
RFDS Central Ops (EGM Medical/Retrieval Services)
22 Nov,
30 tweets, 15 min read
Great work @acemonline SA team including @AWalterPerry organising tonight’s #COVID19 update with updates from Sydney, Melbourne & Adelaide 

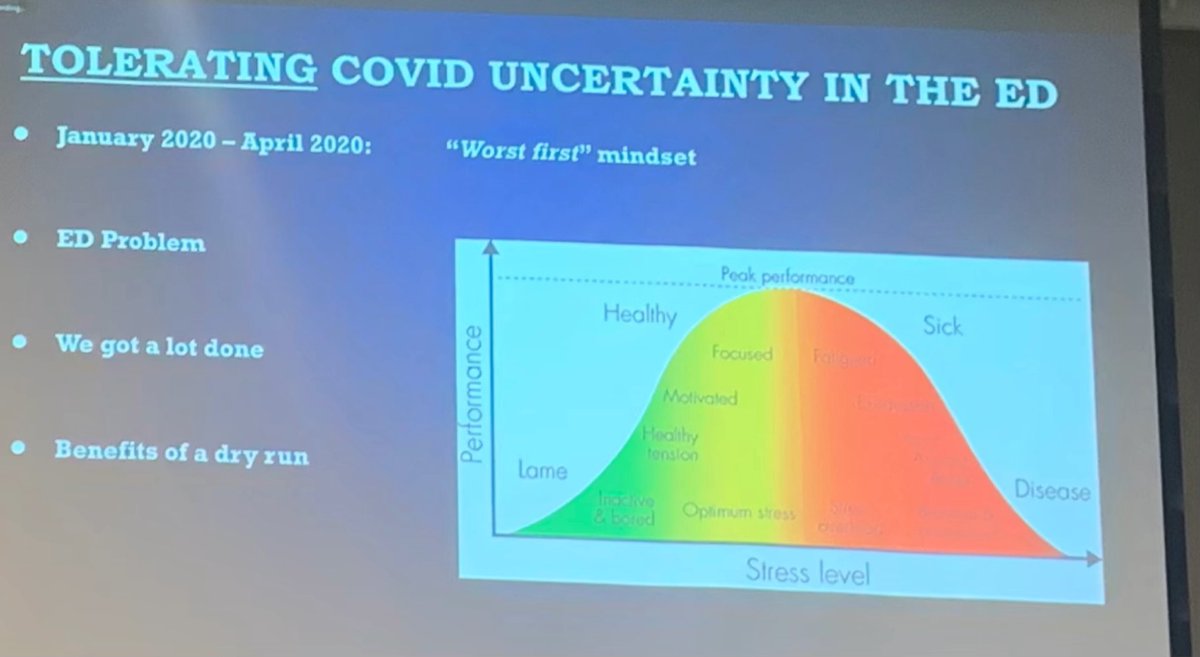
Tips from Dr Andrew Cooke, St George:
* Tolerate uncertainty - lesson 1
* an iterative approach to determining hot/cold zones, PPE etc
* workshopped training to build muscle memory
* accessible, continually updated guidelines via internal website

* Tolerate uncertainty - lesson 1
* an iterative approach to determining hot/cold zones, PPE etc
* workshopped training to build muscle memory
* accessible, continually updated guidelines via internal website
* getting used to proning; which patients qualify for HFNO
* Covid shuttle bus helped with ED flow for discharges from the ward/ED
* grief & disbelief when family members not allowed to visit
* stigma of being #COVID19 (+) delaying seeking care
* a lot of anxiety in patients

* Covid shuttle bus helped with ED flow for discharges from the ward/ED
* grief & disbelief when family members not allowed to visit
* stigma of being #COVID19 (+) delaying seeking care
* a lot of anxiety in patients


