1/Mike Tyson once said, “Everyone has a plan until they get punched.”
In honor of all the great hooks and crosses—here is a #tweetorial about mandibular fxs! #FOAMed #medtwitter #Meded #neurorad #HNrad #FOAMrad #Medstudenttwitter @MedTweetorials
In honor of all the great hooks and crosses—here is a #tweetorial about mandibular fxs! #FOAMed #medtwitter #Meded #neurorad #HNrad #FOAMrad #Medstudenttwitter @MedTweetorials
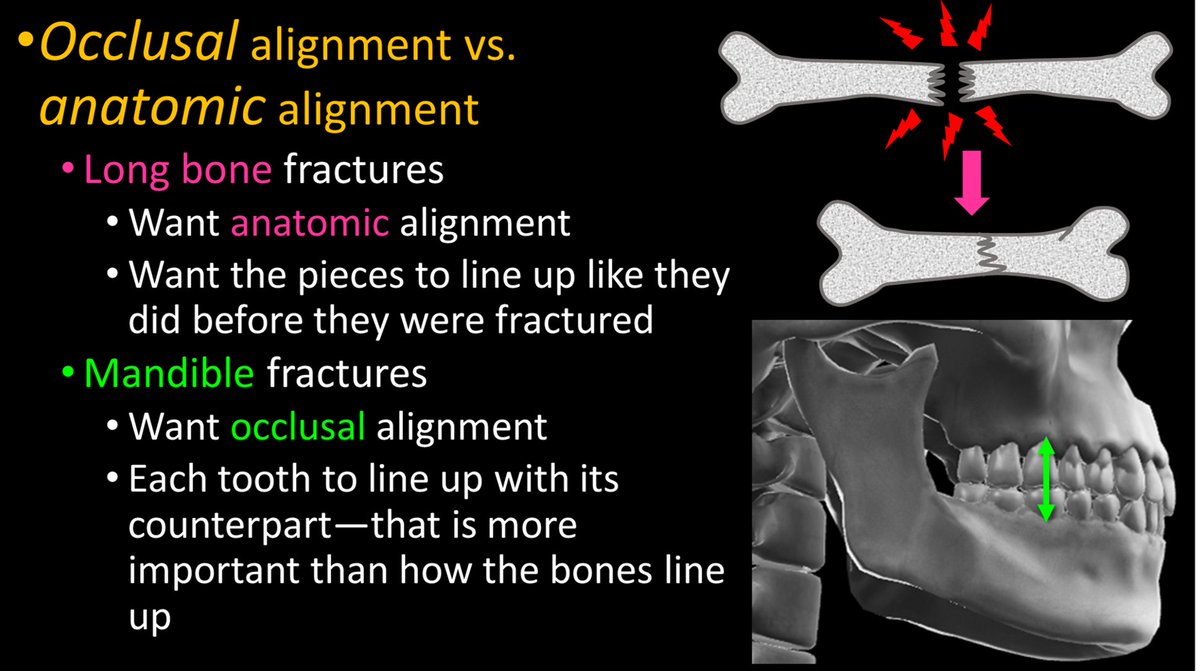
2/A key concept in these fxs is dental occlusion. The jaw is meant to chew. To crush food, teeth need to come as close together as possible—occlusion. Each tooth needs to meet up with its counterpart that fits with it, so no room is left for food—and food will be crushed. 
