1.
Multiple tweet thread #tweetorial on pathologic abnormalities in the lung caused by cigarette smoking
Smoking causes a wide variety of pathologic changes in the lung, not just lung cancer. Some of these are underrecognized or poorly named
#smokinglungpath #pulmpath


Multiple tweet thread #tweetorial on pathologic abnormalities in the lung caused by cigarette smoking
Smoking causes a wide variety of pathologic changes in the lung, not just lung cancer. Some of these are underrecognized or poorly named
#smokinglungpath #pulmpath



2.
These smoking-related abnormalities include:
💥 Emphysema
💥 Pigmented airspace macrophages
💥 Ropy interstitial fibrosis (SRIF)
💥 Pulmonary Langerhans cell histiocytosis
Overlap is common because these abnormalities commonly occur together.
These smoking-related abnormalities include:
💥 Emphysema
💥 Pigmented airspace macrophages
💥 Ropy interstitial fibrosis (SRIF)
💥 Pulmonary Langerhans cell histiocytosis
Overlap is common because these abnormalities commonly occur together.
3.
Every week I will add my thoughts to this #pathtweetorial . I feel strongly about this topic because I see SO much smoking-related lung pathology that is misinterpreted and underrecognized. Not just SRIF (👇🏾) but also pigmented macrophages, commonly dismissed as “anthracotic”
Every week I will add my thoughts to this #pathtweetorial . I feel strongly about this topic because I see SO much smoking-related lung pathology that is misinterpreted and underrecognized. Not just SRIF (👇🏾) but also pigmented macrophages, commonly dismissed as “anthracotic”

4.
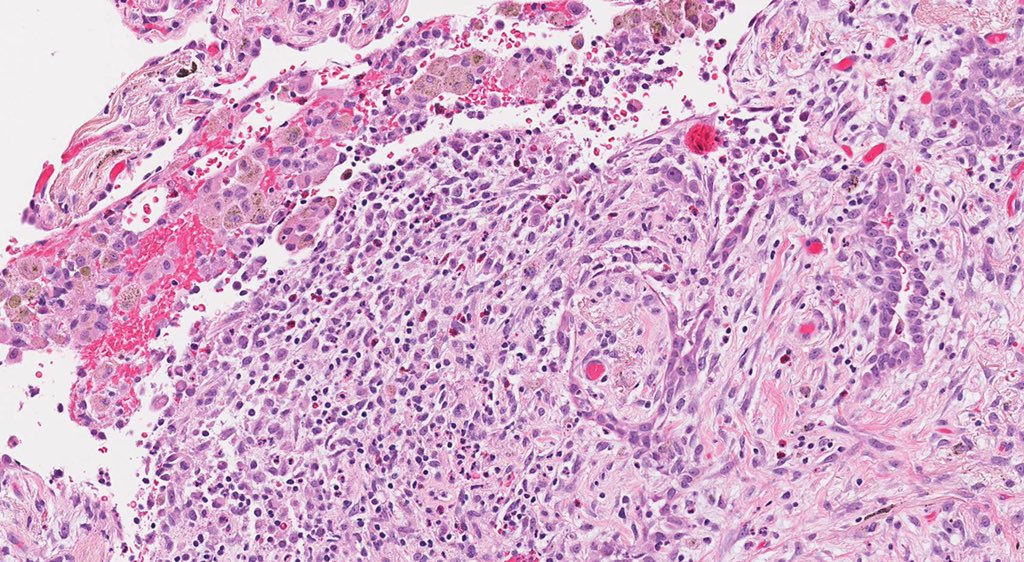
Let us start with pigmented macrophages. These are extremely common in the airspaces (alveolar lumens) of current and ex-smokers. Known since 1974 when Niewohner et al described them in @NEJM (PMID 4414994) in the lungs of young smokers.
Let us start with pigmented macrophages. These are extremely common in the airspaces (alveolar lumens) of current and ex-smokers. Known since 1974 when Niewohner et al described them in @NEJM (PMID 4414994) in the lungs of young smokers.

