1/
There have been a lot of “❓cerebritis” on the neuroICU signouts this year.
I, too, have some questions re: cerebritis… mainly, like what the heck is cerebritis and how are these “cerebritis” pictures related?
A #tweetorial #EmoryNCCTweetorials @MedTweetorials
There have been a lot of “❓cerebritis” on the neuroICU signouts this year.
I, too, have some questions re: cerebritis… mainly, like what the heck is cerebritis and how are these “cerebritis” pictures related?
A #tweetorial #EmoryNCCTweetorials @MedTweetorials

2/
When you hear 'cerebritis' you think ...
When you hear 'cerebritis' you think ...
3/
We'll get there.
But 1⃣st, it's important to realize there are many different forms of neurologic "-itis" 🔥
⭐️Meningitis=inflammation of the meninges
This comes in two flavors🍦 :
👉pachymengitis
👉leptomeningitis
⭐️Pachy-meningitis =🔥 of the “thick membrane” (dura)
We'll get there.
But 1⃣st, it's important to realize there are many different forms of neurologic "-itis" 🔥
⭐️Meningitis=inflammation of the meninges
This comes in two flavors🍦 :
👉pachymengitis
👉leptomeningitis
⭐️Pachy-meningitis =🔥 of the “thick membrane” (dura)

4/
⭐️Leptomeningitis = inflammation of the “thin membrain” (arachnoid and pia)
The two images ↕️ highlight the difference in these entities with contrast enhancement.
However, not all contrast enhancement is “-itis.”
⭐️Leptomeningitis = inflammation of the “thin membrain” (arachnoid and pia)
The two images ↕️ highlight the difference in these entities with contrast enhancement.
However, not all contrast enhancement is “-itis.”

5/
Both lepto & pachymeningeal enhancement can be caused by neoplastic, infiltrative, and reactive conditions.
See ⬇️for an awesome extended differential!
@CPSolvers @KirtanPatolia
Both lepto & pachymeningeal enhancement can be caused by neoplastic, infiltrative, and reactive conditions.
See ⬇️for an awesome extended differential!
@CPSolvers @KirtanPatolia
https://twitter.com/KirtanPatolia/status/1507374719364136964
6/
Ventriculitis = 🔥 of the ventricles
Encephalitis =🔥 of the enkephalos (Greek for “brain,” the brain parenchyma)
The cranial nerves are named: vestibular neuritis, optic neuritis etc... & then there is angiitis / vasculitis of the CNS (@AaronLBerkowitz’s favorite) 😉
Ventriculitis = 🔥 of the ventricles
Encephalitis =🔥 of the enkephalos (Greek for “brain,” the brain parenchyma)
The cranial nerves are named: vestibular neuritis, optic neuritis etc... & then there is angiitis / vasculitis of the CNS (@AaronLBerkowitz’s favorite) 😉
7/
So …what, then, is cerebritis??
Vague inflammation of the “cerebrum”? Wouldn’t that be covered by “encephalitis"?
And is “lupus cerebritis” the same thing as other forms of “cerebritis"?
For the last question, the short answer is:
So …what, then, is cerebritis??
Vague inflammation of the “cerebrum”? Wouldn’t that be covered by “encephalitis"?
And is “lupus cerebritis” the same thing as other forms of “cerebritis"?
For the last question, the short answer is:
8/
Non-lupus cerebritis is inflammation of any intracranial structures.
Its most often caused by an infectious, pyogenic pathogen & tends to be invasive, invading many/any anatomic regions-- dura, subdural space, arachnoid, parenchyma...its not a well localized inflammation.
Non-lupus cerebritis is inflammation of any intracranial structures.
Its most often caused by an infectious, pyogenic pathogen & tends to be invasive, invading many/any anatomic regions-- dura, subdural space, arachnoid, parenchyma...its not a well localized inflammation.

