@Rajiv_Sinanan @ThinkingCC 1/ Real reason(s) based on my conversations with people from different backgrounds:
Private practice: "#POCUS sounds interesting but I ain't got time for that. Will consider if I get compensated"
Academia: (not generalizing but most places)
Emphasis is on funded research
Private practice: "#POCUS sounds interesting but I ain't got time for that. Will consider if I get compensated"
Academia: (not generalizing but most places)
Emphasis is on funded research
@Rajiv_Sinanan @ThinkingCC 2/ Clinical faculty are hired for clinical duties, outreach dialysis etc., which is fair but the problem is educational endeavors are rarely rewarded/provided with protected time. Faculty who want to be #POCUS champions must first learn it (either from institutional experts or
@Rajiv_Sinanan @ThinkingCC 3/ external courses), then integrate into curriculum, take care of administrative stuff/image archiving, prepare didactic material etc., which consume a lot of time and effort. Without dedicated protected time, its almost impossible to continue the initial enthusiasm.
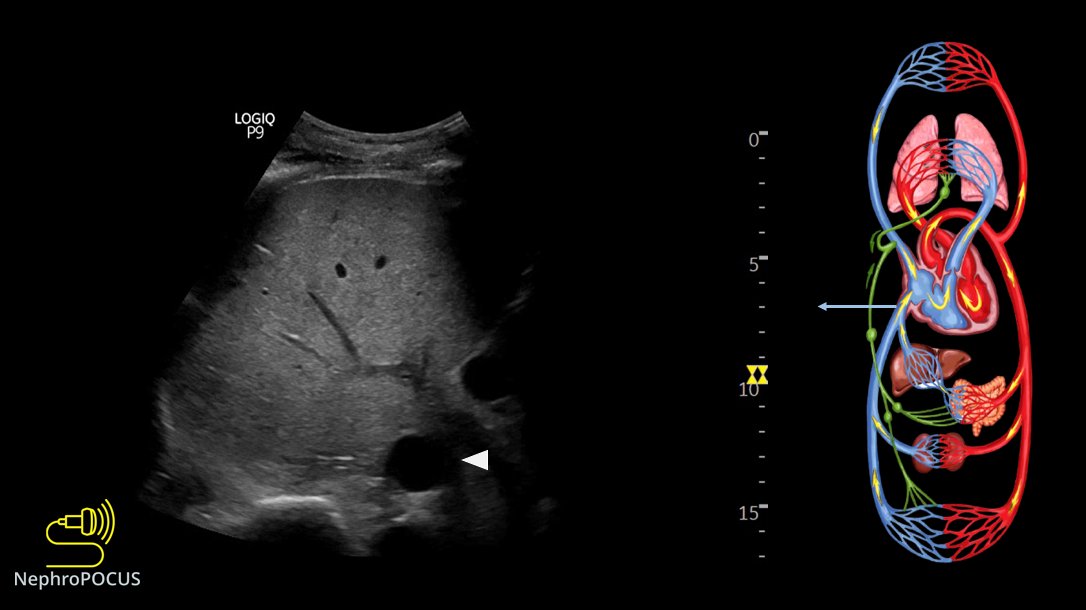
@Rajiv_Sinanan @ThinkingCC 4/ Other problem is that people who never touched the probe or understand its utility form opinions (& propagate) about which sonographic applications are relevant to nephrology and which are not. Many people think FoCUS = comprehensive echocardiography (which is bad not only
@Rajiv_Sinanan @ThinkingCC 5/ from the perspective of discouraging prospective learners but on the other hand, promotes false sense of confidence among novice learners [that's why I put my plant infographic in talks]). 
