Pulse oximeters are widely used to monitor for low oxygen levels among #Covid19 patients at home.
But does pulse oximetry improve outcomes over monitoring for symptoms of shortness of breath?
Our team provides some answers today in @NEJM 🧵👇
nejm.org/doi/full/10.10… #SGIM22
But does pulse oximetry improve outcomes over monitoring for symptoms of shortness of breath?
Our team provides some answers today in @NEJM 🧵👇
nejm.org/doi/full/10.10… #SGIM22
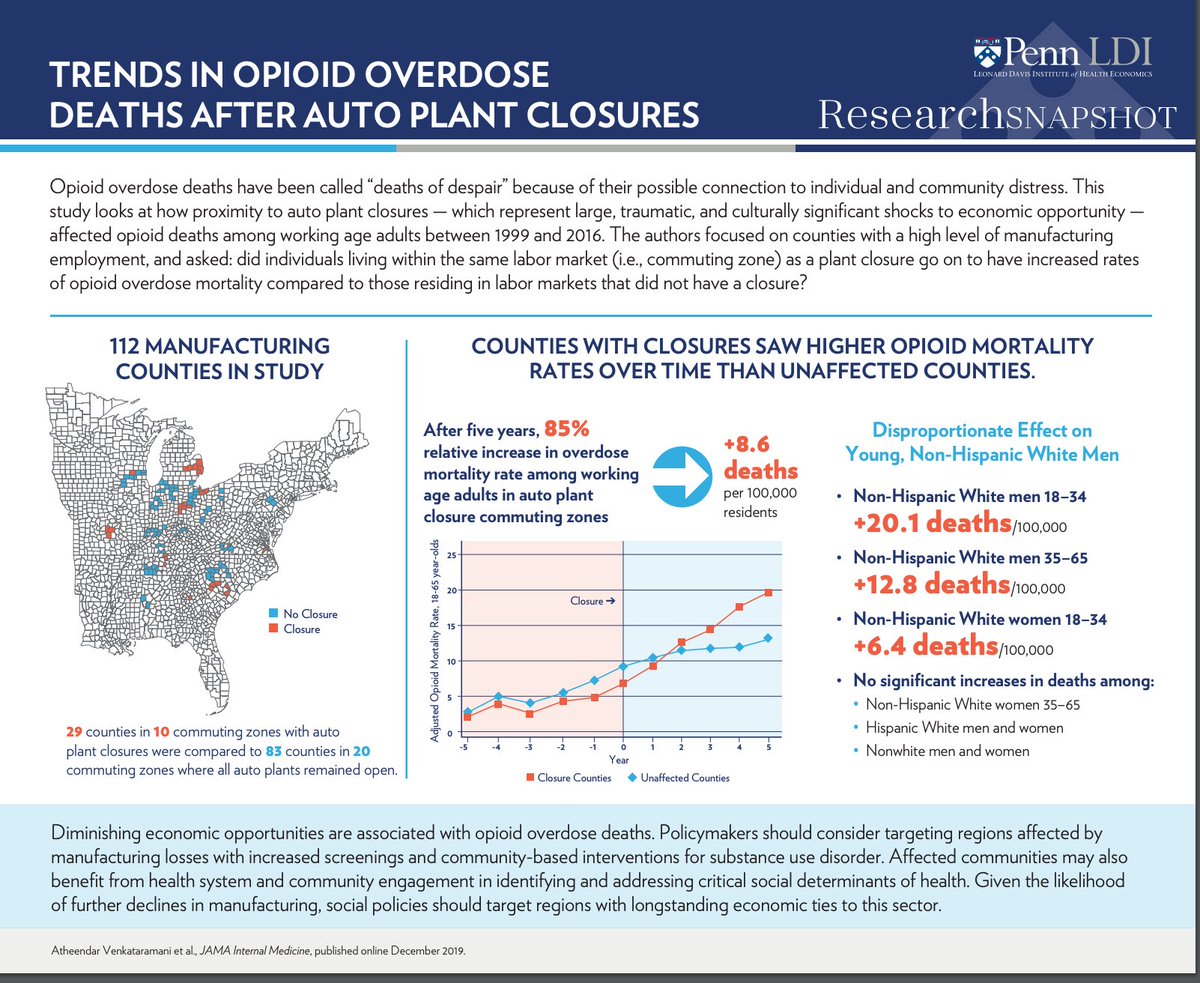
..First some context, early in the pandemic there were widespread accounts of #Covid19 patients presenting to the ER with relatively minor symptoms, but with markedly low oxygen levels, a phenomenon known as “silent hypoxia"...
nytimes.com/2020/04/20/opi…
nytimes.com/2020/04/20/opi…
...It was thought that use of a pulse oximeter could detect declining oxygen levels before symptoms develop, and provide an opportunity for the patients to get to the ER faster where they could be stabilized faster...nytimes.com/2020/04/24/wel…
...In the meantime, within two weeks of the first local #Covid19 diagnosis in March 2020, our health system, @PennMedicine, launched an automated text-messaging program called COVID Watch to check-in on newly diagnosed #Covid19 patients at home...pennmedicine.org/news/news-blog…
...Patients who text-back that they experiencing symptoms of shortness of breath would receive phone calls within 1 hour from an on-call nurse to either guide them to the ER, arrange an urgent tele med appointment, or continue to self-monitor... 



