1/ There’s a lot of AEDs that work great together to tx szs! Unfortunately, Valproic acid (VPA) and Phenytoin (PHT) are two that didn’t get that memo.
Get ready for a fun and educational two-part #tweetorial on the do not miss VPA and PHT interactions w/ @theABofPharmaC
Get ready for a fun and educational two-part #tweetorial on the do not miss VPA and PHT interactions w/ @theABofPharmaC
2/ Let’s go back in time.
Valproic acid was first synthesized in 1882 by Burton. It wasn’t until 1963 when its anticonvulsant properties were discovered by Eymard.
Phenytoin was first synthesized in 1908 by Biltz and discovered to have anticonvulsant properties in 1936
Valproic acid was first synthesized in 1882 by Burton. It wasn’t until 1963 when its anticonvulsant properties were discovered by Eymard.
Phenytoin was first synthesized in 1908 by Biltz and discovered to have anticonvulsant properties in 1936
3/ VPA works by ⬆️ GABA lvls and blocking Na and Ca channels. It’s broad-spectrum permits its use for various szs types: partial, tonic clonic, myoclonic, and absence.
PHT works solely by inhibiting Na channels and has a narrower spectrum of use: partial and tonic clonic szs
PHT works solely by inhibiting Na channels and has a narrower spectrum of use: partial and tonic clonic szs
4/ The typical starting dose of VPA is 10-15 mg/kg/day w/ therapeutic range of 50-100 mcg/ml (total) and 5-15 mcg/ml (free). Roughly 10% of the total level = free level.
Adverse rx include hepatotoxicity, hyperammonemia, thrombocytopenia, pancreatitis, and fetal toxicity.
Adverse rx include hepatotoxicity, hyperammonemia, thrombocytopenia, pancreatitis, and fetal toxicity.
5/ The typical starting dose for Phenytoin PO is 100mg TID (remember to hold tube feeds 1 hr before and after).
If given IV (should really consider fosphenytoin instead), the starting bolus is 15-20mg/kg w/ therapeutic range of 10-20 mcg/ml (total) and 1.0-2.5 mcg/ml (free).
If given IV (should really consider fosphenytoin instead), the starting bolus is 15-20mg/kg w/ therapeutic range of 10-20 mcg/ml (total) and 1.0-2.5 mcg/ml (free).
6/ Adverse rx include gingival hyperplasia, ataxia, peripheral neuropathy, hepatotoxicity, and bone marrow suppression. If given IV purple glove syndrome, hypotension and arrhythmia can occur if given too rapidly.
7/ So what’s the big issue using the two together? VPA and PHT are both are highly protein bound to albumin meaning that they both compete for the same “hang out” spot.
VPA is bound to albumin at 90-95% whereas PHT is bound ~90%
VPA is bound to albumin at 90-95% whereas PHT is bound ~90%
8/ VPA displaces PHT from plasma binding sites, which significantly increases the free phenytoin level (i.e. the actual active form) even though the total level may still be the same or even decreased!
