#Omicron is in #BC and provinces across #Canada, and it moves fast. Cases in #ON are doubling every 2-3 days. The need for #RapidTests is greater than ever. One key issue is how well the tests work for individuals and populations. So let’s talk about it. 🧵1/
In #PoPBC Briefing 3 on testing, @VicLeungIDdoc gave us the run down on rapid tests:
-Usually they are a shallow nose (not deep like a PCR test) or mouth swab
-You analyze at home
-Get the results in 15 minutes
/2
-Usually they are a shallow nose (not deep like a PCR test) or mouth swab
-You analyze at home
-Get the results in 15 minutes
/2

One of the big questions here, is how well do rapid antigen tests work? And the answer is really really well if you want to know if you are infectious and can transmit to someone else.
/3
/3
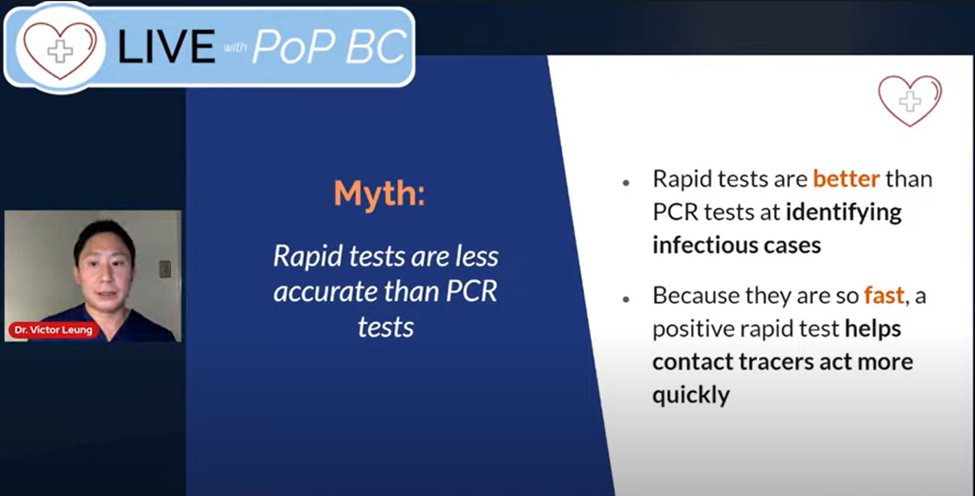
Rapid tests answer the question: can I give someone COVID?
Because you are not infectious for the whole time you have COVID, they cannot be used to diagnose COVID.
See this great chart from @michaelmina_lab
/4
Because you are not infectious for the whole time you have COVID, they cannot be used to diagnose COVID.
See this great chart from @michaelmina_lab
/4

Importantly, rapid tests don’t care if you have symptoms. They don't measure symptoms. They measure viral load. Your viral load can be high enough to transmit covid to someone else even if you don’t have symptoms. As @VicLeungIDdoc explains here:
/5
/5
They work well, but *how* well?
It varies by test but a good estimate is:
-If you *are* infectious, 90% of the time the RAT will correctly say you are infectious
-If you *are not* infectious, 99.5% of the time the RAT will correctly say you are not infectious
/6
It varies by test but a good estimate is:
-If you *are* infectious, 90% of the time the RAT will correctly say you are infectious
-If you *are not* infectious, 99.5% of the time the RAT will correctly say you are not infectious
/6

.@TallPupper walked #PoPBC through how to use rapid tests to make family gatherings safer.
“It’s well worthwhile to have that tiny risk of a false result if I’m cutting down the risk of the event [going to see my elderly mother while infectious] by such a large factor”
/7
“It’s well worthwhile to have that tiny risk of a false result if I’m cutting down the risk of the event [going to see my elderly mother while infectious] by such a large factor”
/7
So that’s how well tests work for you as an individual. But what about large groups or populations?
One thing you might hear come-up when people talk about #rapidtests and how useful they are is “pre-test probability” (PtP) also called “pre-test prevalence”.
/8
One thing you might hear come-up when people talk about #rapidtests and how useful they are is “pre-test probability” (PtP) also called “pre-test prevalence”.
/8