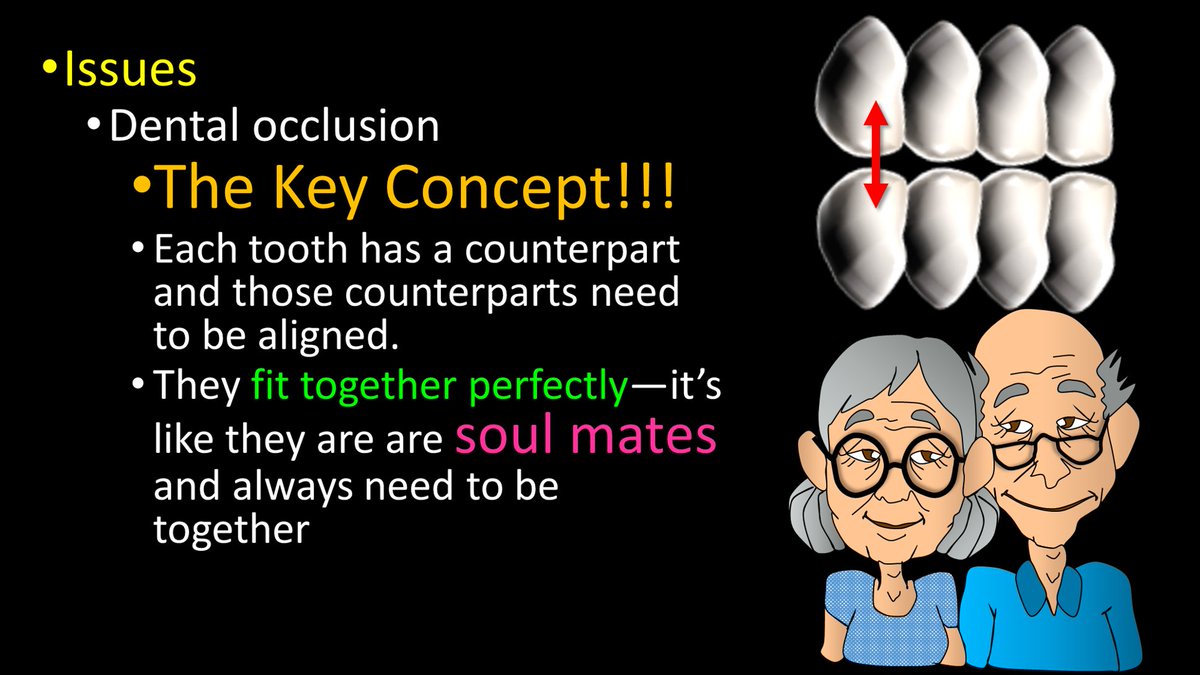
3/Occlusion can be lost w/a fx. The importance of dental occlusion makes mandibular fxs different from other fxs. Usually, we want to fix a bone so that it lines up again. But for the mandible, we want to fix it so the TEETH line up again—so chewing will work. 
4/Another important concept is multiplicity. It used to be taught that the mandible was a ring w/the skullbase—& you can’t break a ring in one place, so every mandible fx had to have a 2nd one. But this is only true ~50% of time—but it is still worth it to look for the 2nd fx. 