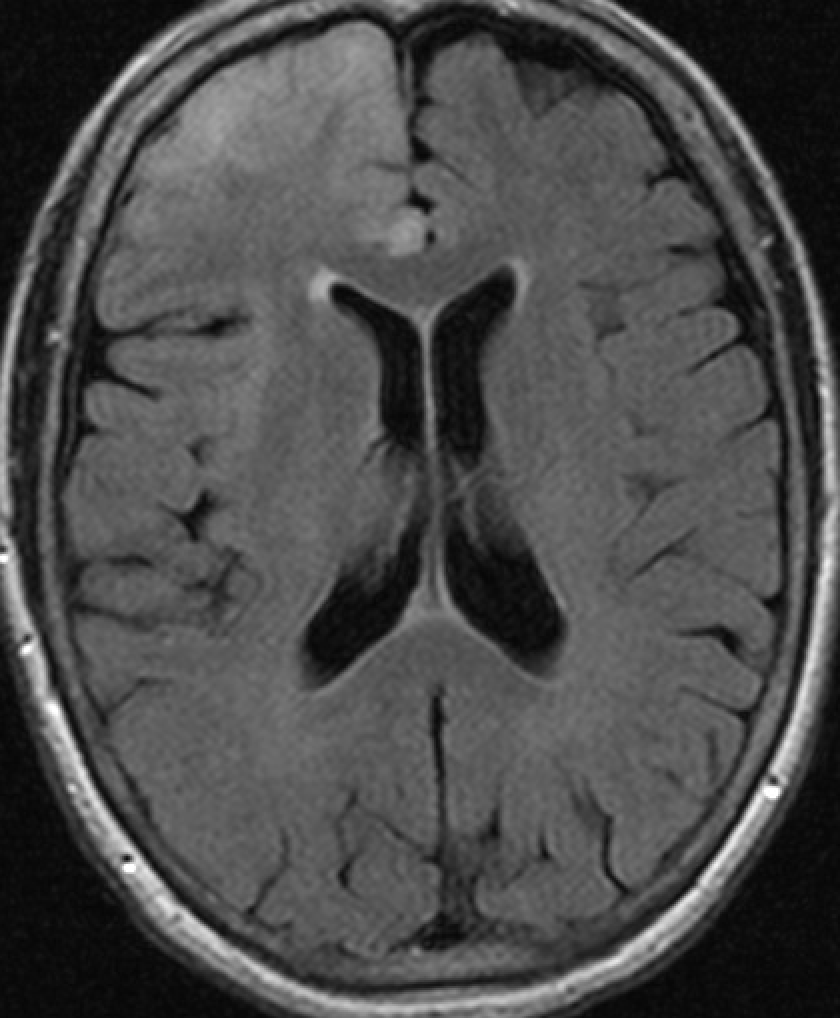
9/ What makes this even more complicated is the fact that Phenytoin follows zero-order kinetics.
.
.
.
Wait say what?
Unlike first-order kinetics where elimination is dependent on a constant % of a drug, zero-order kinetics is where elimination is the same constant amount.
.
.
.
Wait say what?
Unlike first-order kinetics where elimination is dependent on a constant % of a drug, zero-order kinetics is where elimination is the same constant amount.

10/ This means that after a certain threshold, even small ⬆️ in dosage can cause a significant disproportional ⬆️ in plasma concentration.
This is particularly important in patients with hypoalbuminemia or conditions that cause altered albumin binding (ex: acidosis/uremia).
This is particularly important in patients with hypoalbuminemia or conditions that cause altered albumin binding (ex: acidosis/uremia).

11/ If that wasn’t complicated enough, clinically significant % alterations of free VPA occurs when total drug concentrations become >80mcg/mL, making the VPA – PHT drug-drug interaction even more complex.
pubmed.ncbi.nlm.nih.gov/121944/
pubmed.ncbi.nlm.nih.gov/121944/
12/ If this is making your head hurt 🤯, thank all the wonderful and spectacular pharmacists who help keep an eye out on all these drug-drug interactions!
13/ So protein binding and zero order kinetics both play a big role when it comes to using both VPA and PHT together, but there’s more vital concepts to consider!
Head over to @theABofPharmaC to continue to part two of this tweetorial!
Head over to @theABofPharmaC to continue to part two of this tweetorial!
14/ Any other thoughts or pearls of wisdom? #EmoryNCCTweetorials #Neurotwitter
@mallyaa @sigman_md @EricLawson90 @JayKinariwala @maness_caroline @caseyalbin @Capt_Ammonia @DeniseFChen @Raf_Perz @drhibahaider @RebeccaFasanoMD @e_gleich @Tracey1milligan @NeyensRon @rkchoi
@mallyaa @sigman_md @EricLawson90 @JayKinariwala @maness_caroline @caseyalbin @Capt_Ammonia @DeniseFChen @Raf_Perz @drhibahaider @RebeccaFasanoMD @e_gleich @Tracey1milligan @NeyensRon @rkchoi
• • •
Missing some Tweet in this thread? You can try to
force a refresh