1/ Happy #TweetorialTuesday from @ChrisDJacksonMD!
Hypothesis-driven history? Bedside rounds? How do we put it all together?
Don't worry, your #MedEdTwagTeam crew is here to help with this week's thread!
Hypothesis-driven history? Bedside rounds? How do we put it all together?
Don't worry, your #MedEdTwagTeam crew is here to help with this week's thread!

3/ Outlined in this figure are the 5 steps in a hypothesis-driven-history encounter
Depending upon the patient scenario, you may use some or all of these steps.
More important, though, is engaging the learner at each point towards obtaining the diagnosis for the patient
Depending upon the patient scenario, you may use some or all of these steps.
More important, though, is engaging the learner at each point towards obtaining the diagnosis for the patient

4/ While I'm a fan of hypothesis-driven history taking, not all encounters require it. If the patient has an established diagnosis with a clear management plan, HDH may not contribute much to the patient's care.
Outlined below are the times when HDH taking is most impactful
Outlined below are the times when HDH taking is most impactful

5/ So how do we introduce the hypothesis-driven history when we are teaching our learners?
6/ The hypothesis-driven history can be done during teaching rounds. Below is a standard teaching script I use with my residents. 

7/ The HPI is the best place to think about building hypothesis-driven history. HPI is the most data-rich section of the history IMHO. Focusing on the HPI helps you and the learner focus on the main target, which is clarifying diagnostic conundrums with targeted questions. 

8/The journey (clinical reasoning) is just as important as the destination (dx). Prior to the hypothesis-driven history, I tell learners it's okay to leave the history & not know the dx. It is more important to partner with patients and admit our dx uncertainty when appropriate. 

9/ Let’s use a common clinical scenario from the wards to demonstrate how a hypothesis-driven history can be useful 

10/ Over the next few tweets, we will use this framework to further dive into this clinical scenario 

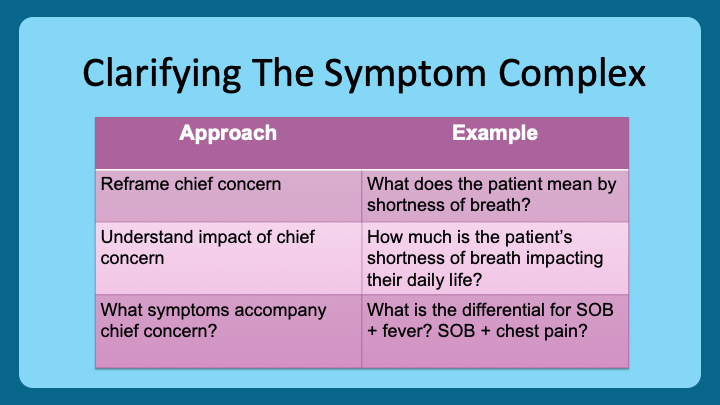
11/The hypothesis-driven history starts with the chief concern. Do we know what it is and why it brought the patient to the hospital? If we don’t, these will be questions to ask the patient when we evaluate them. I do this outside the room to prime the learner for the visit. 
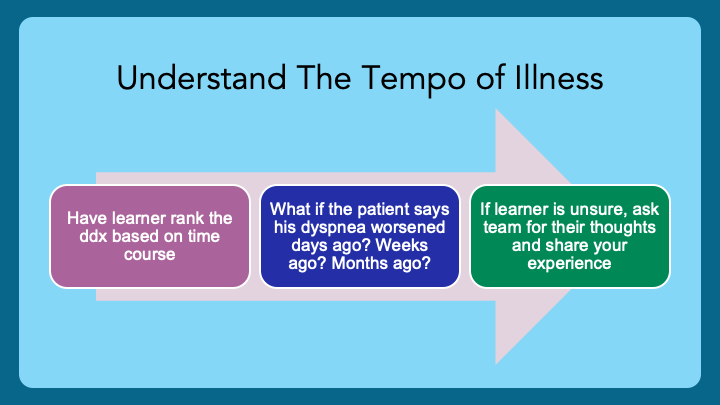
12/ When learners consider their illness scripts for different diseases, time is a key distinguishing factor (H/T @3owllearning). For example, a patient with acute dyspnea + fever is more likely to have CAP than one with chronic SOB and edema. This step occurs outside the room. 
13/ Developing a ddx for a hypothesis-driven history can be challenging.
Rather than listing innumerable diagnoses, I have my learners consider these three questions with input from the entire team.
Using these 3 questions, the list becomes more prioritized to the patient.
Rather than listing innumerable diagnoses, I have my learners consider these three questions with input from the entire team.
Using these 3 questions, the list becomes more prioritized to the patient.

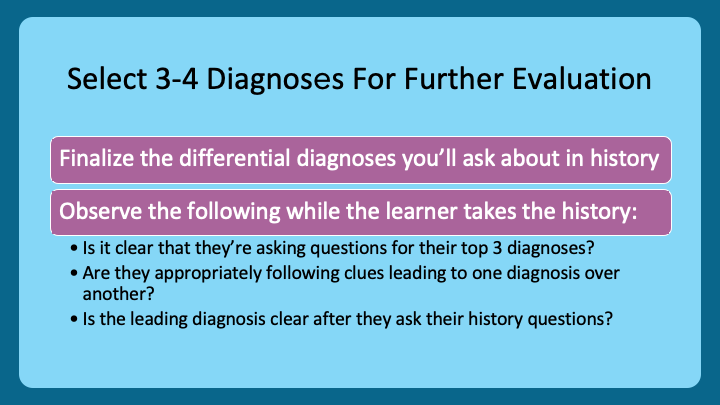
14/After clarifying the chief concern & tempo of illness, the learner should have a few diagnostic hypotheses.
I like them to list them and why they are the most important ones.
With this information, the learner talks with the patient while you observe them.
I like them to list them and why they are the most important ones.
With this information, the learner talks with the patient while you observe them.
15/ Closing out the hypothesis-driven history is developing a working diagnosis.
I encourage the learner to reason aloud, highlighting why they made the diagnosis & excluded others.
As they reason, I affirm or correct their diagnostic thought process.
I encourage the learner to reason aloud, highlighting why they made the diagnosis & excluded others.
As they reason, I affirm or correct their diagnostic thought process.

16/ Learning begins & ends with reflection. Debriefing with learners after doing a hypothesis-driven history allows them to see what important stops they made on the journey to the diagnosis. I try to do this after the patient encounter or at the end of the day one-on-one. 

17/ Highlighted in this figure are some of my favorite resources to support learners in developing their hypothesis-driven-history-taking skills.
Some of the best sources on Twitter to follow regarding HDH are @adamcifu @AdamRodmanMD @Sharminzi @CPSolvers @DxRxEdu @rabihmgeha
Some of the best sources on Twitter to follow regarding HDH are @adamcifu @AdamRodmanMD @Sharminzi @CPSolvers @DxRxEdu @rabihmgeha

18/ Please join us next week as @JenniferSpicer4 introduces bedside physical exam teaching.
You can find our previous threads by following @MedEdTwagTeam
You can find our previous threads by following @MedEdTwagTeam

• • •
Missing some Tweet in this thread? You can try to
force a refresh