I am a generalist,
full-service family doctor,
working in a clinic
that provides
longitudinal primary care,
and I referred
a few patients
to specialists
this week...
here's how and why that happens 🧵 1/9
(#BCPrimaryCare)
full-service family doctor,
working in a clinic
that provides
longitudinal primary care,
and I referred
a few patients
to specialists
this week...
here's how and why that happens 🧵 1/9
(#BCPrimaryCare)
When I see a patient, we talk about:
-the reason they needed the appointment today
-how life is going in general
-as needed, their other medical history
after I get hear the story
do a physical exam
review old information
We may decide that we need extra advice
2/9
-the reason they needed the appointment today
-how life is going in general
-as needed, their other medical history
after I get hear the story
do a physical exam
review old information
We may decide that we need extra advice
2/9
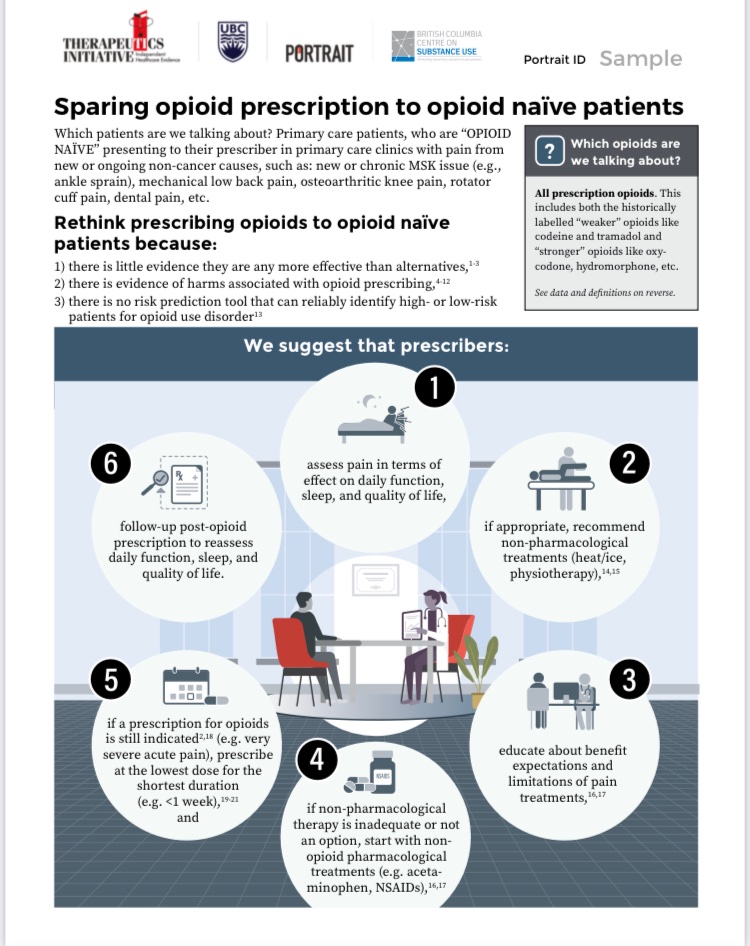
Sometimes it is:
to confirm the diagnosis or
change treatment or
decide on tests or imaging
consider surgery
etc
I need to formulate a specific question & summarize the patient's condition, history and preferences. I do this both on the fly & after the appointment. 3/9
to confirm the diagnosis or
change treatment or
decide on tests or imaging
consider surgery
etc
I need to formulate a specific question & summarize the patient's condition, history and preferences. I do this both on the fly & after the appointment. 3/9
I have a few choices about how to get that advice:
✅other MDs/NPs (I work w 16 VERY smart clinicians- our collective wisdom is 🤯)
✅The BC-specific RACE line raceconnect.ca where a specialist will call me back wi 2 hours
✅read an article
✅refer to a specialist
4/9
✅other MDs/NPs (I work w 16 VERY smart clinicians- our collective wisdom is 🤯)
✅The BC-specific RACE line raceconnect.ca where a specialist will call me back wi 2 hours
✅read an article
✅refer to a specialist
4/9
I add a note to the patient chart about what my decision is & any new information I have.
