
In Oct, the #USPSTF released draft guidelines addressing aspirin (ASA) use for the primary prevention of cardiovascular disease (CVD).
Why is ASA falling more out of favor? Join me for a #MedTwitter #Tweetorial about the hx of ASA use in *primary* prevention of CVD 1/20
Why is ASA falling more out of favor? Join me for a #MedTwitter #Tweetorial about the hx of ASA use in *primary* prevention of CVD 1/20
We'll answer a few questions on this journey:
1) What is new in the USPSTF draft update?
2) What trials informed the old practice patterns and guidelines?
3) What new trials have caused such a shift in how we think about ASA for the primary prevention of CVD?
2/20
1) What is new in the USPSTF draft update?
2) What trials informed the old practice patterns and guidelines?
3) What new trials have caused such a shift in how we think about ASA for the primary prevention of CVD?
2/20
First, what is in the USPSTF update?
ASA would now be recommended only after a shared-decision making conversation in those 40-59, at ⬆️risk of CVD (ASCVD risk >10%), at low risk for bleeding.
The recommendation grade is a "C", suggesting any net benefit is likely small. 3/20
ASA would now be recommended only after a shared-decision making conversation in those 40-59, at ⬆️risk of CVD (ASCVD risk >10%), at low risk for bleeding.
The recommendation grade is a "C", suggesting any net benefit is likely small. 3/20

So is this new?
Well since 2002, the USPSTF has more widely recommended ASA for the primary prevention of CVD.
More specifically, the recommendation has previously gotten an "A" or "B" rating (i.e. high certainty of at least moderate benefit). 4/20
Well since 2002, the USPSTF has more widely recommended ASA for the primary prevention of CVD.
More specifically, the recommendation has previously gotten an "A" or "B" rating (i.e. high certainty of at least moderate benefit). 4/20
Second, so why was ASA previously so beloved?
The modern hx of ASA began in the 1980s with the Physicians Health Study (PHS). In this study, docs were randomized to ASA vs placebo and followed.
Most notably, the PHS reported a 44% reduction in MI! 5/20
nejm.org/doi/full/10.10…
The modern hx of ASA began in the 1980s with the Physicians Health Study (PHS). In this study, docs were randomized to ASA vs placebo and followed.
Most notably, the PHS reported a 44% reduction in MI! 5/20
nejm.org/doi/full/10.10…
After the study was published, the @nytimes wrote an article with the headline "Doctors Confirm Benefits Of Aspirin"
....so if the benefit was confirmed, why have we kept studying ASA and its role in the primary prevention of CVD? 6/20
nytimes.com/1989/07/20/us/…
....so if the benefit was confirmed, why have we kept studying ASA and its role in the primary prevention of CVD? 6/20
nytimes.com/1989/07/20/us/…
Well, because another similar study conducted at the same time, the British Male Doctor (BMD) study, didn't show any benefit. Furthermore, neither the BMD nor PHS study showed any CV mortality benefit, and there was bleeding risk for those on ASA in both studies. 7/20 

The inconsistent results led to questions.
Were the same populations captured by both trials? Were events being classified the same way?
...Are all people who get CVD men...
Also, with time more folks were on statins and fewer smoked. Could this make ASA unnecessary? 8/20
Were the same populations captured by both trials? Were events being classified the same way?
...Are all people who get CVD men...
Also, with time more folks were on statins and fewer smoked. Could this make ASA unnecessary? 8/20
So from 1990-2014, eight major (but flawed) trials studied if ASA could prevent CVD.
Results showed ASA possibly⬇️CVD events (but not mortality) and definitely⬆️bleeds
Despite the trials' flaws, many docs recommended ASA due to positive secondary endpoints in the trials. 9/20
Results showed ASA possibly⬇️CVD events (but not mortality) and definitely⬆️bleeds
Despite the trials' flaws, many docs recommended ASA due to positive secondary endpoints in the trials. 9/20

Finally, this brings us to 2018, the golden year of ASA trials.
Three excellent trials were conducted 1) those at moderate risk of ASCVD (ARRIVE), 2) healthy older adults (ASPREE), 3) adults with diabetes (ASCEND).
Summary of the results below: 10/20
Three excellent trials were conducted 1) those at moderate risk of ASCVD (ARRIVE), 2) healthy older adults (ASPREE), 3) adults with diabetes (ASCEND).
Summary of the results below: 10/20

