Unfortunately, there will likely be an H3N2 antigenic mismatch with the 2021-2022 Northern Hemisphere influenza vaccine. Our manuscript describing this has been posted on @medrxivpreprint. 1/10
medrxiv.org/content/10.110…
medrxiv.org/content/10.110…
Influenza viruses have circulated at low levels during the COVID-19 pandemic, and population immunity against these viruses is low. As COVID-19-related restrictions are eased or lifted, we expect wide circulation of influenza viruses. 2/10
In recent weeks, a unique H3N2 clade, 3C.2a1b.2a2 (herein 2a2), has circulated at elevated levels in the United States and other parts of the world. 3/10 

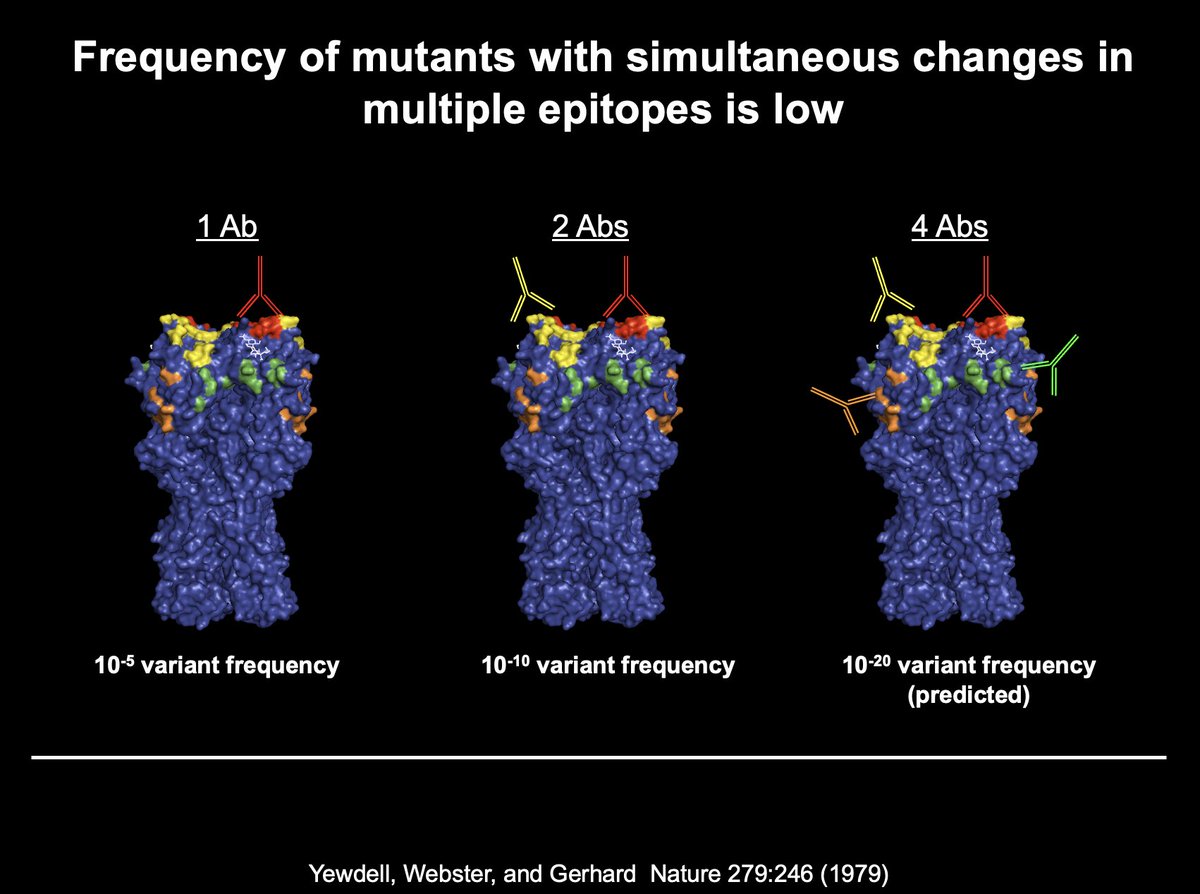
Viruses within this new clade have several substitutions in key antigenic sites on hemagglutinin (HA) relative to the 2021-2022 Northern Hemisphere H3N2 vaccine strain, a 3C.2a1b.2a1 (herein 2a1) virus. 4/10 

We found that one of these substitutions eliminates a key glycosylation site on HA. Although 2a2 viruses have a decrease in receptor specificity breadth, they replicate at least as efficiently as 2a1 H3N2 viruses in both primary and transformed cell culture systems. 5/10 

Importantly, we found that antibodies elicited by the 2021-2022 Northern Hemisphere influenza vaccine poorly neutralize the new 2a2 H3N2 clade. 55% of vaccinees had undetectable levels of neutralizing antibodies against 2a2 H3N2 after vaccination. 6/10 

Our data provide an antigenic explanation for low VE against 2a2 during a recent outbreak on a college campus. 7/10
cdc.gov/mmwr/volumes/7…
cdc.gov/mmwr/volumes/7…
Our study has some limitations. We only measured antibody responses in 40 individuals and most participants in our study were relatively young and healthy. 8/10
It is very important for everyone to receive this year's influenza vaccine. Studies have clearly shown that seasonal influenza vaccines consistently prevent hospitalizations and deaths even in years where there are large antigenic mismatches. 9/10
Influenza vaccinations will be crucial for reducing hospitalizations as SARS-CoV-2 and 2a2 H3N2 viruses co-circulate in the coming months. 10/10
This study involved a great collaborative effort with the labs of @jcpJim @andrewpekosz and was funded by @CEIRRNetwork.
• • •
Missing some Tweet in this thread? You can try to
force a refresh