5.
This paper is the origin of the problematic term “respiratory bronchiolitis”. Why problematic? These cells are neither limited to bronchioles nor a true “itis”.
In reality, you will most commonly see these pigmented macrophages within alveoli.
nejm.org/doi/full/10.10…
This paper is the origin of the problematic term “respiratory bronchiolitis”. Why problematic? These cells are neither limited to bronchioles nor a true “itis”.
In reality, you will most commonly see these pigmented macrophages within alveoli.
nejm.org/doi/full/10.10…
6.
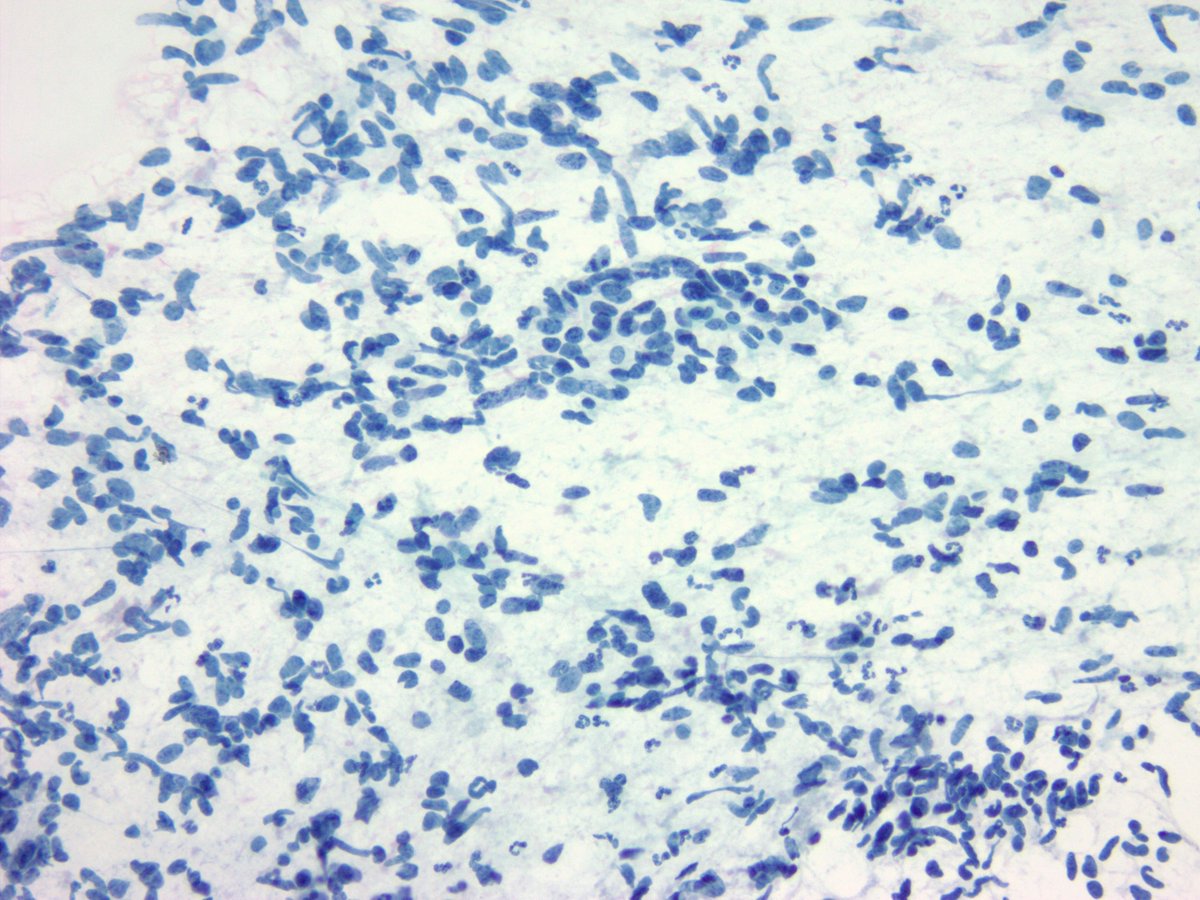
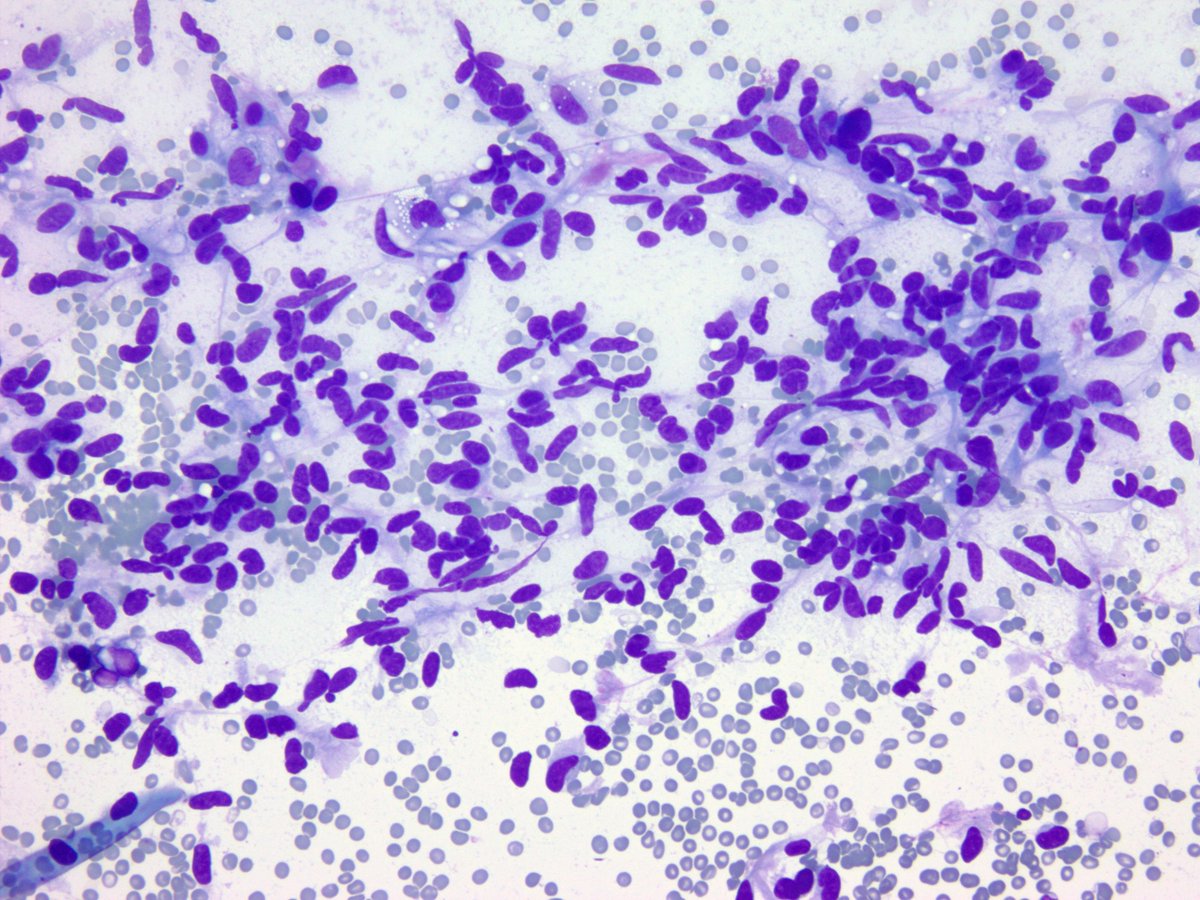
Look at these pics. Are these cells in bronchioles or alveoli?
Such a common smoking-related finding, yet we either use the wrong location (RB) or misrepresent the etiology by implying it’s related to coal (anthracotic). Why? Because we don’t have a better term.

