
1/Briefs were filed for the Supreme Court today, on whether doctors will continue to be criminally convicted under the Controlled Substances Act when Rx’s were offered in good faith.
Our team’s work was cited in the @national_pain amicus whose thread covers the law.
My 🧵:
Our team’s work was cited in the @national_pain amicus whose thread covers the law.
My 🧵:
https://twitter.com/national_pain/status/1475507669502939139
2/The use of criminal charges and prison as a method of regulating US opioid prescribing is a U.S.-specific phenomenon.
It reflects the legacy of the Harrison Narcotics Tax Act (1914) and the Controlled Substances Act (1971).
It is a choice we made that other countries didn’t
It reflects the legacy of the Harrison Narcotics Tax Act (1914) and the Controlled Substances Act (1971).
It is a choice we made that other countries didn’t
3/as opioid overdoses rose, Department of Justice announced its intention to use “data tools” to drive prosecutions, ie investigate higher prescribers - justice.gov/opa/pr/attorne…
4/The DoJ & DEA rely partly on Rx records for each state & profiles prepared for them from the Office of Inspector General of @HHSGov - this is suggested by OIG reports. My collaborators & I noted that in a piece for @JournalGIM in 2020 @AllysonVarley link.springer.com/article/10.100… 

5/I increasingly hear from doctors subject to criminal investigation, by DEA, predicated on just a few patients’ care, patients who presented genuine clinical decision-making challenges, and where there is not even a shadow of intent to “distribute” - not pill mills
6/US Attorneys Offices have announced their own letters of warning to physicians based only on statistical profiling of prescriptions relative to peers - the “warning” here is from a criminal justice agency. The obvious implication is the risk of prison. link.springer.com/article/10.100… 

7/For anyone who has recently watched @DopesickOnHulu, or read @EricEyre and resonated with the absolute chaos it depicts, this could sound reasonable .. but it is not. For three reasons that bear on the safety and care of our patients right now
8/First, we are not sitting in 2012: US opioid prescribing per capita now sits at the level of 1992, pre-Oxycontin 

9/Second, the fear of caring for patients who need opioids or happen to be on them, has resulted in a US crisis of abandonment and refusal to care for patients with pain.
The research data is real but so too are the myriad patient stories that I receive pubmed.ncbi.nlm.nih.gov/33230009/
The research data is real but so too are the myriad patient stories that I receive pubmed.ncbi.nlm.nih.gov/33230009/
10/Third, and this gets back to the core question before the Supreme Court. The historic legal standard of prosecution for a crime normally requires “mens rea” , is intent to commit a crime. The exception to that, in some federal districts (but not others) is prescribing doctors
11/the central legal matter is whether jury instructions can allow a doctor to be found guilty of criminal drug distribution because their opioid prescribing diverted from the views of DEA’s paid physician experts, even if the decision was carefully made, with good intentions
12/The underlying matter is how the expression “good faith” (a term used in the Controlled Substances Act) can be interpreted when juries are given instructions prior to their deliberation on whether to convict a doctor.
This matters for the safety and protection of patients
This matters for the safety and protection of patients
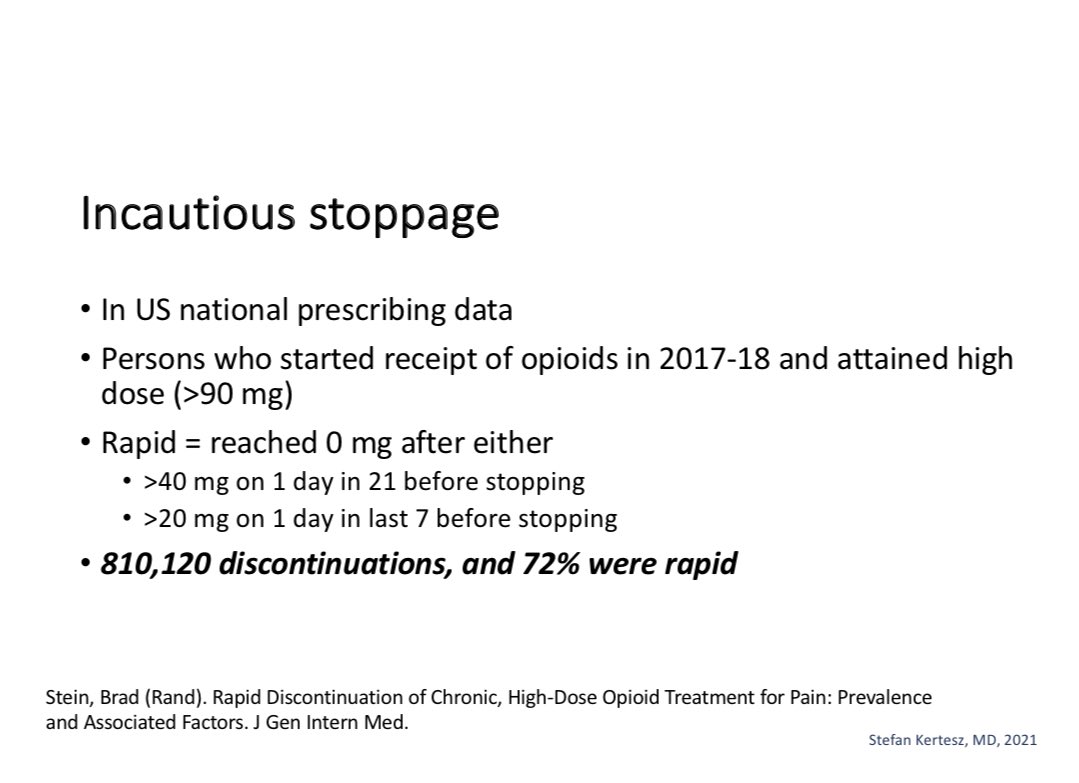
13/Today, physicians are under inducement from quality regulators, and from legal authorities, to refuse to continue opioids, to stop them even when needed, to stop suddenly, and to ignore actual harms that follow, which the regulators and law enforcement also ignore 




14/There is no point in medical training where we’re told “it is okay to harm patients or cause deaths; no one will be watching”
But we’ve arrived at a historic moment where that has become a de facto reality, tolerated partly because of a reckoning with past excess prescribing
But we’ve arrived at a historic moment where that has become a de facto reality, tolerated partly because of a reckoning with past excess prescribing
15/The threat of prosecution of doctors lacking criminal intent is just one part of a very difficult historic moment in a US opioid story.But an important part. I salute the parties who filed Amici @RonChapmanAtty @dineenkk - and proud our article helped with @national_pain /fin
• • •
Missing some Tweet in this thread? You can try to
force a refresh