...Other health systems (e.g. Kaiser, VA), states (e.g. Vermont), and whole countries implemented programs to monitor #Covid19 patients at home with pulse oximeters...england.nhs.uk/nhs-at-home/co… 

...So after a scramble to get grant funding from
@PCORI our team set out to determine:
1) How do patients who receive symptom based monitoring (COVID Watch) do compared with no monitoring;
2) Can COVID Watch be improved with the addition of home pulse oximetry?....
@PCORI our team set out to determine:
1) How do patients who receive symptom based monitoring (COVID Watch) do compared with no monitoring;
2) Can COVID Watch be improved with the addition of home pulse oximetry?....
...We found that enrollment in the symptom-based monitoring program (COVID Watch) was associated with a significant reduction in mortality with faster presentation to the ER compared with no monitoring
See thread from our paper in @AnnalsofIM below...
See thread from our paper in @AnnalsofIM below...
https://twitter.com/kit_delgadoMD/status/1460590169715838976?s=20&t=jmY7U-dUEuxpdRm18ZSJZA
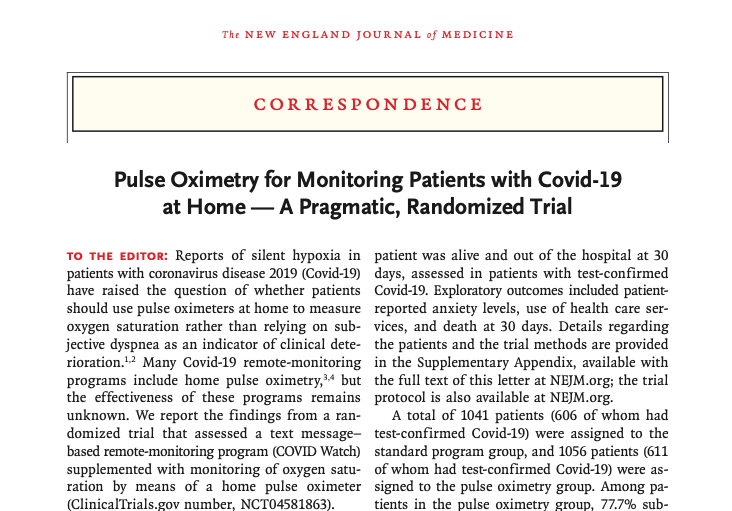
...We then set up a pragmatic randomized trial from Dec 2020 – Feb 2021 in which patients enrolled in COVID Watch as part of usual care were randomized to receive an overnight mailed pulse oximeter or just the standard COVID Watch program...
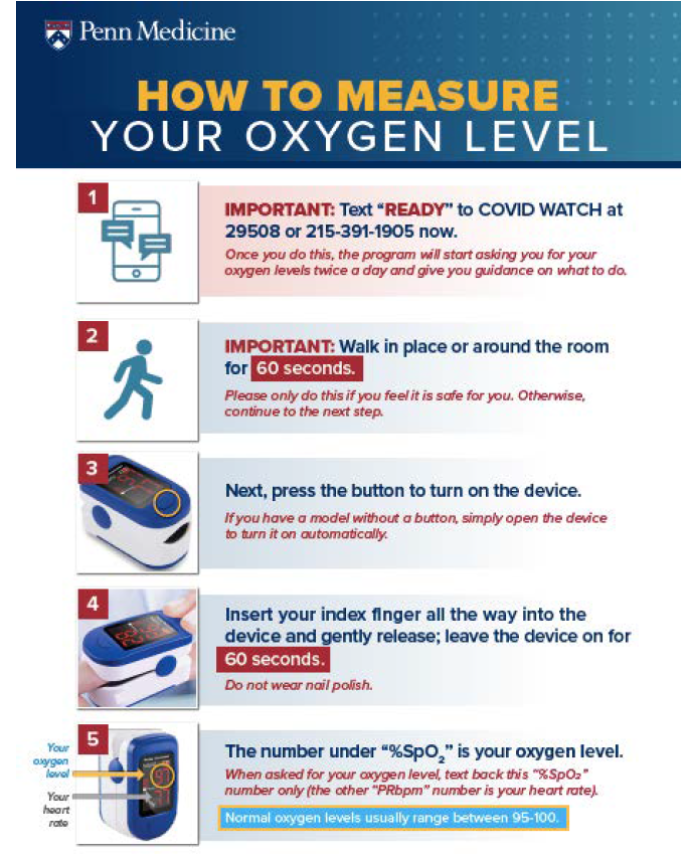
..Patients randomized to pulse oximetry were monitored for symptoms of shortness of breath. Then in addition to be asked about shortness of breath, they were asked to provide their pulse ox levels twice daily. An alert was triggered for declining oxygen levels or a level =<90%... 
We hypothesized that the addition of pulse oximeters could help in two ways:
1) Enable patients who feel “dyspnea” (aka shortness of breath) but have normal oxygen level to continue to self-monitor at home
2) And help patients who develop silent hypoxia to the hospital faster
1) Enable patients who feel “dyspnea” (aka shortness of breath) but have normal oxygen level to continue to self-monitor at home
2) And help patients who develop silent hypoxia to the hospital faster

