
COVID-19: Rapid test sensitivity with Omicron and where to swab
A couple of studies on the sensitivity of rapid tests with Omicron have recently been released. The first is a pre-print that evaluated 7 rapid tests ( medrxiv.org/content/10.110… ). 🧵1/ FYI @SabiVM,@imgrund,@DFisman
A couple of studies on the sensitivity of rapid tests with Omicron have recently been released. The first is a pre-print that evaluated 7 rapid tests ( medrxiv.org/content/10.110… ). 🧵1/ FYI @SabiVM,@imgrund,@DFisman
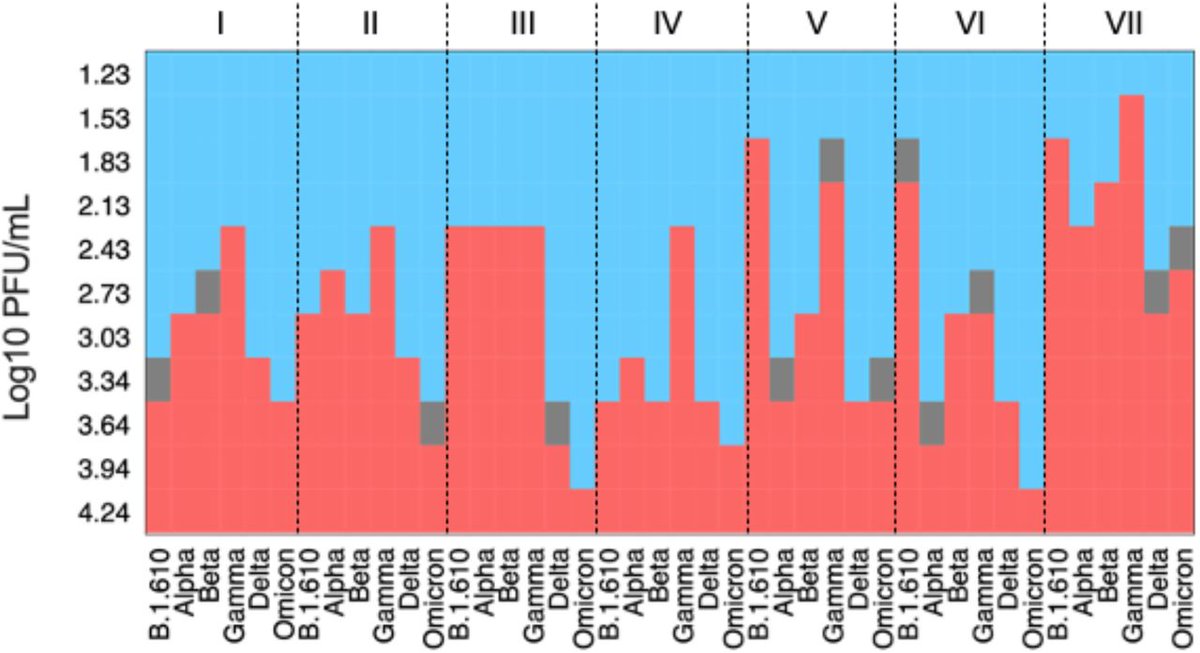
They found that detection of Omicron is the first variant of concern (VOC) that showed a tendency towards lower analytical sensitivity across tests. They found a considerable difference in sensitivity patterns between tests across variants including Omicron. 2/
The differences in analytical sensitivity between rapid tests might be explained by the different epitopes each test is looking for in the virus and potentially impacted differently from mutations in the nucleocapsid protein that most tests use (not the spike). 3/
If lower sensitivity is confirmed in clinical validations, that means rapid tests in the early stages of an Omicron infection when viral load is lower could be less reliable. 4/
You can see from the first graph that the Flowflex (ACON Biotech) rapid test listed as VII in the table was able to detect Omicron with a lower viral load than all the others. 5/ 
The rapid tests were:
I = Panbio COVID-19 Ag Rapid test device (Abbott)
II = Standard Q COVID-19 Ag (SD Biosensor/Roche)
III = Sure Status (Premier Medical Corporation)
IV = 2019-nCoV Antigen test (Wondfo)
6/
I = Panbio COVID-19 Ag Rapid test device (Abbott)
II = Standard Q COVID-19 Ag (SD Biosensor/Roche)
III = Sure Status (Premier Medical Corporation)
IV = 2019-nCoV Antigen test (Wondfo)
6/
V = Beijng Tigsun Diagnostics Co. Ltd (Tigsun)
VI = Onsite COVID-19 Ag Rapid Test (CTK Biotech)
VII = Flowflex (ACON Biotech)
7/
VI = Onsite COVID-19 Ag Rapid Test (CTK Biotech)
VII = Flowflex (ACON Biotech)
7/
A couple of the tests (III and VI) require a much higher viral load to detect Omicron than some of the others. One box height in the graph means double the amount of virus is required for detection which equals around one additional PCR cycle count (
https://twitter.com/RolandSB13/status/1474096812885745675).8/
Viral load doubling times with previous variants (D614G) was about 2.4 hours while Delta is much faster at 1.2-1.6 hours. 9/
If Omicron is similar that means in practical terms some of the rapid tests may need someone to be infected 2-4 hours longer for the viral load to be high enough to be detected compared with Delta. 10/
Dr. Mina believes these results may show that all tests will have slightly lower sensitivity, PCR included (