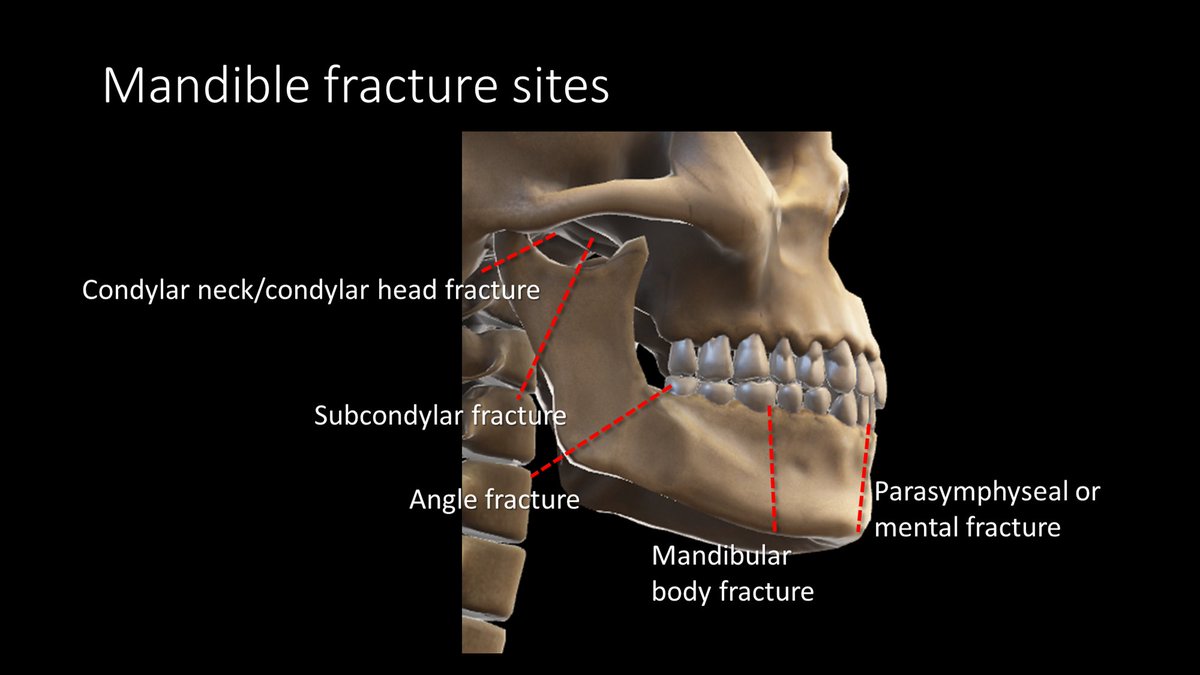
5/Because of the shape of the mandible and the typical forces applied to it, mandibular fractures usually occur at the same few locations. But the names of these fxs are not always intuitive—at least not without a tweetorial to help explain them! 😉 
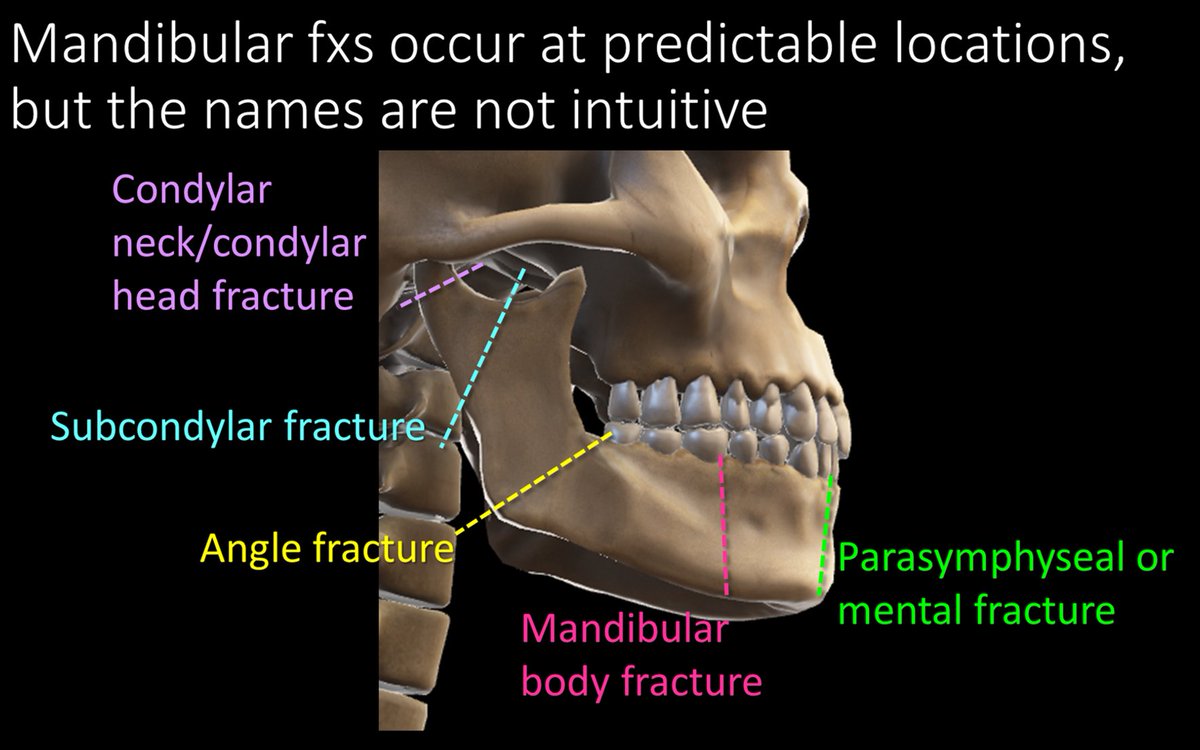
6/Well, perhaps I lied a little. The most common fx does have an intuitive name. An angle fx starts at…wait for it…the angle and extends into socket of the 3rd molar. If you can’t remember an angle fx starts at the mandibular angle, then not even this tweetorial can help you! 