9/
Another way to think about non-lupus cerebritis is to think of it as a “pre-abscess.”
In the early phase bacterial invasion results in perivascular inflammation & softening of the brain tissue
Look for T2 hyperintensity, DWI restriction, & poorly defined enhancement.↕️
Another way to think about non-lupus cerebritis is to think of it as a “pre-abscess.”
In the early phase bacterial invasion results in perivascular inflammation & softening of the brain tissue
Look for T2 hyperintensity, DWI restriction, & poorly defined enhancement.↕️

10/
Untreated the inflammatory response results in a walled off abscess, and/or subdural empyema depending on the location of the inflammation.
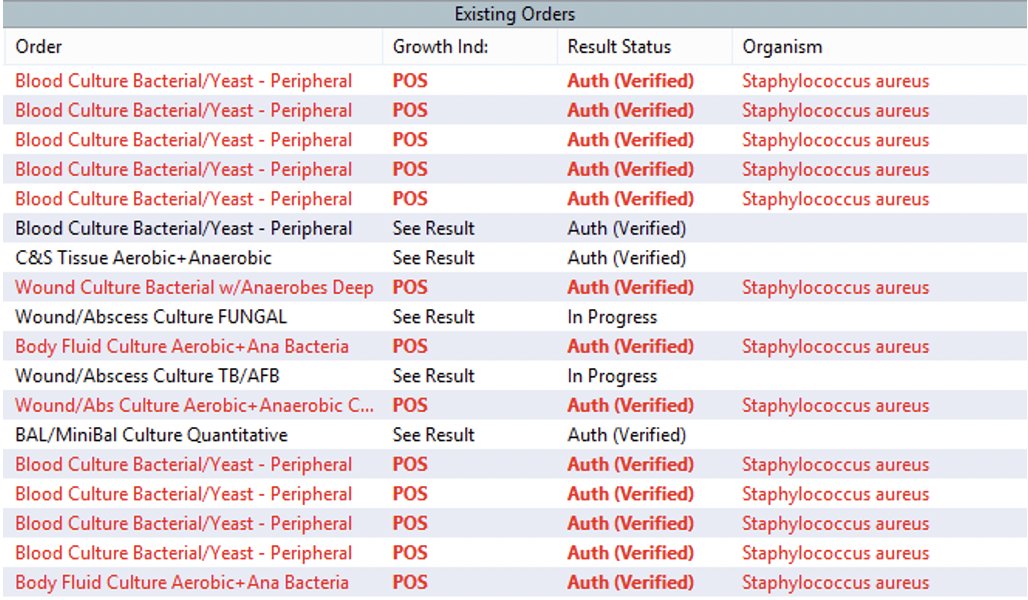
Microbiology can be difficult to diagnose because the CSF may be sterile, and aspiration may be necessary.
Untreated the inflammatory response results in a walled off abscess, and/or subdural empyema depending on the location of the inflammation.
Microbiology can be difficult to diagnose because the CSF may be sterile, and aspiration may be necessary.
10/
Of course, a forming abscess is not the only thing that causes patchy diffusion restriction and enhancement.
The differential for non-lupus cerebritis includes:
💥High grade neoplasms
💥Subacute infarcts
💥Mets
💥Radiation necrosis
💥Demyelinating disease
Of course, a forming abscess is not the only thing that causes patchy diffusion restriction and enhancement.
The differential for non-lupus cerebritis includes:
💥High grade neoplasms
💥Subacute infarcts
💥Mets
💥Radiation necrosis
💥Demyelinating disease
11/
There is potentially a role for advanced neuroimaging like MR spectroscopy especially in cases where aspiration/biopsy would have high morbidity.
Imaging of Cerebritis, Encephalitis, and Brain Abscess sciencedirect.com/science/articl…
There is potentially a role for advanced neuroimaging like MR spectroscopy especially in cases where aspiration/biopsy would have high morbidity.
Imaging of Cerebritis, Encephalitis, and Brain Abscess sciencedirect.com/science/articl…
12/
So then...Is lupus cerebritis related at all? Basically, no.
Lupus cerebritis is an outdated term which has been replaced with neuropsychiatric SLE (NPSLE). But even NPSLE is a vague umbrella term which covers everything from headaches to stroke.
Kivity et al. BMC med
So then...Is lupus cerebritis related at all? Basically, no.
Lupus cerebritis is an outdated term which has been replaced with neuropsychiatric SLE (NPSLE). But even NPSLE is a vague umbrella term which covers everything from headaches to stroke.
Kivity et al. BMC med

