#POCUS #MedTwitter #Nephpearls
Many #VExUS enthusiasts asked for a #tweetorial on image acquisition pearls. Did one b4 but time for an updated one 🧵
#1 Let's start with basics
Color Doppler identifies the flow + tells the direction (blue is away & red towards the probe [BART])
Many #VExUS enthusiasts asked for a #tweetorial on image acquisition pearls. Did one b4 but time for an updated one 🧵
#1 Let's start with basics
Color Doppler identifies the flow + tells the direction (blue is away & red towards the probe [BART])
#2 👆BART holds good unless u invert the scale.
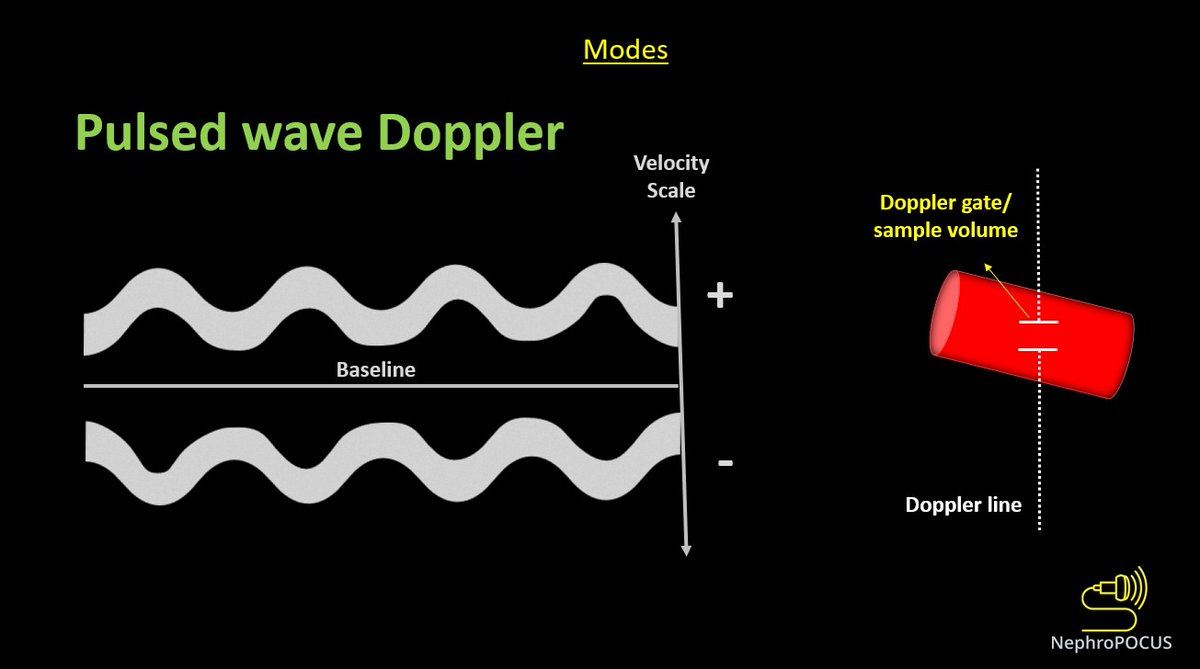
👇Pulsed wave Doppler (PWD) depicts blood flow at a certain point (sample volume) - we analyze the pattern of flow + velocity using this mode.
Above-the-baseline = flow towards the probe (like red on color)
Below = away (like blue)
👇Pulsed wave Doppler (PWD) depicts blood flow at a certain point (sample volume) - we analyze the pattern of flow + velocity using this mode.
Above-the-baseline = flow towards the probe (like red on color)
Below = away (like blue)
#3
While performing any Doppler study, it's important to keep in mind that the angle between US beam & blood flow determines the accuracy of velocity displayed. Parallel = best, perpendicular = worst
As #VExUS does not rely on absolute velocities, its OK not to have perfect angle
While performing any Doppler study, it's important to keep in mind that the angle between US beam & blood flow determines the accuracy of velocity displayed. Parallel = best, perpendicular = worst
As #VExUS does not rely on absolute velocities, its OK not to have perfect angle
#4
Below image explains 👆point. Angle alignment can be performed anatomically i.e., adjusting the ultrasound beam such that the vessel is parallel or near-parallel (as in right side image below).
Can also use 'angle correction' feature when anatomic correction is not possible.
Below image explains 👆point. Angle alignment can be performed anatomically i.e., adjusting the ultrasound beam such that the vessel is parallel or near-parallel (as in right side image below).
Can also use 'angle correction' feature when anatomic correction is not possible.