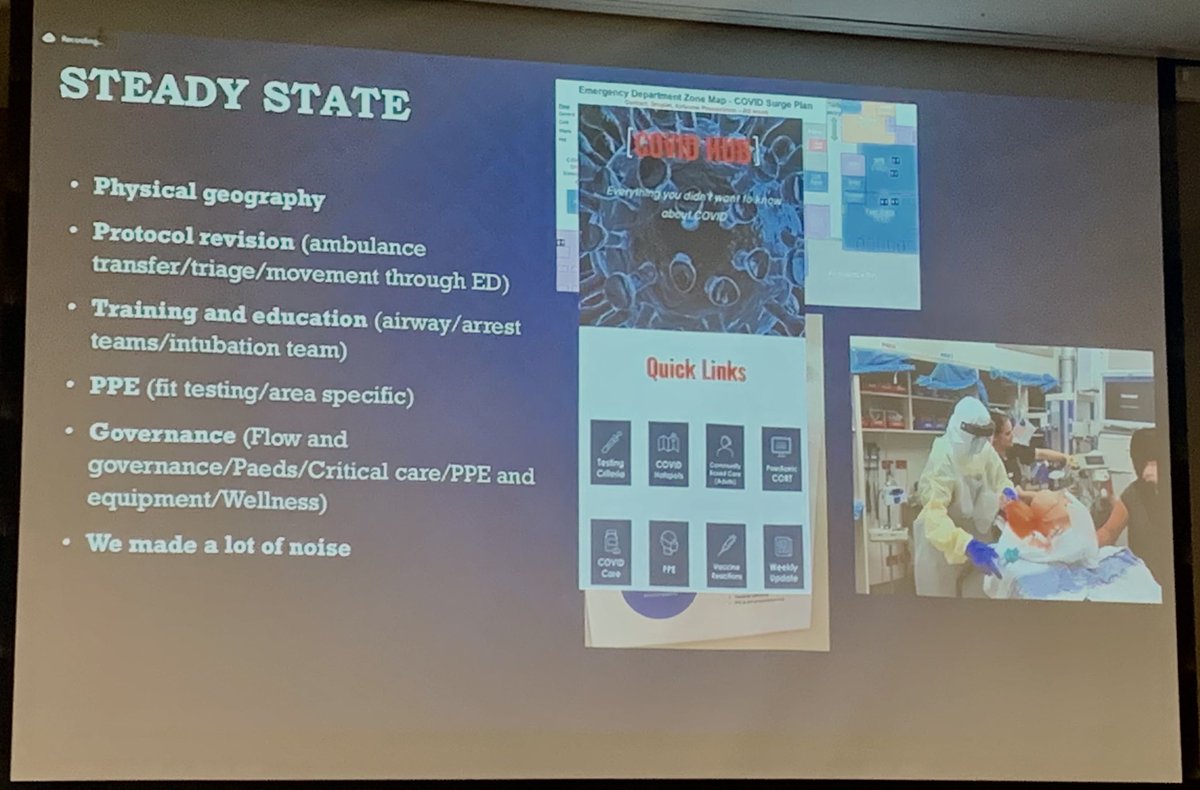
Moving ahead in the vaccinated world
* redesigning ED w single, (-) flow rooms
* hot/warm/cold zones
* “Covid assessment unit” helped ED flow
* be prepared to creatively use space - corridors, etc
* huddles to be agile with staff - ⬇️geographic staffing
* workshops > simulation
* redesigning ED w single, (-) flow rooms
* hot/warm/cold zones
* “Covid assessment unit” helped ED flow
* be prepared to creatively use space - corridors, etc
* huddles to be agile with staff - ⬇️geographic staffing
* workshops > simulation

* team well-being is not organic - it takes dedication to check in
* humble leadership matters
Thanks Andrew for a great overview of the journey. Next up: @DrSimonCraig from Monash
* humble leadership matters
Thanks Andrew for a great overview of the journey. Next up: @DrSimonCraig from Monash

The #PedsEM experience at Monash
* a spectrum of cases
* unvaxxed teen example- mild hypoxia & normal chest auscultation can betray significant pathology
* dex, antibiotics baricitanib
* significant disease requiring NIV
* a spectrum of cases
* unvaxxed teen example- mild hypoxia & normal chest auscultation can betray significant pathology
* dex, antibiotics baricitanib
* significant disease requiring NIV

The “close contact”
- managing staff when retrospectively exposed for non-Covid presentation who turns out to be positive days later
- all staff now w N95/face shield, gloves for patient contact, gown/apron for higher risk to mitigate this risk
- managing staff when retrospectively exposed for non-Covid presentation who turns out to be positive days later
- all staff now w N95/face shield, gloves for patient contact, gown/apron for higher risk to mitigate this risk
What about the Covid (+) child who is well enough to go home?
- transport protocols are important!
Is nitrous for sedation an AGP?
- treat all procedural sedation as high risk
- procedure, non neg pressure rooms with full PPE are probably ok
- transport protocols are important!
Is nitrous for sedation an AGP?
- treat all procedural sedation as high risk
- procedure, non neg pressure rooms with full PPE are probably ok
What really needs to be referred to the #COVID19 centre?
- have clear guidelines for your ambulance service
Consider multiple diagnoses
- #COVID19 can present with pneumonitis + myocarditis
Not everything is #COVID19!
- look for clubbing, chronicity for other underlying Dx
- have clear guidelines for your ambulance service
Consider multiple diagnoses
- #COVID19 can present with pneumonitis + myocarditis
Not everything is #COVID19!
- look for clubbing, chronicity for other underlying Dx
What about #MISC / #PIMSTS? Make sure to bear it in mind if you are thinking of Kawasaki on your differential.
What about mental health? Eating disorders increased during lockdowns.