13/
The pathophysiology is complicated and may be antibody-mediated, vasculopathy, hypercoaguable state, cytokine-induced neuroloxic, and loss of neuroplasticity.
Neuropsychiatric lupus: a mosaic of clinical presentations pubmed.ncbi.nlm.nih.gov/25858312/
The pathophysiology is complicated and may be antibody-mediated, vasculopathy, hypercoaguable state, cytokine-induced neuroloxic, and loss of neuroplasticity.
Neuropsychiatric lupus: a mosaic of clinical presentations pubmed.ncbi.nlm.nih.gov/25858312/

13/
Many of these neuropsychiatric symptoms have no MRI findings.
Cerebrovascular dz is a notable exception.
If “lupus cerebritis” shows up in an imaging report the likely pathophysiology is cerebrovascular disease.
Lupus Cerebritis = Stroke until Proven Otherwise

Many of these neuropsychiatric symptoms have no MRI findings.
Cerebrovascular dz is a notable exception.
If “lupus cerebritis” shows up in an imaging report the likely pathophysiology is cerebrovascular disease.
Lupus Cerebritis = Stroke until Proven Otherwise


14/
⚠️This DOES NOT mean that lupus cerebritis = vasculitis.
Remember, that vasculitis, by definition[!], involves inflammation. You CANNOT look at diffusion restriction on an MRI & determine vasculitis.
⚠️This DOES NOT mean that lupus cerebritis = vasculitis.
Remember, that vasculitis, by definition[!], involves inflammation. You CANNOT look at diffusion restriction on an MRI & determine vasculitis.
15/
In these patients, the most common pathology finding is thrombotic-vasculopathy. This may be due to:
✨antiphospholipid antibodies
✨immune complex/compliment activation.
SLE pts also can have:
✨cardiac emboli (Libman-Zachs endocarditis)
✨accelerated atherosclerosis.
In these patients, the most common pathology finding is thrombotic-vasculopathy. This may be due to:
✨antiphospholipid antibodies
✨immune complex/compliment activation.
SLE pts also can have:
✨cardiac emboli (Libman-Zachs endocarditis)
✨accelerated atherosclerosis.
16/
Can something other than cerebrovascular disease be going on?
Absolutely.
Given chronic immune suppression, SLE pts are at risk for infections (including the “non-lupus” form of “cerebritis”!) & can have demyelination, encephalitis, sz-related MRI.
Can something other than cerebrovascular disease be going on?
Absolutely.
Given chronic immune suppression, SLE pts are at risk for infections (including the “non-lupus” form of “cerebritis”!) & can have demyelination, encephalitis, sz-related MRI.
17/
But keep cerebrovascular dz high on Ddx.
LP and advanced neuroimaging can be helpful here. Vessel Wall Imaging has been reported to help differentiate which is interesting.
non-aneurysmal SAH in two patients with SLE: Case reports and literatu… pubmed.ncbi.nlm.nih.gov/27453474/
But keep cerebrovascular dz high on Ddx.
LP and advanced neuroimaging can be helpful here. Vessel Wall Imaging has been reported to help differentiate which is interesting.
non-aneurysmal SAH in two patients with SLE: Case reports and literatu… pubmed.ncbi.nlm.nih.gov/27453474/

19/
So, finally, how then are lupus cerebritis and infectious cerebritis at similar?
Again, they are mostly different, but in both you may find diffusion restriction and patchy contrast enhancement.
Context matters & the underlying pathology is almost always different.
So, finally, how then are lupus cerebritis and infectious cerebritis at similar?
Again, they are mostly different, but in both you may find diffusion restriction and patchy contrast enhancement.
Context matters & the underlying pathology is almost always different.

other experience with this twin moniker!? @CajalButterfly @AvrahamCooperMD @namorrismd @sigman_md @JayKinariwala @aszelikovich @aartisarwal @theABofPharmaC @SubinMatthews @SMuehlschMD @PulmCrit @a_charidimou @rkchoi @Capt_Ammonia @drdangayach @DxRxEdu @SCCM_Neuro
@EricLawson90 @SitaraKoneru @ACRheum @jhrheumatology @NMatch2022 @zach_london @ghoshal_shivani @EmoryNeurology @DanHarrisonMD
• • •
Missing some Tweet in this thread? You can try to
force a refresh