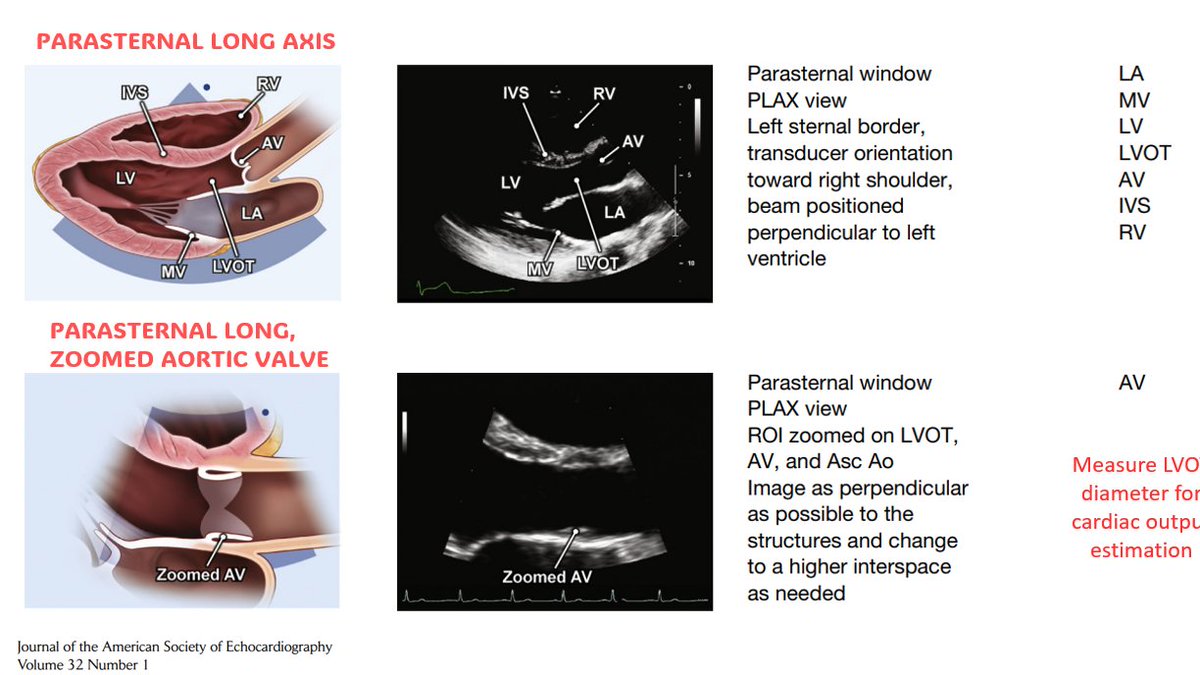
#5
What probe to use?
Either phased array or curvilinear is OK. As most people do cardiac #POCUS first, its reasonable to use the same probe to do #VExUS.
However, pay attention to velocity scale & adjust accordingly. For example, in cardiac preset,
What probe to use?
Either phased array or curvilinear is OK. As most people do cardiac #POCUS first, its reasonable to use the same probe to do #VExUS.
However, pay attention to velocity scale & adjust accordingly. For example, in cardiac preset,

#6
standard velocity scale tends to be high. May need to ⬇️
Otherwise, curvilinear works well as it's optimized for abdominal applications. Specifically for kidney, color pick up is much better with it.
🚨Reminder: Use EKG when available. Just limb leads - takes 10-15 sec
standard velocity scale tends to be high. May need to ⬇️
Otherwise, curvilinear works well as it's optimized for abdominal applications. Specifically for kidney, color pick up is much better with it.
🚨Reminder: Use EKG when available. Just limb leads - takes 10-15 sec
#7
Know your #anatomy
#POCUS = #anatomy + common sense
Hepatic and portal veins (HV, PV respectively) can be visualized either from the lateral window or the subxiphoid window. Details below.
Know your #anatomy
#POCUS = #anatomy + common sense
Hepatic and portal veins (HV, PV respectively) can be visualized either from the lateral window or the subxiphoid window. Details below.

#8
From the mid to posterior axillary line (right upper quadrant), this is the anatomic orientation of the HV, IVC and aorta.
As you know, structures closer to the probe are displayed on top of the image.
Yellow arrow = probe marker orientation (superior, slightly posterior)
From the mid to posterior axillary line (right upper quadrant), this is the anatomic orientation of the HV, IVC and aorta.
As you know, structures closer to the probe are displayed on top of the image.
Yellow arrow = probe marker orientation (superior, slightly posterior)
#9
On fanning the probe anteriorly (from IVC/HV view above), portal vein comes into view. This is how it looks like 👇
On fanning the probe anteriorly (from IVC/HV view above), portal vein comes into view. This is how it looks like 👇

#10
To summarize, anterior fanning brings PV into view and posterior fanning demonstrates HV from the same sonographic window.
To summarize, anterior fanning brings PV into view and posterior fanning demonstrates HV from the same sonographic window.
#11
With slight probe rotation, we might be able to catch both HV and PV from the lateral window. IVC is also seen 👇though may not represent accurate size.
With slight probe rotation, we might be able to catch both HV and PV from the lateral window. IVC is also seen 👇though may not represent accurate size.
#12
Transverse view of the IVC, HV, PV from the lateral window. Probe orientation marker is to the right (left is OK as long as you don't confuse the anatomy/US preset). PV has thick walls where as HVs have imperceptible walls.
HVs go toward the IVC, PV goes into the liver.
Transverse view of the IVC, HV, PV from the lateral window. Probe orientation marker is to the right (left is OK as long as you don't confuse the anatomy/US preset). PV has thick walls where as HVs have imperceptible walls.
HVs go toward the IVC, PV goes into the liver.
#13
Now coming to the subxiphoid window. #POCUS users performing IVC ultrasound are very familiar with this window.
Here👇long axis view of the IVC is demonstrated along with HV. Probe orientation marker is towards patient's head.
Now coming to the subxiphoid window. #POCUS users performing IVC ultrasound are very familiar with this window.
Here👇long axis view of the IVC is demonstrated along with HV. Probe orientation marker is towards patient's head.
#14
Do not confuse aorta with IVC. Fanning from the midline to right, you can see aorta, IVC and portal vein.
Do not confuse aorta with IVC. Fanning from the midline to right, you can see aorta, IVC and portal vein.
#16
If you rotate the probe 90 degrees from the long axis view of the IVC, can visualize it in short axis. Hepatic veins are seen joining the IVC.
There are 3 main HVs - right, middle and the left. Middle and left veins often fuse before joining the IVC.
If you rotate the probe 90 degrees from the long axis view of the IVC, can visualize it in short axis. Hepatic veins are seen joining the IVC.
There are 3 main HVs - right, middle and the left. Middle and left veins often fuse before joining the IVC.
#17
In the subxiphoid transverse view, fanning superiorly brings HVs into view and fanning inferiorly demonstrates PV.
In the subxiphoid transverse view, fanning superiorly brings HVs into view and fanning inferiorly demonstrates PV.
#18
Normal HV and PV #VExUS waveforms
Normal HV and PV #VExUS waveforms
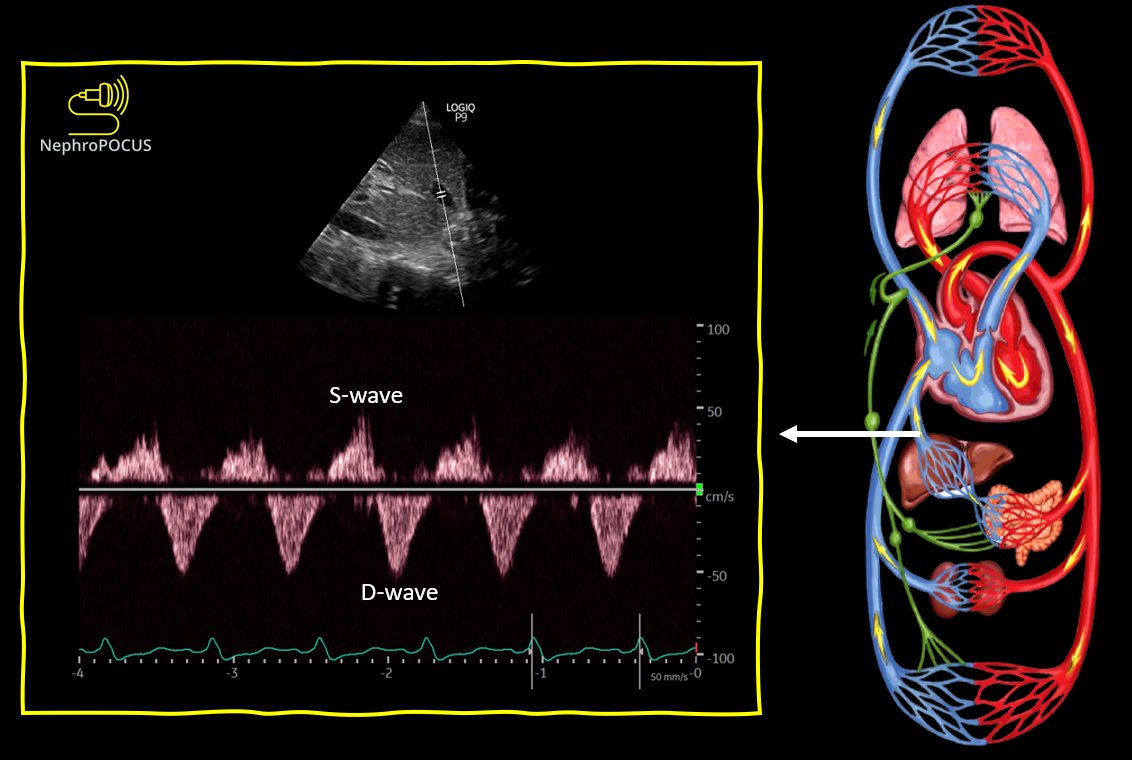
#19
I mentioned the scale before.