What about mental health? Eating disorders increased during lockdowns.


Take homes in kids:
1) vaccines are awesome!
2) anyone could have #COVID19!
3) consistent PPE for everyone
4) single rooms are rapidly filled - you will need to be creative.
Thanks @DrSimonCraig - next up, Dr Nick Edwards, intensivist from the RAH
1) vaccines are awesome!
2) anyone could have #COVID19!
3) consistent PPE for everyone
4) single rooms are rapidly filled - you will need to be creative.
Thanks @DrSimonCraig - next up, Dr Nick Edwards, intensivist from the RAH

Oops nope, it’s Assoc Prof David Shaw, Head of Unit ID from CALHN! Let’s talk about testing for #COVID19 🧪🦠
* in-house PCR needs to amplify virus; 96% sensitive
* GenXpert rapid 4hrs is quicker - worldwide shortage of cartridges limiting
* rapid antigens: lower sensitivity
* in-house PCR needs to amplify virus; 96% sensitive
* GenXpert rapid 4hrs is quicker - worldwide shortage of cartridges limiting
* rapid antigens: lower sensitivity

Let’s talk rapid antigen testing
- low sensitivity one off
- day-in day-out testing likely to reveal an emerging infection
- asymptomatic has sensitivity 24%, symptomatic done day after day may have sensitivity up to 85%
Saliva PCR
- daily test for 3-5 days in a row⬆️
sens

- low sensitivity one off
- day-in day-out testing likely to reveal an emerging infection
- asymptomatic has sensitivity 24%, symptomatic done day after day may have sensitivity up to 85%
Saliva PCR
- daily test for 3-5 days in a row⬆️
sens


Serology - limited utility unless trying to diagnose a past infection
Do vaccines reduce transmission?
- YES
- by about 50%
Do vaccines reduce transmission?
- YES
- by about 50%

What about Novavax?
- old tech - some want to trust it
- really complex production
- aside - this guy has a hilariously dry sense of humour; lots of chuckles here: “if you want something mixed in moth cells and soap, well fine”
- trials: ongoing
- old tech - some want to trust it
- really complex production
- aside - this guy has a hilariously dry sense of humour; lots of chuckles here: “if you want something mixed in moth cells and soap, well fine”
- trials: ongoing

Who’s at highest risk? Aside from the obvious (comorbidities, immunosuppressed) - it’s 🤰🏻women. We really need to make sure mums to be vaxxed.
Treatment - well this was a machine gun fire section so just gonna share the slides. ID guys love the replication phase so much.


Treatment - well this was a machine gun fire section so just gonna share the slides. ID guys love the replication phase so much.



Monoclonal antibodies are really effective for high risk patients not on O2, and also maybe for prophylaxis in early exposure. Also too molnupiravir (oral antiviral) and paxlovir. 





What about remdesivir? Need to be given it in the first few days of symptoms; which we currently don’t really have systematised.
Dexamethasone: goodness.
Budesonide? Probably
Fluvoxamine? We’ll see
We ran out of time on this one! Maybe questions later…Next: Dr Lauren Fielke!
Dexamethasone: goodness.
Budesonide? Probably
Fluvoxamine? We’ll see
We ran out of time on this one! Maybe questions later…Next: Dr Lauren Fielke!
Why is Gen Med running the #COVID19 unit at the RAH? It’s the home of the sick patient with a horizontal hierarchy & used to collaboration through a generalist lens!
Help!! How do I assess the exposure risk? #COVID19 risk for newbies table here:
Help!! How do I assess the exposure risk? #COVID19 risk for newbies table here:

High risk and low risk are easy - intermediate risk is the tricky middle.
What matters: keep asking questions as things evolve
What matters: keep asking questions as things evolve

Where in the hospital should these positive patients be?
- not always the ICU!
- ward based HFNO can help in Rx and also post exit at ion
- standard O2 is dry, coldness can ➡️bronchoconstriction; inconsistent FiO2

- not always the ICU!
- ward based HFNO can help in Rx and also post exit at ion
- standard O2 is dry, coldness can ➡️bronchoconstriction; inconsistent FiO2