https://twitter.com/michaelmina_lab/status/1474473813349912576). A more aggressive, more efficient ability to infect a cell and take hold would appear in a study like this as lower sensitivity. 11/
That means someone could potentially get a negative test result when they are slightly contagious. This is another reason why rapid tests the night or day before are not a good indicator for your status now. 12/
Another study looked at the analytical sensitivity of 10 rapid tests with the Omicron variant ( journals.asm.org/doi/10.1128/jc… ). 13/
They found less of a difference between test results for Delta and Omicron than the study above. All 10 kits were able to detect Delta at 6.5 log10 copies/mL (PCR Ct 25.4) and Omicron at 6.39 log10 copies/mL (PCR Ct 25.8). 12/
None of the test kits detected Omicron at the lowest dilution 5.33 log10 copies/mL (PCR Ct 28.8). 13/
The rapid tests were:
1 = Panbio COVID-19 (Abbott)
2 = NowCheck COVID-19 (BioNote Inc )
3 = Roche SARS-CoV-2 (SD Biosensor Inc)
4 = STANDARD Q (SD Biosensor Inc)
5 = Surescreen Diagnostics (BTNX Inc )
6 = VivaDiag (VivaChek Biotech)
14/
1 = Panbio COVID-19 (Abbott)
2 = NowCheck COVID-19 (BioNote Inc )
3 = Roche SARS-CoV-2 (SD Biosensor Inc)
4 = STANDARD Q (SD Biosensor Inc)
5 = Surescreen Diagnostics (BTNX Inc )
6 = VivaDiag (VivaChek Biotech)
14/

7 = Wantai (Beijing Wantai Biologicalpharmacy)
8 = Testsea (Hangzhou Testsea Biotechnology)
9 = InnoScreen (Innovation Scientific)
10 =LYHER (Hangzhou Laihe Biotech)
15/
8 = Testsea (Hangzhou Testsea Biotechnology)
9 = InnoScreen (Innovation Scientific)
10 =LYHER (Hangzhou Laihe Biotech)
15/
The tests with best sensitivity to Omicron are:
- Panbio (Abbott)
- Surescreen (BTNX)
- VivaDiag (VivaCheck Biotech)
Abbott and BTNX rapid tests are available in Canada but stock is limited. 16/
- Panbio (Abbott)
- Surescreen (BTNX)
- VivaDiag (VivaCheck Biotech)
Abbott and BTNX rapid tests are available in Canada but stock is limited. 16/
Where is the best place to swab for Omicron? A pre-print study looked at shallow nose (mid-turbinate) and throat (saliva) swabs for both Delta and Omicron to see which ones tested positive the most ( medrxiv.org/content/10.110… ). 17/
For Delta they found that shallow nose swabs tested positive 100% of the time in their tests while throat/saliva swabs only tested positive 71% of the time when compared with PCR tests. 18/
This completely flips with Omicron and 86% of shallow nose swabs tested positive while 100% of throat/saliva swabs tested positive. 19/
It is actually possible to get the best of both worlds by swabbing the throat first and then the nose. Here is a video showing the process ( ). 20/
Another example where a combine swab provides much better results ( 
https://twitter.com/VicLeungIDdoc/status/1477156006798905346). Viral loads seems much higher in throat/mouth. 21/

• • •
Missing some Tweet in this thread? You can try to
force a refresh






