Last afternoon of #APSAD40! It is a joy to chair this session on #overdose - lots of key learnings and great work in the prevention space. Here are a couple of highlights from the session 1/
2/ Louisa Durrant (NUM at Melaleuca, @qldhealthnews) spoke about lessons learned supplying take-home naloxone in the opioid treatment program in QLD. Despite many having experienced an overdose, few had access to naloxone before the pilot, and consumers valued being offered THN. 





3/ Dr Eleanor Black presented on the ONE study, a pilot study looking at ED delivery of #naloxone - a key opportunity to offer naloxone to people at risk of overdose. Most (not all) staff through they should offer #naloxone, with common misconception of naloxone increased OD risk 
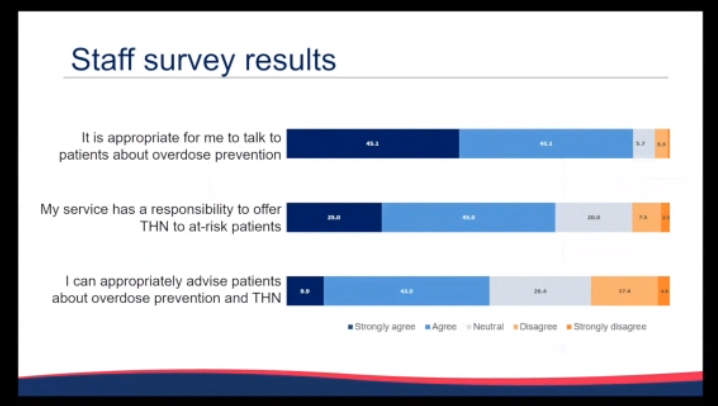
3/ Low provision of naloxone in ED suggest more work is needed to address barriers to supply in the ED 

5/ @DrTinaLam_AU presented at #APSAD40 on ED poisonings with prescription opioids .. work which has just been published in @AddictionJrnl (if you want to read more) onlinelibrary.wiley.com/doi/full/10.11…
6/ @DrTinaLam_AU - most poisonings were with more accessible opioids (codeine&oxycodone), with lower rates of harm for tapentadol & fentanyl relative to supply. Fentanyl&methadone more likely to be accidental poisonings, with intentional harm seen more with most other opioids 



7/ Dr Rachel Sutherland spoke on take-home fentanyl test strips. Most found FTS acceptable and were interested in drug checking. Some issues with misreading the strips (false positives). Harm reduction actions taken as a result of testing. Acceptable, but maybe not reliable? 







8/ Rapid Preso from Rosie Gilliver (Kirketon Road Centre) rapid review from a primary healthcare setting in Kings Cross, Sydney - exciting to see lots of outreach to supply naloxone outside the clinic, with strong staff support! 

9/ Rapid preso from PhD researcher Anna Conway (@KirbyInstitute) on opioid OD and naloxone access among people who recently used opioids or received opioid agonist treatment.. polysubstance use assoc with more OD and more THN access, TM associated with less OD and more THN! 



10/ @JMoullin talked about the importance normalising pharmacists attitudes towards naloxone, highlighting the importance of targeted implementation strategies.. and the challenges of implementation during a pandemic (sorry my slide short was fuzzy) 

• • •
Missing some Tweet in this thread? You can try to
force a refresh