If I'm referring to a specialist, I usually need to pick a SPECIFIC person (sometimes I can refer to a "pooled service")
I use another great BC-specific tool:
5/9
pathwaysbc.ca
If I'm referring to a specialist, I usually need to pick a SPECIFIC person (sometimes I can refer to a "pooled service")
I use another great BC-specific tool:
5/9
pathwaysbc.ca
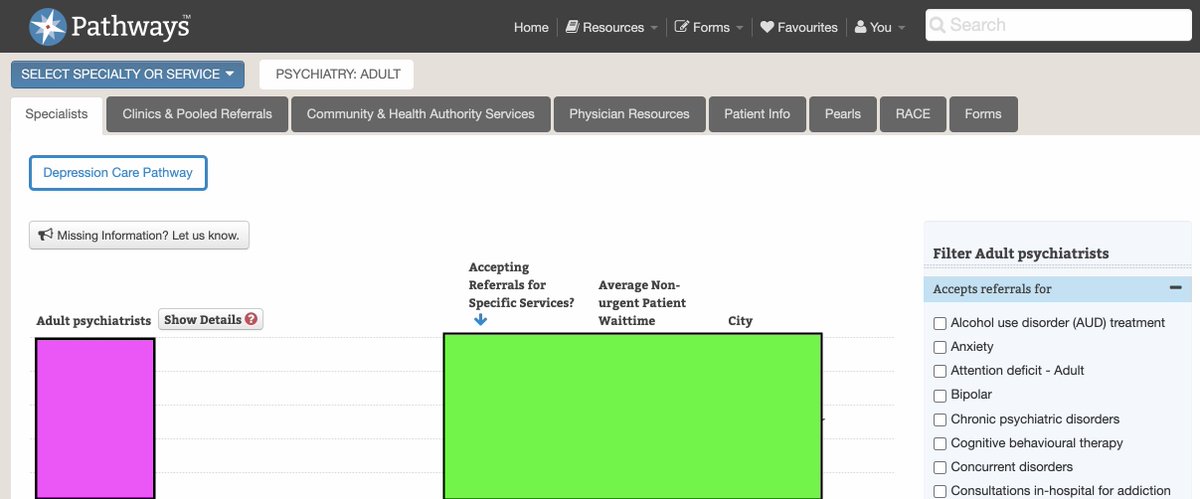
On Pathways I can see who is accepting referrals and how long the wait typically is, and then I need to write a referral letter.
Our EMR has a template & I can
copy lab results
lists of meds etc
pretty easily
but the letter usually takes 5-20 min
AFTER the appt time.
6/9
Our EMR has a template & I can
copy lab results
lists of meds etc
pretty easily
but the letter usually takes 5-20 min
AFTER the appt time.
6/9
Then I "submit" the letter
And our amazing admin staff
FAXES the letter
to the specialist's office
Sometimes the specialist acknowledges the referral, sometimes not
Usually, the specialist office advises the patient of the appointment date, but sometimes they ask us to 👀
7/9
And our amazing admin staff
FAXES the letter
to the specialist's office
Sometimes the specialist acknowledges the referral, sometimes not
Usually, the specialist office advises the patient of the appointment date, but sometimes they ask us to 👀
7/9
Once the patient sees the specialist, I get a letter back (faxed, or through a system called "excelleris") and my EMR notifies me it is there.
I read it & plan about how to react to it, & I document that in the chart
If it makes sense-I review w the patient at a new appt.
8/9
I read it & plan about how to react to it, & I document that in the chart
If it makes sense-I review w the patient at a new appt.
8/9
Primary care as the "gatekeeper" to specialist care is a key part of our 🇨🇦 system.
Interestingly, research shows that the more contact patients have w primary care (versus specialists) the LONGER they live & more equitable health is in a population
9/9
ncbi.nlm.nih.gov/pmc/articles/P…
Interestingly, research shows that the more contact patients have w primary care (versus specialists) the LONGER they live & more equitable health is in a population
9/9
ncbi.nlm.nih.gov/pmc/articles/P…
ADDENDUM 💰
1) in the current fee for service system, the only payment for this referral work is the patient visit ~32$, no matter how long writing/managing/responding takes
2) in a salaried or sessionally paid role, this work is acknowledged … as part of the work.
1) in the current fee for service system, the only payment for this referral work is the patient visit ~32$, no matter how long writing/managing/responding takes
2) in a salaried or sessionally paid role, this work is acknowledged … as part of the work.
@threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh