One of my favorite topics in #POCUS - various effusions seen from different sonographic windows.
Here is a thread 🧵with labeled images for those interested.
1. PLAX view - pericardial effusion - anterior to descending aorta ⚫️below LA), wedge shaped
#MedEd #IMPOCUS #Nephpearls
Here is a thread 🧵with labeled images for those interested.
1. PLAX view - pericardial effusion - anterior to descending aorta ⚫️below LA), wedge shaped
#MedEd #IMPOCUS #Nephpearls
2/ PSAX papillary muscle view
LV is think as many of my patients have #CKD and LVH (as well as mitral annular calcification seen on PLAX view above)
#Nephrology #POCUS
LV is think as many of my patients have #CKD and LVH (as well as mitral annular calcification seen on PLAX view above)
#Nephrology #POCUS
3/ Apical 4-chamber view
Sometimes, effusions may be missed due to inadequate visualization of ventricular free wall/lung interference. Always pay attention to the RA area
#POCUS
Sometimes, effusions may be missed due to inadequate visualization of ventricular free wall/lung interference. Always pay attention to the RA area
#POCUS
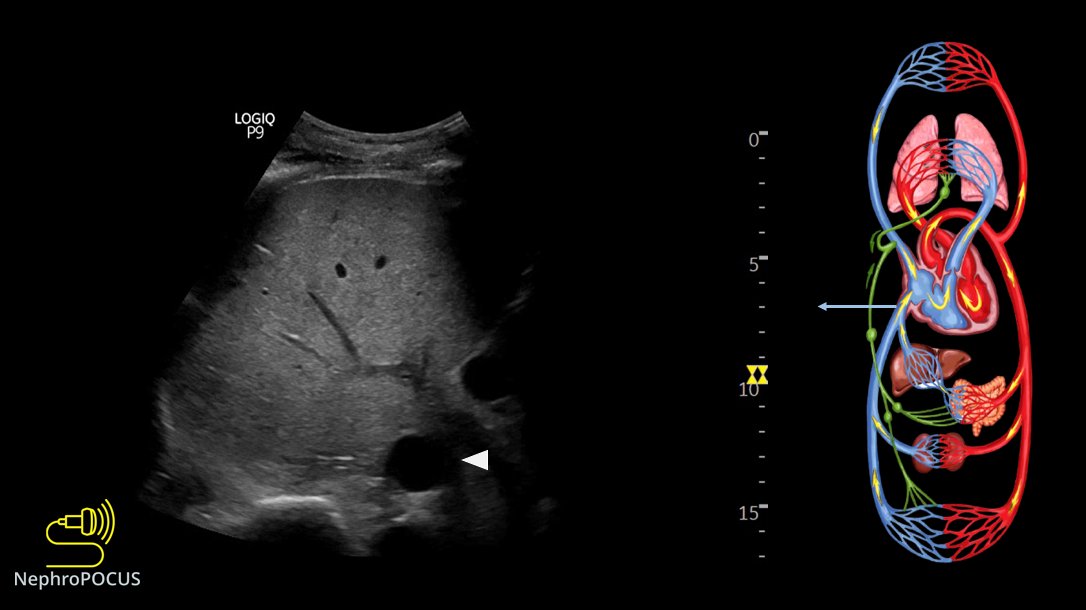
5/ Pericardial effusion is usually detectable on IVC long axis view as well. You just need to pay attention and identify anechoic space between the diaphragm and the heart.
#POCUS
#POCUS
6/ Pleural effusion (left) from PLAX view - posterior to descending aorta. Often the lung is visible floating in the effusion.
#POCUS
#POCUS
7/ Here is another example of left pleural effusion on PLAX view. While lung is not visualized, the effusion is NOT wedge shaped and follows the curvature of the chest wall.
#POCUS
#POCUS
8/ #POCUS = #anatomy + commonsense
Here is the anatomic correlation that explains why descending thoracic aorta is an important landmark to distinguish pericardial and pleural effusions.
Here is the anatomic correlation that explains why descending thoracic aorta is an important landmark to distinguish pericardial and pleural effusions.

9/ Sometimes (thin patients, increased depth) you can see both left and right pleural effusions from the PLAX window. Compare with CT image above.
#POCUS
#POCUS
10/ Pleural effusion from PSAX window. Note the floating lung, which is a big clue in any window.
#POCUS
#POCUS
👆 is called the 'fox tail' sign #POCUS
14/ Apical window demonstrating both pericardial and left pleural effusion.
16/ We see a circumferential pericardial effusion in this subxiphoid view. Anything else?
Answer in next tweet
#POCUS
Answer in next tweet
#POCUS
18/ Another example of ascites seen in the subxiphoid window. Liver comes into view intermittently, which is a clue to ascites (like lung is to pleural effusion)
#POCUS
#POCUS
19/ The famous Boomerang sign - right pleural effusion seen from the subxiphoid window. This is often confused with ascites.
#POCUS
#POCUS
21/ Coming to the end of long 🧵
#POCUS example showing multiple effusions seen from the subxiphoid window.
#POCUS example showing multiple effusions seen from the subxiphoid window.
All the above images can be found in my recent RFN posts. Unfortunately, the gif files are not playing.
🔗renalfellow.org/2021/10/21/ide…
🔗renalfellow.org/2022/04/18/ide…
🔗renalfellow.org/2021/10/21/ide…
🔗renalfellow.org/2022/04/18/ide…
• • •
Missing some Tweet in this thread? You can try to
force a refresh