CHEST2021 32/
Asthma prevalence is increasing. #CHEST2021 33/ 



Asthma healthcare utilization #CHEST2021 34/ 

The good news is that the hospitalization rate is decreasing. #CHEST2021 35/ 

Asthma mortality is also decreasing #CHEST2021 36/ 

Asthma mortality worsens by age group with 4 times the risk of death in adults compared to children. #CHEST2021 37/ 
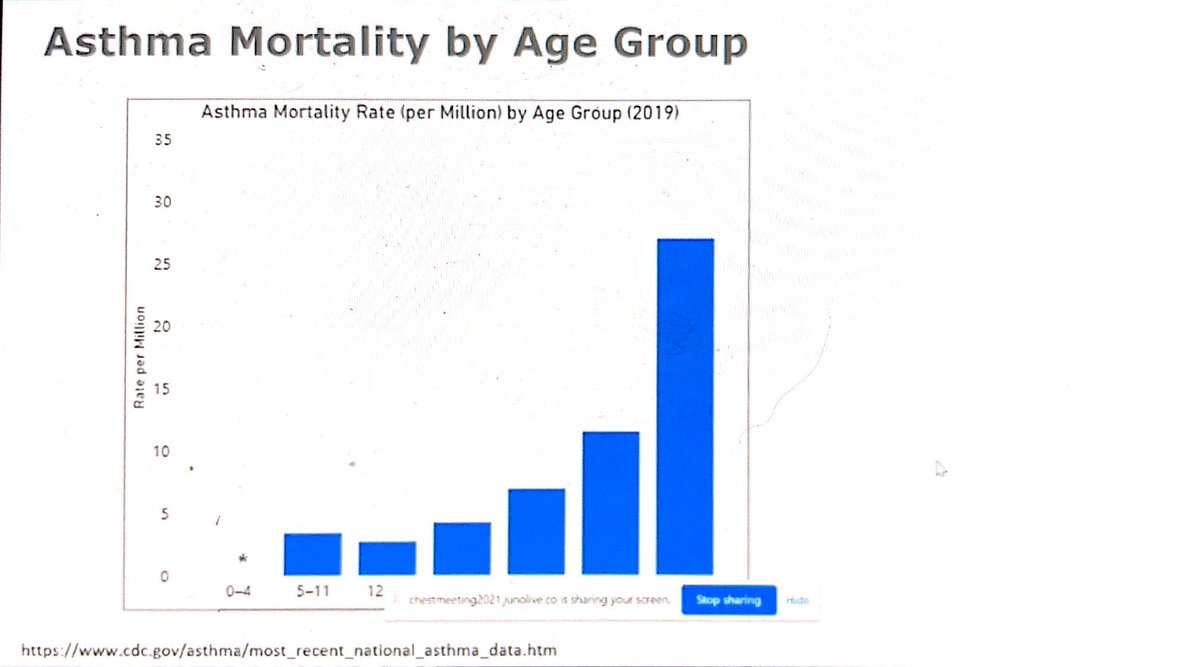
Non-hispanic blacks have the highest mortality rate. #CHEST2021 38/ 

Hospital admissions with asthma #CHEST2021 39/ 

Economic burden of asthma #CHEST2021 40/ 

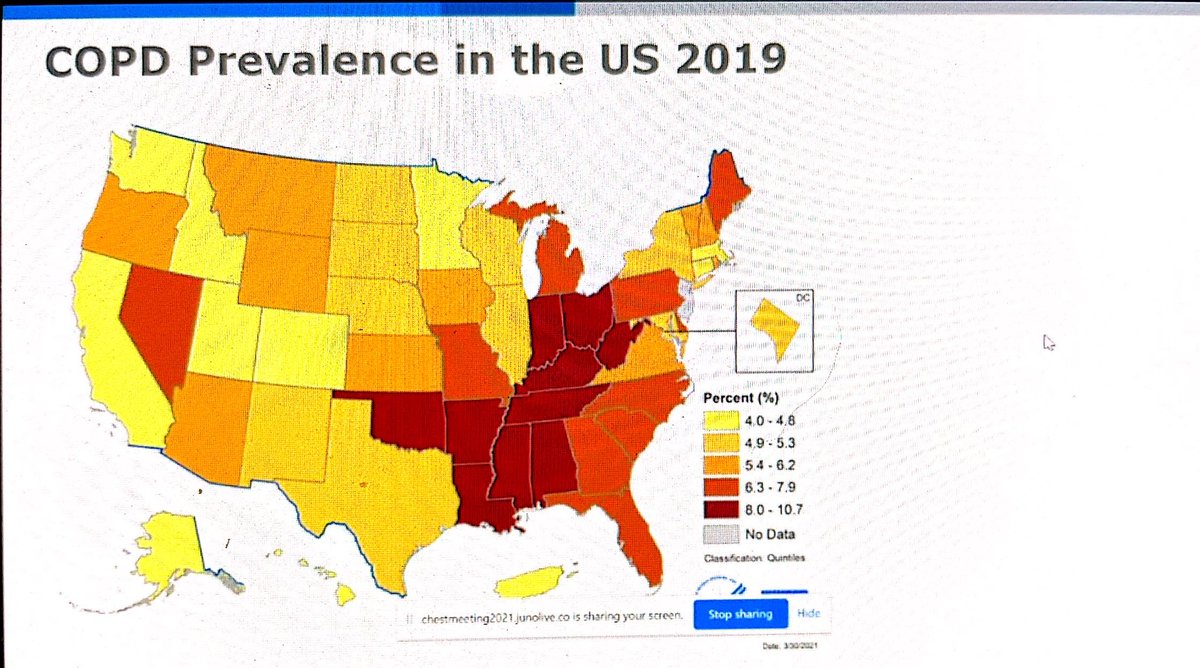
COPD prevalence in the US #CHEST2021 41/ 
COPD healthcare use #CHEST2021 42/ 

COPD mortality is decreasing #CHEST2021 43/ 

COPD age-adjusted death rate #CHEST2021 44/ 

COPD economic burden #CHEST2021 45/ 

Severe COPD exacerbations #CHEST2021 46/ 

Mechanical ventilation use in the ICU - Use has declined in COPD (blue line), but less for asthma (orange line). #CHEST2021 47/ 

Summary #CHEST2021 48/48 

• • •
Missing some Tweet in this thread? You can try to
force a refresh