If it is set too high 👇, the waveform will appear small - difficult to properly interpret.
I mentioned the scale before.
If it is set too high 👇, the waveform will appear small - difficult to properly interpret.
#20
Even when evaluating using color Doppler, scale is important. Too high scale -> scanty color -> may falsely diagnose vessel thrombosis (e.g. PV thrombosis in a patient with cirrhosis).
Even when evaluating using color Doppler, scale is important. Too high scale -> scanty color -> may falsely diagnose vessel thrombosis (e.g. PV thrombosis in a patient with cirrhosis).
#21
PWD scale set too low -> results in aliasing (as you see here, peaks of the waves are being chopped off and displayed above the baseline).
To avoid aliasing, simply increase the scale or move the baseline up.
PWD scale set too low -> results in aliasing (as you see here, peaks of the waves are being chopped off and displayed above the baseline).
To avoid aliasing, simply increase the scale or move the baseline up.
#22
Remember we talked about the angle in the beginning?
I said don't worry too much even if the angle is not parallel because we are not relying on absolute velocities. It's true but its better to aim for a good angle when possible - waveforms will be better interpretable👇
Remember we talked about the angle in the beginning?
I said don't worry too much even if the angle is not parallel because we are not relying on absolute velocities. It's true but its better to aim for a good angle when possible - waveforms will be better interpretable👇
#23
If the patient is able to cooperate, ask them to hold the breath in end-expiration -> easier to acquire the images when the vessels are not moving.
Note that valsalva maneuver must be avoided (sometimes happens inadvertently). See how the HV became blunted here 👇
If the patient is able to cooperate, ask them to hold the breath in end-expiration -> easier to acquire the images when the vessels are not moving.
Note that valsalva maneuver must be avoided (sometimes happens inadvertently). See how the HV became blunted here 👇
#24
We frequently say lateral view gives better waveforms. Here is an example.
Below images show HV and PV from the same subject (nice crisp waveforms above) obtained from the subxiphoid view. They are OK but look noisy/blurry (possibly due to small tributaries/branches here).
We frequently say lateral view gives better waveforms. Here is an example.
Below images show HV and PV from the same subject (nice crisp waveforms above) obtained from the subxiphoid view. They are OK but look noisy/blurry (possibly due to small tributaries/branches here).
#25
Finally renal interlobar veins. Most of us know how to find the kidneys. Just go slightly posterior in the RUQ approximately at the junction of subxiphoid line and posterior axillary line.
Interlobar vessels are just adjacent to the medullary pyramids (nice B-flow image 👇)
Finally renal interlobar veins. Most of us know how to find the kidneys. Just go slightly posterior in the RUQ approximately at the junction of subxiphoid line and posterior axillary line.
Interlobar vessels are just adjacent to the medullary pyramids (nice B-flow image 👇)
#26
It's no secret that intra-renal Doppler is tough compared to the rest, especially in critically ill patients.
But in most pts (70-80% in my experience), its possible to get interpretable waveforms.
Use Power Doppler to identify the vessels if available - identifies low flow.
It's no secret that intra-renal Doppler is tough compared to the rest, especially in critically ill patients.
But in most pts (70-80% in my experience), its possible to get interpretable waveforms.
Use Power Doppler to identify the vessels if available - identifies low flow.
#27
Normal intra-renal vessel waveform👇: arterial above the baseline and venous below.
Its interpretable if you manage to get 2-3 consecutive cardiac cycles. Just make sure you are not interpreting loss of signal (due to PWD gate movement) as discontinuous venous flow.
Normal intra-renal vessel waveform👇: arterial above the baseline and venous below.
Its interpretable if you manage to get 2-3 consecutive cardiac cycles. Just make sure you are not interpreting loss of signal (due to PWD gate movement) as discontinuous venous flow.
#28
That's it for now. I know its a long 🧵but hope its useful, at least for beginners.
Happy scanning!
In the 'Doppler' section of NephroPOCUS.com, you'll find more related posts/flash cards.
That's it for now. I know its a long 🧵but hope its useful, at least for beginners.
Happy scanning!
In the 'Doppler' section of NephroPOCUS.com, you'll find more related posts/flash cards.
• • •
Missing some Tweet in this thread? You can try to
force a refresh