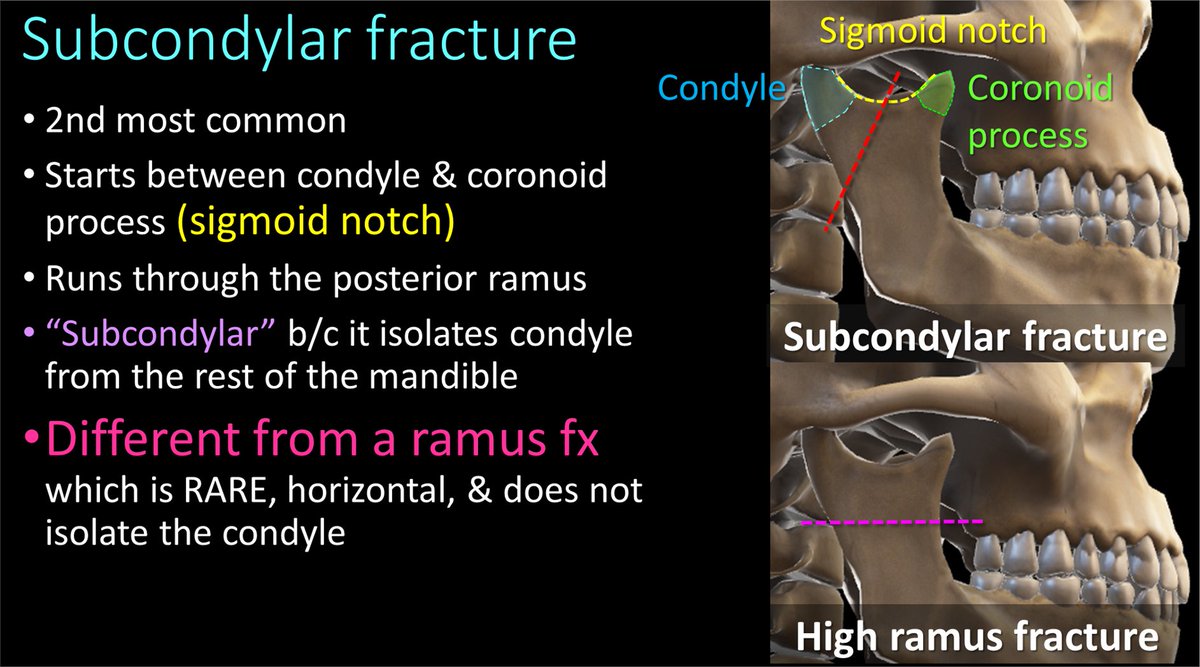
7/A subcondylar fracture starts from the notch between the condyle and coronoid process, called the sigmoid notch and extends into the posterior ramus. Don’t call this a ramus fx bc a ramus fx goes straight horizontally through the ramus! 
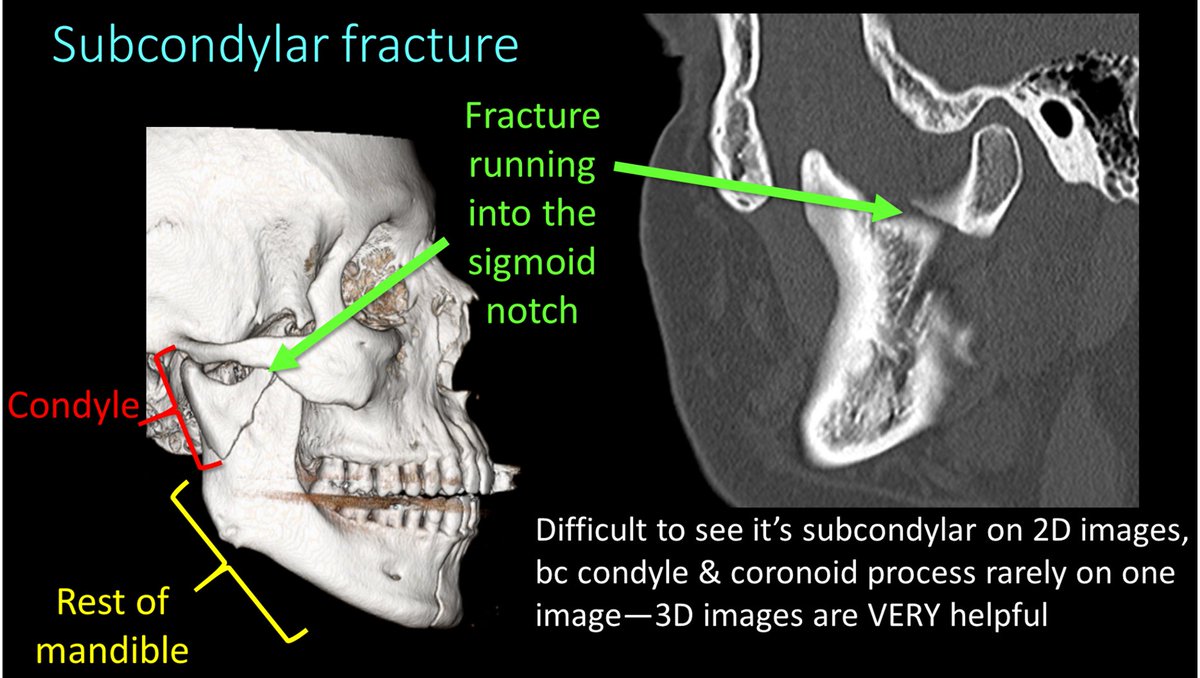
8/Here are examples of subcondylar fxs. A key finding in subcondylar fxs is that it separates the condyle from the rest of the mandible. It can be difficult to see the fx running through the sigmoid notch & ramus on 2D images—3D images can be helpful to see the fx anatomy. 
9/I remember subcondylar fxs bc they separate the condyle from the rest of the mandible. If you isolate someone, you make them feel SUBpar—so SUBcondylar fxs make the condyle feel subpar bc they separate it from the rest of the mandible! 