What about awake proning?
- no mortality difference
- a difference in intubation rates
- 17% vs 48% impact for proning >8 hours per 24 hours
- early proning makes a difference to mortality
- some caveats around obesity and impending resp failure
- no mortality difference
- a difference in intubation rates
- 17% vs 48% impact for proning >8 hours per 24 hours
- early proning makes a difference to mortality
- some caveats around obesity and impending resp failure

Takeaways:
- O2: target SpO2 92-94
- steroids ✅
- awake proning ✅
- ? Remdesivir
- HFNO if proning not working
- ?CPAP next
- the first 24/48hrs are crucial
- O2: target SpO2 92-94
- steroids ✅
- awake proning ✅
- ? Remdesivir
- HFNO if proning not working
- ?CPAP next
- the first 24/48hrs are crucial
NOW it’s Dr Nick Edwards, intensivist & #COVID19 lead at the RAH.
So… who should come to ICU?
- O2 requirement >4L/min to maintain SpO2>92% or RR>30 should trigger a discussion
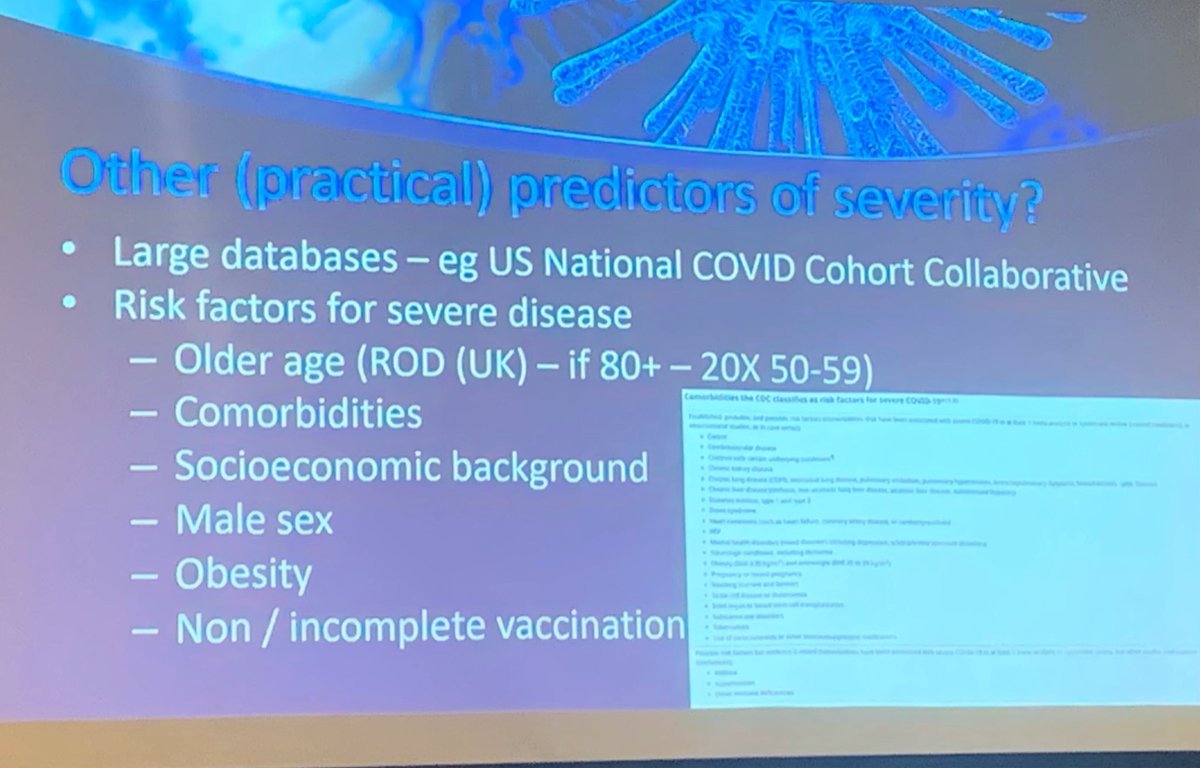
- So… what predicts severity?
So… who should come to ICU?
- O2 requirement >4L/min to maintain SpO2>92% or RR>30 should trigger a discussion
- So… what predicts severity?
Severity predicted by:
- factors below are population based
- what about bloods? Thresholds are not well established without good prognostic value
- what about clinical indicators: not too predictive.
- it really…. Comes down to clinical judgement

- factors below are population based
- what about bloods? Thresholds are not well established without good prognostic value
- what about clinical indicators: not too predictive.
- it really…. Comes down to clinical judgement