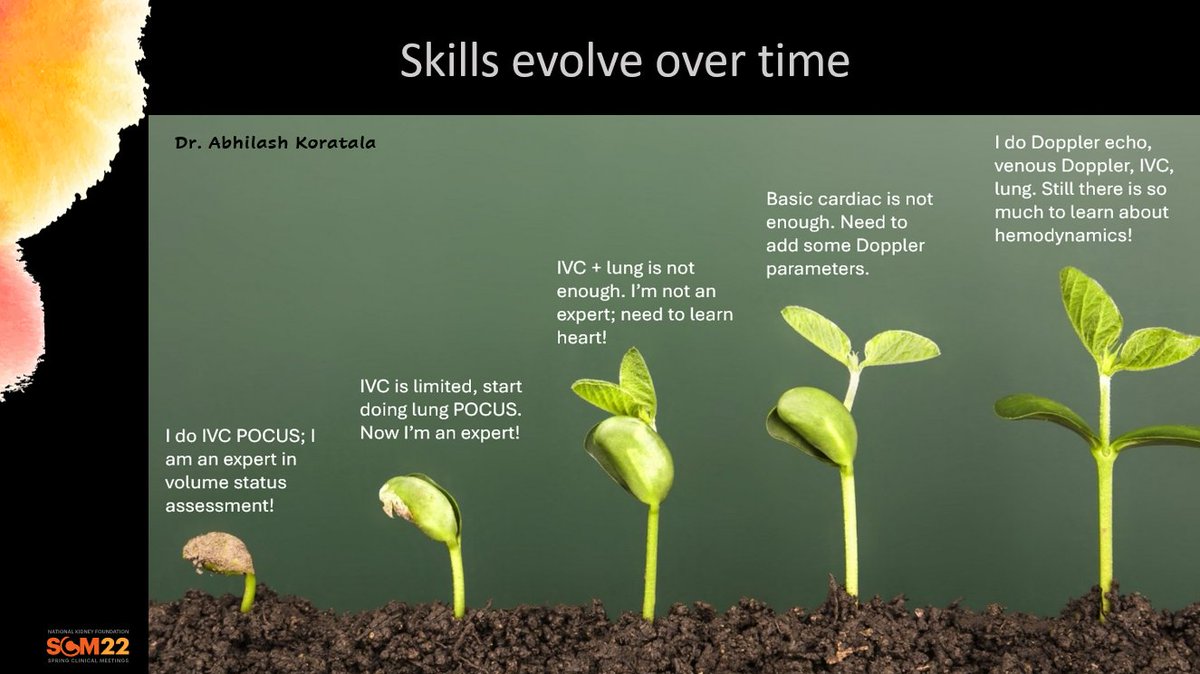
@Rajiv_Sinanan @ThinkingCC 6/ I've seen scenarios where junior faculty express interest in #POCUS and the so-called mentor or division chief who never heard about it say "why not publish something first, the we can apply for funding and you get protected time".
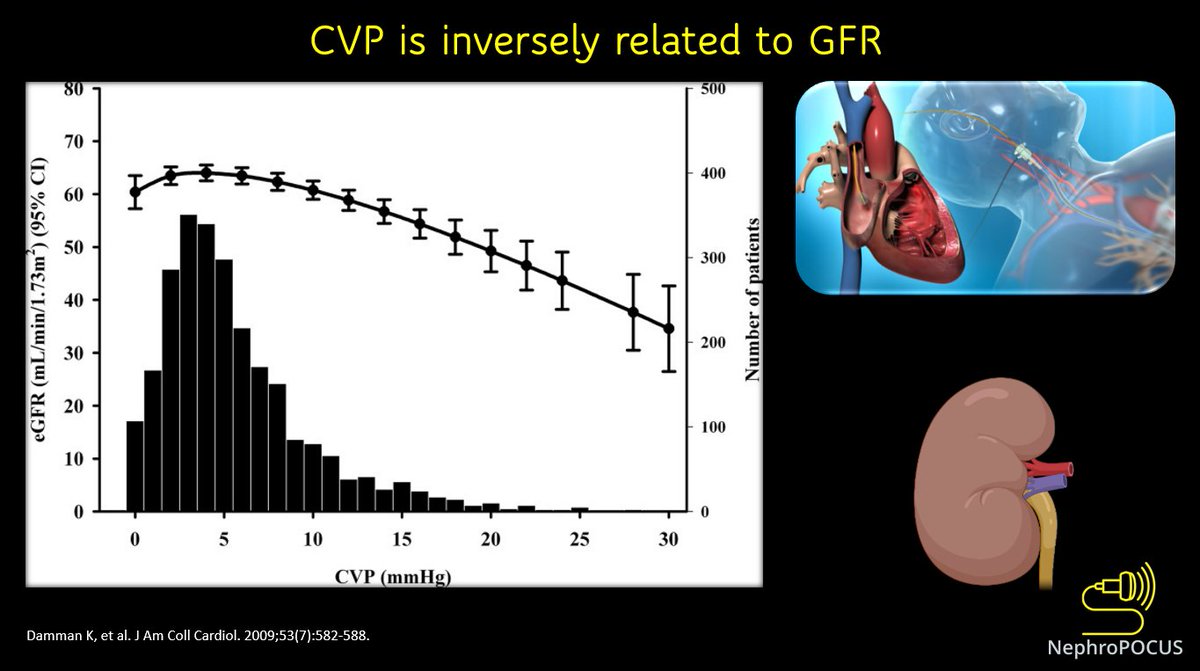
@Rajiv_Sinanan @ThinkingCC 7/ In mad rush for research funding, clinical skills & education of future generations suffer. Recent study where they looked at whether POCUS improves outcomes is a classic example where the investigators had probably thought POCUS = snake oil [cures all!🤔]) 
@Rajiv_Sinanan @ThinkingCC 8/ Bottom line is lack of understanding of the utility + academic inertia.
• • •
Missing some Tweet in this thread? You can try to
force a refresh