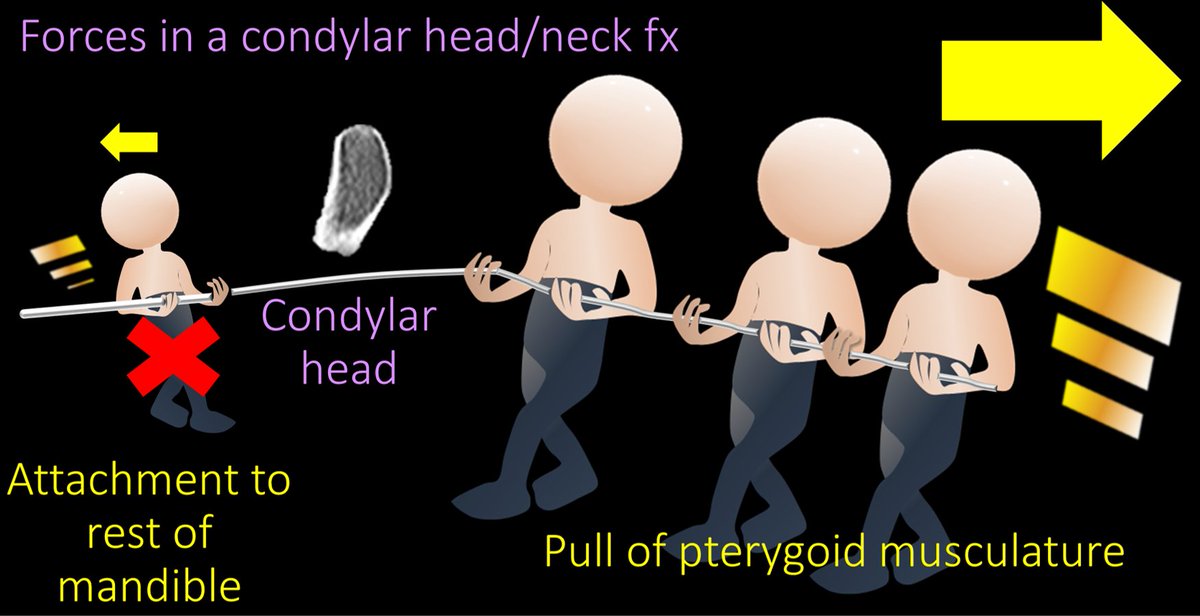
10/Condylar head/neck fxs are easy to remember—they are through, well, the condylar head or neck. These are fx/dislocations. Pterygoid muscles attach to the head & pull medially. So when the head is no longer attached to the mandible, pterygoids are unopposed & pull it medially. 

11/So if you ever see a condylar head displaced medially, you know it is a condylar head or neck fracture bc this is where the pterygoids are unopposed and pull medially! 
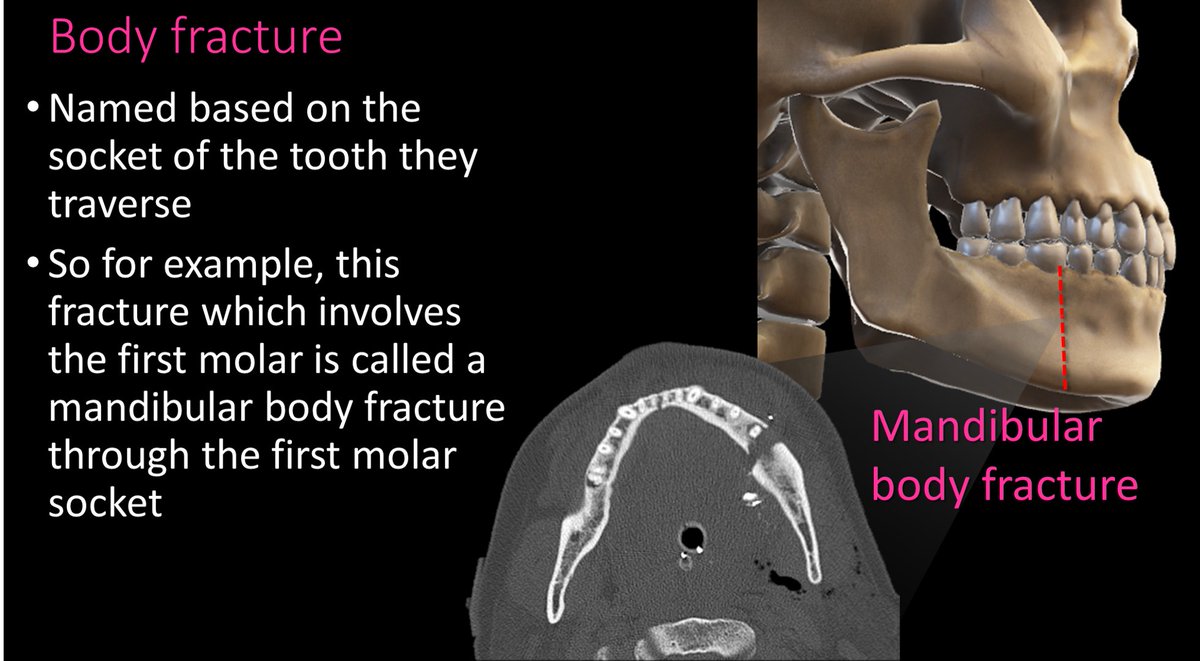
12/Body fxs are through the body of the mandible and are named for the tooth socket that they involve. So you would say “A mandibular body fx through the FILL IN THE BLANK TOOTH socket.” 