..To capture both of these potential outcomes, we made our primary outcome days alive and out of hospital at 30 days after enrollment because patients would prefer to stay home if safe, but if needed, get treatment faster reducing time in the hospital and the risk of mortality...
...Under the outstanding, tactical leadership of co-lead authors @katleemd and @AnnaUma we enrolled 2,097 during the winter 2021 #Covid19 wave. The primary analysis was specified to be among the 1,217 with confirmed positive Covid19 tests within our health system....
...Among patients in the pulse oximetry group, 78% submitted at least one pulse oximetry reading; these patients submitted a mean of 10 readings, corresponding to a response rate of 69% to pulse oximetry check-ins...
...The main result: There was no difference in days alive and out of the hospital between the standard program and program + pulse oximetry. In sensitivity analyses this held up for all randomized patients and when just looking at those who actually used their pulse oximeter... 

...We also set out to ensure we would have a sufficiently large study sample to assess whether there were any differences within racial and ethnic subgroups to assess for equity in effects. We didn't find any differences...
...This is important because recent research has raised concerns that fingertip pulse oximeters may be less likely to detect low oxygen levels in Black patients (this paper came out in the middle of our trial)...nejm.org/doi/full/10.10…
...Across a large number of exploratory outcomes, we did not find any differences. This included patient reported anxiety, helpfulness, and confidence in managing #Covid19, time to return to the ER, rates of ER visits, hospitalizations, and death... 

...However, there was one difference. The group who received pulse oximeters did generate more alerts to the nurses and more phone calls indicating more clinical resources were required to manage the population...
...So what can we conclude? The addition of pulse oximetry to an established symptom based remote monitoring program did not improve clinical outcomes despite increased cost and resource use....
...This implies that low tech, symptom based monitoring with access to an on-call nurse is a scalable approach to continue to monitor large populations of #Covid19 patients...covidwatch.waytohealth.org...
..Important caveat. We did not compare handing out pulse oximeters to no monitoring in this trial. So for patients that don’t have access to on-call clinicians or a remote monitoring program, using a pulse oximeter may be reasonable. But so is monitoring for shortness of breath..
This was a pandemic labor of love involving a huge team of researchers, clinicians, innovators. Special shout outs to @katleemd (implementation lead), @AnnaUma (Covid Watch medical director), @khchaiyachati (co-PI), and @76Dalton @PM_Innovation leader and everyone on the team...
...And special thanks to @PCORI for funding this effort.
With the limited word count in the paper, figure some extra context would be helpful.
And check out the supplement for the all the details and release below.
(nejm.org/doi/suppl/10.1…)
Thanks!/
pennmedicine.org/news/news-rele…
With the limited word count in the paper, figure some extra context would be helpful.
And check out the supplement for the all the details and release below.
(nejm.org/doi/suppl/10.1…)
Thanks!/
pennmedicine.org/news/news-rele…
…PS if you are at #SGIM22, COVID Watch Medical Director and co-lead author @AnnaUma will be presenting this paper on Friday. Check out her presentation! 

• • •
Missing some Tweet in this thread? You can try to
force a refresh