What are complications assoc with ⬆️mortality?
- hypercoagulability. How do we prevent it? Standard dose chemoprophylaxis - no evidence for ⬆️dose
- what about cardiac disease - what’s underlying vs what’s a complication? Myocarditis (mostly a clinical Dx), Takotsubo, arrhythmia

- hypercoagulability. How do we prevent it? Standard dose chemoprophylaxis - no evidence for ⬆️dose
- what about cardiac disease - what’s underlying vs what’s a complication? Myocarditis (mostly a clinical Dx), Takotsubo, arrhythmia


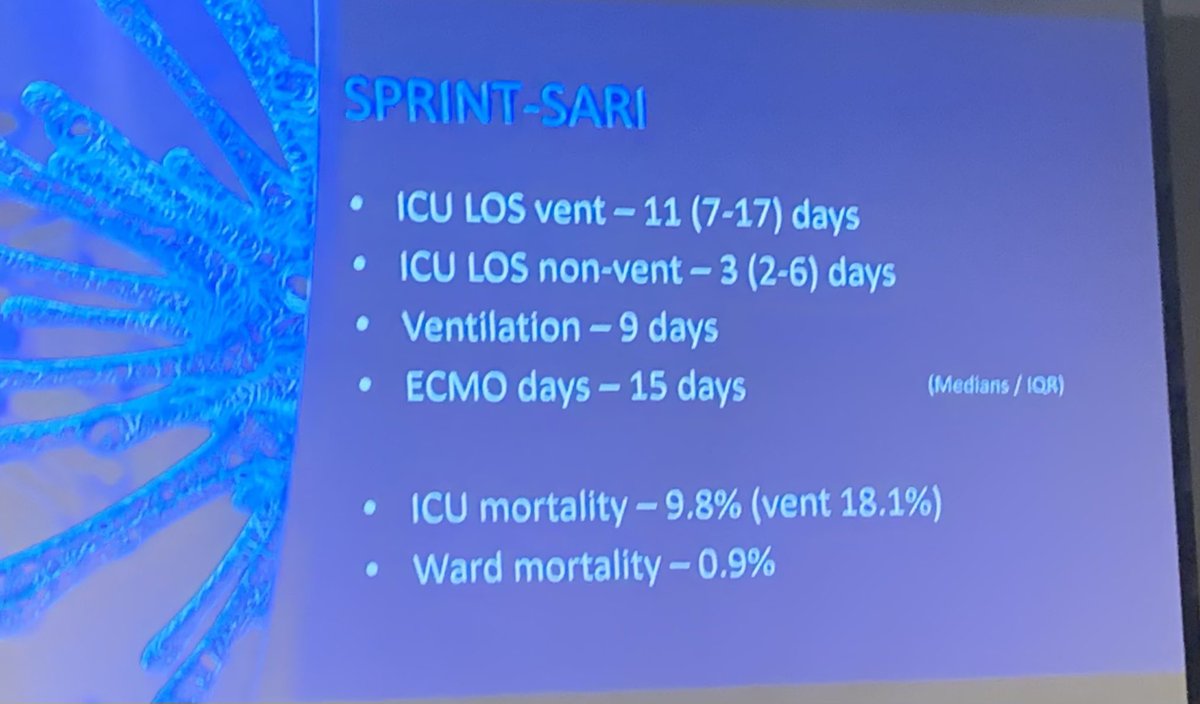
What do patients in ICU look like in Australia?
- 1827 patients so far
- median age 53
- triggers for ECMO are markedly varied, as are proning rates
- awake proning is the standard of care for FiO2>28% (}L/min) for >3hrs a day

- 1827 patients so far
- median age 53
- triggers for ECMO are markedly varied, as are proning rates
- awake proning is the standard of care for FiO2>28% (}L/min) for >3hrs a day

I got to ask a❓for our rural/remote patients!
- what about monoclonal antibodies for our high risk non-metro patients?
- sourced from the RAH
- 50 doses of monoclonal antibodies in SA right now…. Strategic placement of some in key regional centres for high risk is the goal.
- what about monoclonal antibodies for our high risk non-metro patients?
- sourced from the RAH
- 50 doses of monoclonal antibodies in SA right now…. Strategic placement of some in key regional centres for high risk is the goal.
Thanks so much to all of the outstanding speakers who really gave us a great sense of lessons learned, in our country, and a great sense of “we’re all in this together”. /END
• • •
Missing some Tweet in this thread? You can try to
force a refresh