It’s important to know that PtP doesn’t change how well the test works for each person.
What it does change is the positive predictive value (PPV) and the negative predictive value (NPV) of a test. That is, how many people who test positive are truly positive and vice versa.
/9
What it does change is the positive predictive value (PPV) and the negative predictive value (NPV) of a test. That is, how many people who test positive are truly positive and vice versa.
/9

An easy way to see how PtP influences PPV is to imagine a scenario where everybody in our population had COVID (PtP = 100%).
If everybody had COVID, it would be impossible to get any false positives or true negatives. So, PPV = 100% and NPV = 0%
/10
If everybody had COVID, it would be impossible to get any false positives or true negatives. So, PPV = 100% and NPV = 0%
/10
Conversely, if nobody had COVID (PtP = 0%), then it would be impossible to get any true positives or false negatives. So PPV = 0% and NPV = 100%.
In these instances, the test is still exactly the same, but how much COVID is in the population has changed the PPV and the NPV.
/11
In these instances, the test is still exactly the same, but how much COVID is in the population has changed the PPV and the NPV.
/11
Luckily & unluckily, neither is true.
Let’s imagine PtP of infectiousness is 1%. We have 20,000 people to test (about 1 NHL game); 200 of them are infectious (PtP = 1%).
Using rapid tests, we would correctly identify 180 of the 200 infectious cases.
Risk⬇️90%!
PPV = 64.5%
/12
Let’s imagine PtP of infectiousness is 1%. We have 20,000 people to test (about 1 NHL game); 200 of them are infectious (PtP = 1%).
Using rapid tests, we would correctly identify 180 of the 200 infectious cases.
Risk⬇️90%!
PPV = 64.5%
/12

If we’re concerned about false positives and want a higher PPV, we could give a second test to the 279 people who tested positive.
This would correctly identify 162 people as infectious.
Risk ⬇️ 81%
PPV = 99%
/13
This would correctly identify 162 people as infectious.
Risk ⬇️ 81%
PPV = 99%
/13

But we know pre-test prevalence (PtP) impacts positive predict value (PVP). So let’s also look at 10% and 0.1%
We can see when PtP is low, PPV with one test is also low.
But, PPV improves a lot and risk is still reduced by giving 2 tests to each person who tests positive.
/14
We can see when PtP is low, PPV with one test is also low.
But, PPV improves a lot and risk is still reduced by giving 2 tests to each person who tests positive.
/14

So, what's the take home from all of that:
What matters to individuals using a rapid test for single events is different from what matters when using rapid tests in large groups.
PtP and PPV aren't super important for individuals using rapid tests to make holidays safer./15
What matters to individuals using a rapid test for single events is different from what matters when using rapid tests in large groups.
PtP and PPV aren't super important for individuals using rapid tests to make holidays safer./15
Overall, #rapidtests are a very valuable tool:
-Rapid tests are great at detecting if you are infectious
-They can reduce your risk of going somewhere when infectious by 90%
-For large groups, low PPV can be addressed with 2 tests (it only takes 15 more minutes!)
/end
-Rapid tests are great at detecting if you are infectious
-They can reduce your risk of going somewhere when infectious by 90%
-For large groups, low PPV can be addressed with 2 tests (it only takes 15 more minutes!)
/end
Addendum. This thread didn't address negative predictive value—the probability that a person who tests negative is negative—because often the discussion in BC has focused on PPV and false +s. @VicLeungIDdoc discusses NPV of rapid tests re infectiousness:
https://twitter.com/VicLeungIDdoc/status/1470899171360063489?t=z_wuTGSyt0EMi3cGkz7noA&s=19
• • •
Missing some Tweet in this thread? You can try to
force a refresh









