David Ledgerwood talks about a pharmacist delivered contingency management in people with HIV who smoke - and of course I am super excited to see #pharmacists deliver these interventions #cpdd22 1/ 

2/ can pharmacists be trained to deliver contingency management for smoking cessation?
3/ yes! Of course they can. Pharmacists do really well in terms of delivering contingency management, especially discussing smoking and praising efforts and being generally skilful in smoking cessation 


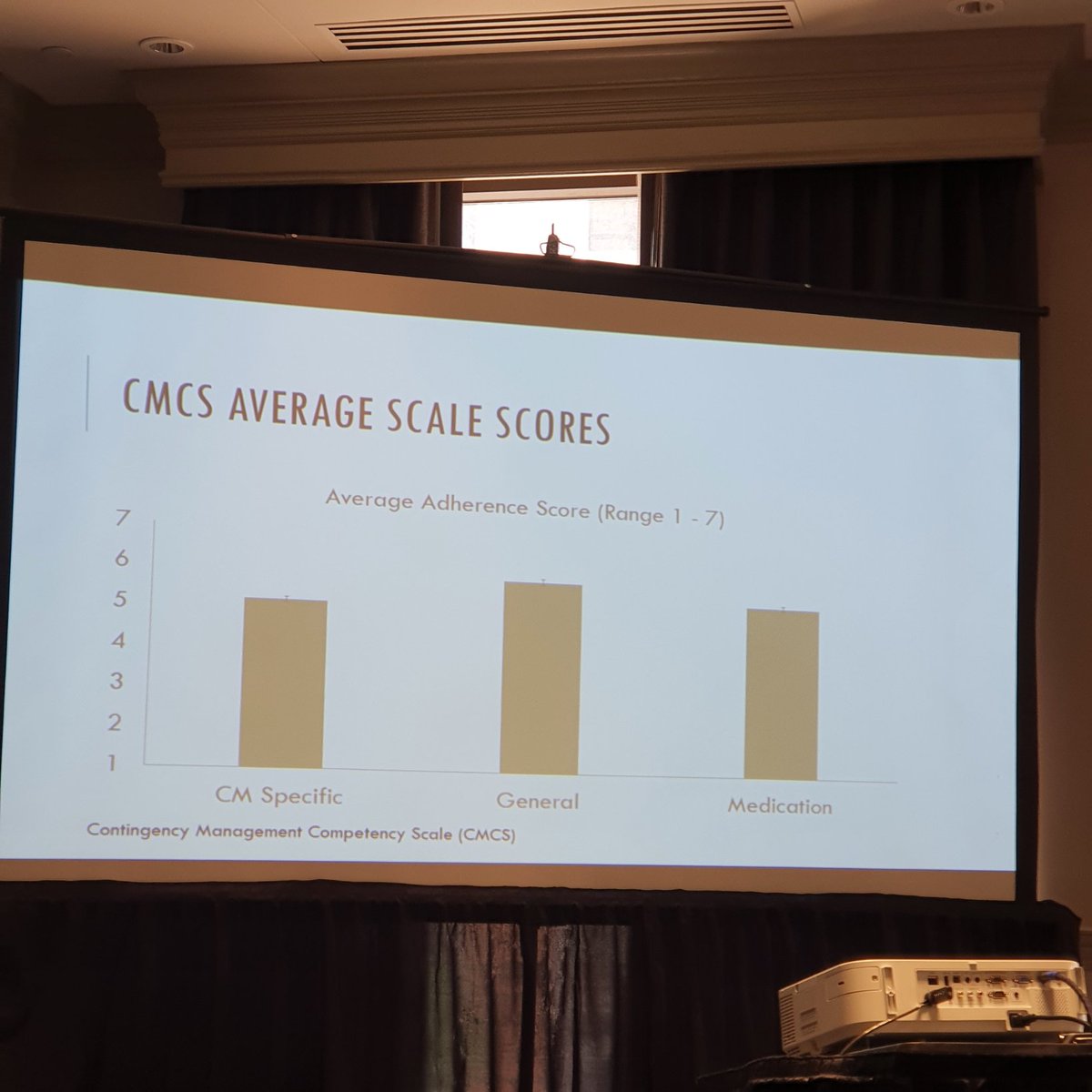
4/ pharmacist seemed less likely to assess contingency management prize interest or discussing prize draws... this may be a less familiar part of pharmacy practice 



• • •
Missing some Tweet in this thread? You can try to
force a refresh