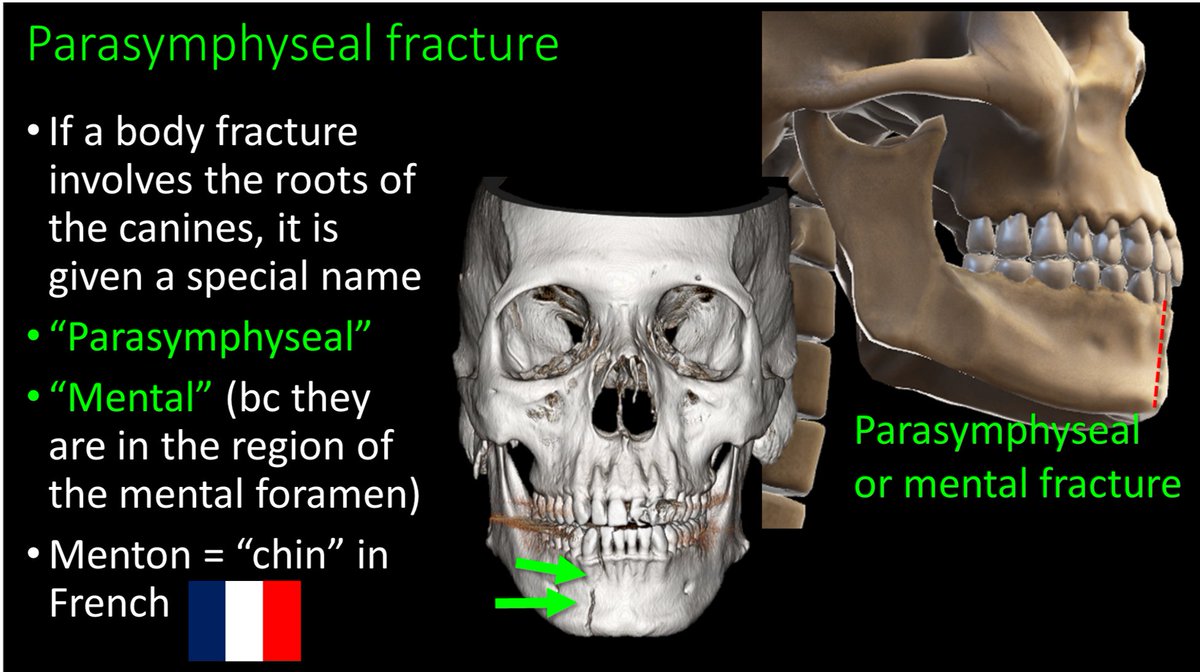
13/Body fxs through the canine are given the special name “parasymphaseal” or “mental” fx bc they are near the mental foramen where the inferior alveolar nerve exits. Menton means “chin” in French, so if they are a body fx anteriorly near the chin, they are “mental” fxs 
• • •
Missing some Tweet in this thread? You can try to
force a refresh