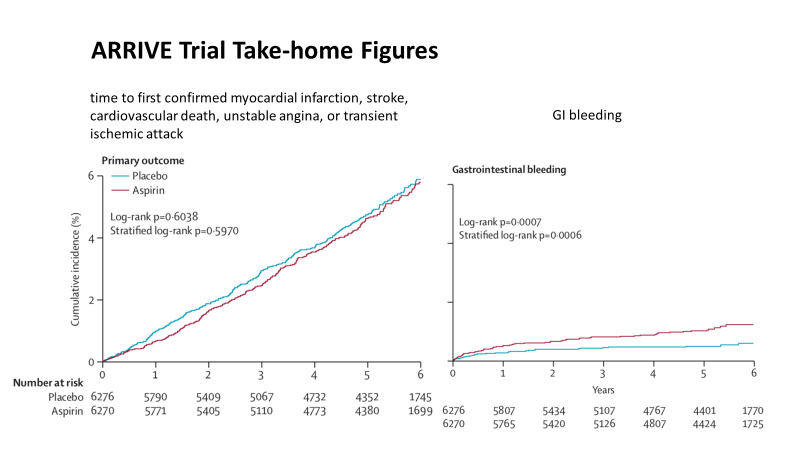
First, ARRIVE - ASA 100mg vs placebo did not reduce the risk of major CVD events, but did increase the risk of bleeding in patients. 11/20
thelancet.com/article/S0140-…
thelancet.com/article/S0140-…
Next, ASPREE - ASA 100mg vs placebo did not reduce the risk of major CVD events, but increased the risk of bleeding in healthy, older adults. 12/20
nejm.org/doi/full/10.10…
nejm.org/doi/full/10.10…

And ASCEND - ASA 100mg vs placebo reduced the risk of major CV events, but increased the risk of bleeding in patients with diabetes. 13/20
nejm.org/doi/full/10.10…
nejm.org/doi/full/10.10…

However, even in ASCEND, the only trial to meet its primary endpoint, only select patients clearly benefitted from ASA.
➡️Those under 60 had fewer CVD events and less bleeding risk (tying back to the USPSTF guideline age cutoff). 14/20
➡️Those under 60 had fewer CVD events and less bleeding risk (tying back to the USPSTF guideline age cutoff). 14/20

So where are we?
13 major trials looking at ASA for the primary prevention of CVD.
2 old trials w/o women and before the statin era showing mixed results.
8 more contemporary flawed trials showing mixed results
3 new well-done trials suggesting minimal net benefit 14/20
13 major trials looking at ASA for the primary prevention of CVD.
2 old trials w/o women and before the statin era showing mixed results.
8 more contemporary flawed trials showing mixed results
3 new well-done trials suggesting minimal net benefit 14/20
And so since that first trial was published in 1988:
-ASA has inconsistently shown benefit for CVD prevention depending on the population and study.
-ASA has consistent shown harm via ⬆️bleeding risk. 15/20
-ASA has inconsistently shown benefit for CVD prevention depending on the population and study.
-ASA has consistent shown harm via ⬆️bleeding risk. 15/20
Ultimately meta-analyses results are in:
-11% (95% CI 6-15%) ⬇️in odds of CVD Mortality, Nonfatal Stroke, or Nonfatal MI
-No significant association with CVD or all-cause mortality
-45% (95% CI 33-58%) ⬆️in odds of major bleeds
16/20
uspreventiveservicestaskforce.org/uspstf/documen…



-11% (95% CI 6-15%) ⬇️in odds of CVD Mortality, Nonfatal Stroke, or Nonfatal MI
-No significant association with CVD or all-cause mortality
-45% (95% CI 33-58%) ⬆️in odds of major bleeds
16/20
uspreventiveservicestaskforce.org/uspstf/documen…




The case for ASA was never particularly strong before the 2018 trials, so why was ASA use so seared into the public consciousness?
Partly inconsistent trial results, but partly because companies like Bayer used media to propagate its use.
17/20
ncbi.nlm.nih.gov/pmc/articles/P…
Partly inconsistent trial results, but partly because companies like Bayer used media to propagate its use.
17/20
ncbi.nlm.nih.gov/pmc/articles/P…
So now you know how we got to the place where we can say:
ASA may have benefit in primary prevention of CVD for some patients <60 with⬆️CVD risk and ⬇️bleed risk.
But the benefit is likely small, the risks are real, and there is likely no mortality benefit. 18/20
ASA may have benefit in primary prevention of CVD for some patients <60 with⬆️CVD risk and ⬇️bleed risk.
But the benefit is likely small, the risks are real, and there is likely no mortality benefit. 18/20
Hope this contextualization of the evidence for ASA in primary prevention of CVD was helpful! To learn more, this is a great paper.
Of course, this is ONLY for PRIMARY prevention. 19/20
thelancet.com/journals/lance…
Of course, this is ONLY for PRIMARY prevention. 19/20
thelancet.com/journals/lance…
Thanks anybody who reads this for joining!
Perhaps interesting to @BrighamMedRes @tony_breu @kkidia @WalkerReddMD @Sophia_Hayes_MD @reverendofdoubt @AlexanderZheut1 @AdamRodmanMD @adamcifu @mikejohansenmd @SalamBachour 20/20
Perhaps interesting to @BrighamMedRes @tony_breu @kkidia @WalkerReddMD @Sophia_Hayes_MD @reverendofdoubt @AlexanderZheut1 @AdamRodmanMD @adamcifu @mikejohansenmd @SalamBachour 20/20
• • •
Missing some Tweet in this thread? You can try to
force a refresh