Look at these pics. Are these cells in bronchioles or alveoli?
Such a common smoking-related finding, yet we either use the wrong location (RB) or misrepresent the etiology by implying it’s related to coal (anthracotic). Why? Because we don’t have a better term.


7.
I used to label them as RB but have started calling them what they are: pigmented airspace macrophages.
If I see them in a known smoker and I’m sure the pigment is not hemosiderin, I say: pigmented airspace macrophages, smoking-related
pubmed.ncbi.nlm.nih.gov/32843423/
I used to label them as RB but have started calling them what they are: pigmented airspace macrophages.
If I see them in a known smoker and I’m sure the pigment is not hemosiderin, I say: pigmented airspace macrophages, smoking-related
pubmed.ncbi.nlm.nih.gov/32843423/
8.
I do not mean to disparage the Niewohner paper by pointing out that respiratory bronchiolitis was not the best term.
The paper is a landmark in our understanding of the histologic changes that smoking causes in the lungs before emphysema develops.
Key cells: macrophages
I do not mean to disparage the Niewohner paper by pointing out that respiratory bronchiolitis was not the best term.
The paper is a landmark in our understanding of the histologic changes that smoking causes in the lungs before emphysema develops.
Key cells: macrophages

9.
Correction: PMID is 4414996. Interestingly, this highly cited study was done at Case Western Reserve Univ, just a few minutes’ walk from where I am right now.
Others (Pratt 1969, Harris 1970) had previously noticed increased macrophages in BAL specimens from smokers.
Correction: PMID is 4414996. Interestingly, this highly cited study was done at Case Western Reserve Univ, just a few minutes’ walk from where I am right now.
Others (Pratt 1969, Harris 1970) had previously noticed increased macrophages in BAL specimens from smokers.

10.
The very next year, an electron microscopic study looked at these pigmented macrophages from smokers in breathtaking detail!
The study was by Brody and Craighead, 1975. They called the cytoplasmic particles derived from cigarette smoke “smokers’ inclusions”
PMID: 163418
The very next year, an electron microscopic study looked at these pigmented macrophages from smokers in breathtaking detail!
The study was by Brody and Craighead, 1975. They called the cytoplasmic particles derived from cigarette smoke “smokers’ inclusions”
PMID: 163418

• • •
Missing some Tweet in this thread? You can try to
force a refresh